Cancer Res Treat.
2020 Apr;52(2):516-523. 10.4143/crt.2019.328.
Pretreatment Lymph Node Metastasis as a Prognostic Significance inCervical Cancer: Comparison between Disease Status
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2500336
- DOI: http://doi.org/10.4143/crt.2019.328
Abstract
- Purpose
Lymph node metastasis (LNM) is the most significant prognostic factor in cervical cancer that was recently incorporated into the International Federation of Gynecology and Obstetrics (FIGO) staging system. This study was performed to evaluate whether the prognostic significance of LNM differs according to disease status.
Materials and Methods
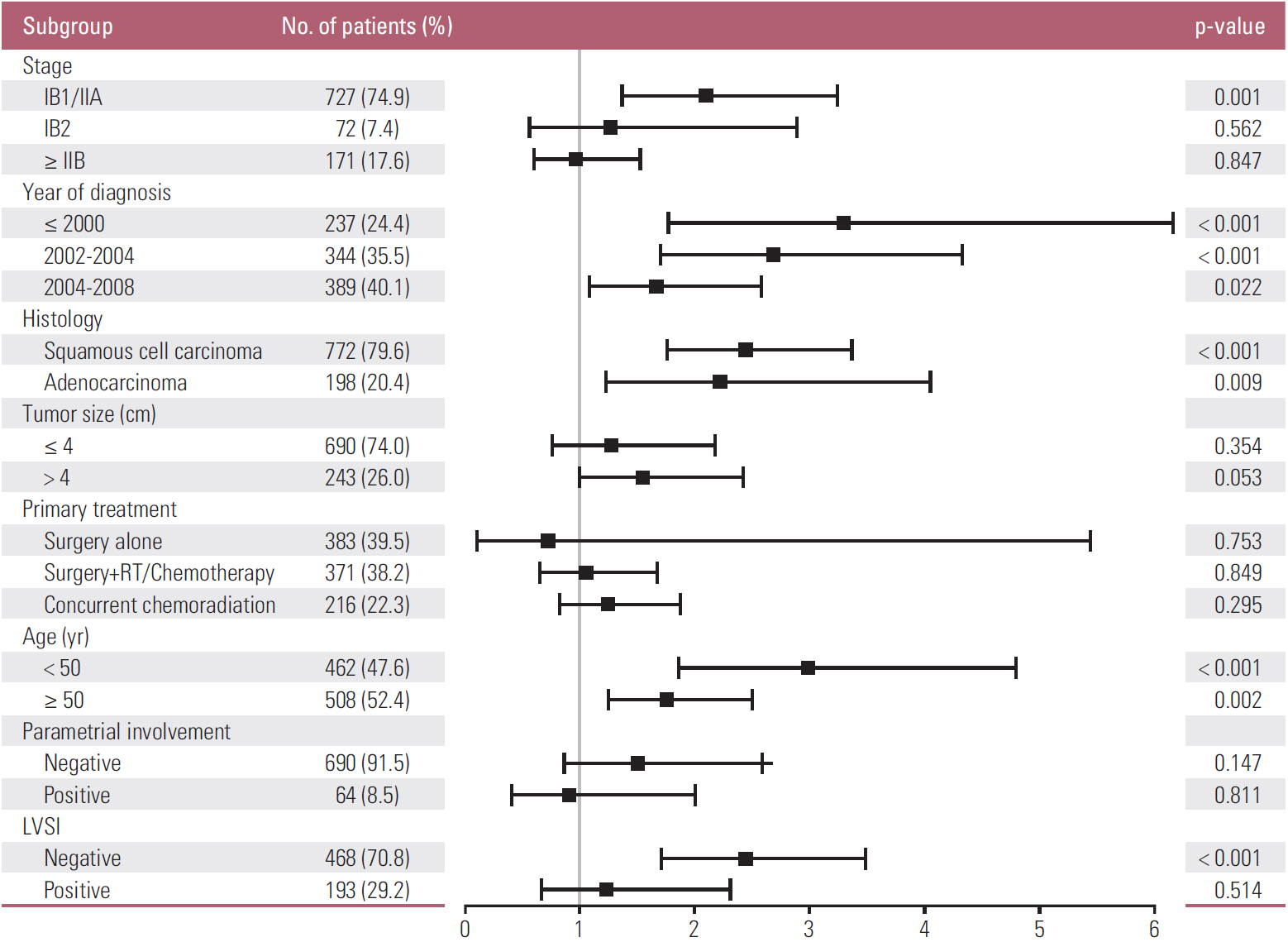
Patients with FIGO stage IB or higher cervical cancer who had pretreatment computed tomography and/or magnetic resonance imaging studies as well as long-term follow-up were enrolled in this retrospective study. The hazard ratio (HR) of Cox regression was used to determine the prognostic significance of LNM. The HRs were compared between the different tumor groups (based on stage, histology, tumor size, primary treatment, age, parametrium involvement, and lymphovascular space invasion).
