Obstet Gynecol Sci.
2020 Mar;63(2):158-163. 10.5468/ogs.2020.63.2.158.
Prognostic value of lymph node ratio in surgically treated cases of vulvar cancer: a tertiary care centre experience
- Affiliations
-
- 1Department of Gynecological Oncology, Gujarat Cancer & Research Institute, Ahmedabad, India. drshilpamukesh@gmail.com
- KMID: 2471753
- DOI: http://doi.org/10.5468/ogs.2020.63.2.158
Abstract
OBJECTIVE
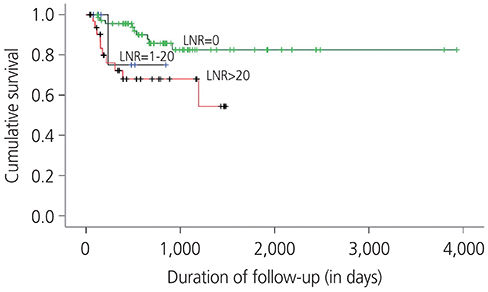
This study aimed to study the patterns of recurrence in surgically treated cases of vulvar cancer (VC) and determine the factors associated with recurrence, with a special emphasis on lymph node ratio (LNR).
METHODS
This retrospective study examined VC patients primarily treated with surgery at our institute from January 2005 to December 2015. Demographic data, clinical characteristics, surgicohistopathological data, adjuvant treatment, follow up, and recurrence site and treatment were studied.
RESULTS
Among the 111 cases treated, a recurrence rate of 18.9% was noted. Recurrence was most commonly local (61.9%). On