Results
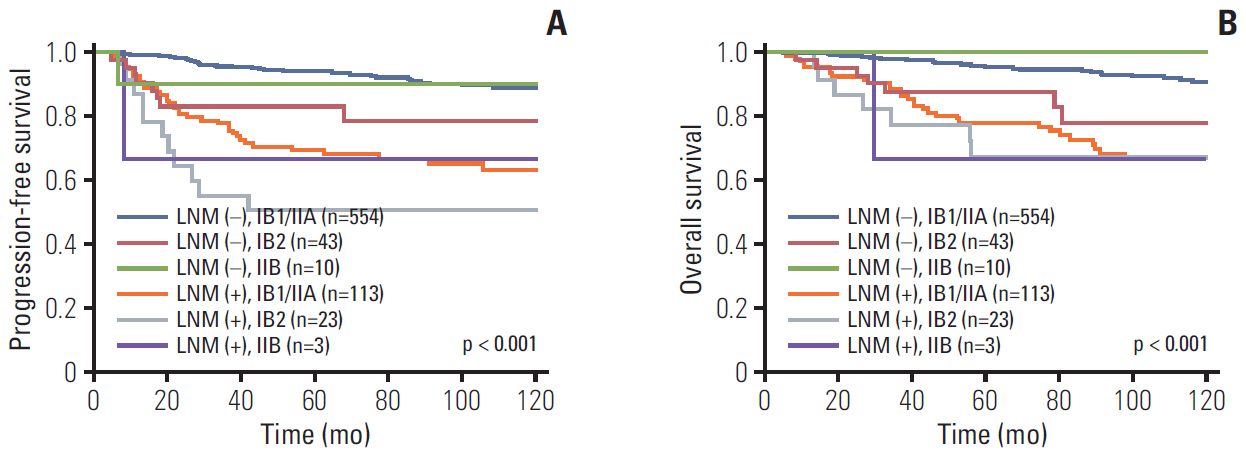
A total of 970 patients treated between January 1999 and December 2007 were included. The pretreatment LNM had prognostic significance in patients with stage IB1/IIA (HR for progression-free survival 2.10, p=0.001; HR for overall survival 1.99, p=0.005). However, the significance gradually decreased or disappeared with advancing stages. Similarly, the prognostic significance of the pretreatment LNM decreased with advancing disease status, including old age, parametrial involvement or lymphovascular space involvement. In contrast, the tumor size was associated with the prognostic significance of LNM with advancing status. The significance of the clinical LNM did not reflect the significance of the clinical stage. In contrast, the tumor size, parametrial involvement, and significance of the pathologic LNM reflected the clinical stage.
Conclusion
In patients with cervical cancer, pretreatment LNM on imaging has different clinical significance depending on the tumor status.
Keyword
Figure
Reference
-
References
1. Jung KW, Won YJ, Kong HJ, Lee ES. Prediction of cancer incidence and mortality in Korea, 2019. Cancer Res Treat. 2019; 51:431–7.
Article2. Pecorelli S, Zigliani L, Odicino F. Revised FIGO staging for carcinoma of the cervix. Int J Gynaecol Obstet. 2009; 105:107–8.
Article3. Lagasse LD, Creasman WT, Shingleton HM, Ford JH, Blessing JA. Results and complications of operative staging in cervical cancer: experience of the Gynecologic Oncology Group. Gynecol Oncol. 1980; 9:90–8.
Article4. Creasman WT, Kohler MF. Is lymph vascular space involvement an independent prognostic factor in early cervical cancer? Gynecol Oncol. 2004; 92:525–9.
Article5. Liu B, Gao S, Li S. A comprehensive comparison of CT, MRI, positron emission tomography or positron emission tomography/CT, and diffusion weighted imaging-MRI for detecting the lymph nodes metastases in patients with cervical cancer: a meta-analysis based on 67 studies. Gynecol Obstet Invest. 2017; 82:209–22.
Article6. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65:87–108.
Article7. Scheidler J, Hricak H, Yu KK, Subak L, Segal MR. Radiological evaluation of lymph node metastases in patients with cervical cancer: a meta-analysis. JAMA. 1997; 278:1096–101.
Article8. LaPolla JP, Schlaerth JB, Gaddis O, Morrow CP. The influence of surgical staging on the evaluation and treatment of patients with cervical carcinoma. Gynecol Oncol. 1986; 24:194–206.
Article9. Hricak H, Gatsonis C, Chi DS, Amendola MA, Brandt K, Schwartz LH, et al. Role of imaging in pretreatment evaluation of early invasive cervical cancer: results of the intergroup study American College of Radiology Imaging Network 6651-Gynecologic Oncology Group 183. J Clin Oncol. 2005; 23:9329–37.
Article10. Thomeer MG, Gerestein C, Spronk S, van Doorn HC, van der Ham E, Hunink MG. Clinical examination versus magnetic resonance imaging in the pretreatment staging of cervical carcinoma: systematic review and meta-analysis. Eur Radiol. 2013; 23:2005–18.
Article11. Sala E, Micco M, Burger IA, Yakar D, Kollmeier MA, Goldman DA, et al. Complementary prognostic value of pelvic magnetic resonance imaging and whole-body fluorodeoxyglucose positron emission tomography/computed tomography in the pretreatment assessment of patients with cervical cancer. Int J Gynecol Cancer. 2015; 25:1461–7.
Article12. Shim SH, Lee SW, Park JY, Kim YS, Kim DY, Kim JH, et al. Risk assessment model for overall survival in patients with locally advanced cervical cancer treated with definitive concurrent chemoradiotherapy. Gynecol Oncol. 2013; 128:54–9.
Article13. Kang S, Nam BH, Park JY, Seo SS, Ryu SY, Kim JW, et al. Risk assessment tool for distant recurrence after platinum-based concurrent chemoradiation in patients with locally advanced cervical cancer: a Korean gynecologic oncology group study. J Clin Oncol. 2012; 30:2369–74.
Article14. Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R. Cancer of the cervix uteri. Int J Gynaecol Obstet. 2018; 143 Suppl 2:22–36.
Article15. Lai CH, Yen TC, Ng KK. Surgical and radiologic staging of cervical cancer. Curr Opin Obstet Gynecol. 2010; 22:15–20.
Article16. Wu SY, Huang EY, Chanchien CC, Lin H, Wang CJ, Sun LM, et al. Prognostic factors associated with radiotherapy for cervical cancer with computed tomography-detected para-aortic lymph node metastasis. J Radiat Res. 2014; 55:129–38.
Article17. Sakuragi N. Up-to-date management of lymph node metastasis and the role of tailored lymphadenectomy in cervical cancer. Int J Clin Oncol. 2007; 12:165–75.
Article18. Mitchell DG, Snyder B, Coakley F, Reinhold C, Thomas G, Amendola MA, et al. Early invasive cervical cancer: MRI and CT predictors of lymphatic metastases in the ACRIN 6651/GOG 183 intergroup study. Gynecol Oncol. 2009; 112:95–103.
Article19. Hori M, Kim T, Murakami T, Imaoka I, Onishi H, Tomoda K, et al. Uterine cervical carcinoma: preoperative staging with 3.0-T MR imaging: comparison with 1.5-T MR imaging. Radiology. 2009; 251:96–104.20. Shen G, Zhou H, Jia Z, Deng H. Diagnostic performance of diffusion-weighted MRI for detection of pelvic metastatic lymph nodes in patients with cervical cancer: a systematic review and meta-analysis. Br J Radiol. 2015; 88:20150063.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Implications of Lymph Node Metastasis in Colorectal Cancer: Current Status and Future Perspectives
- Lymph Node Metastasis in a Gynecologic Malignancy
- Significance of Lymph Node Metastasis in Early Gastric Cancer
- Ratio of Involved Lymph Nodes to Resected Lymph Nodesas a Prognostic Factor of Gastric Cancer
- Clninical Utility of Serum Squamous Cell Carcinoma Antigen and Urine Polyamines in Cervical Carcinoma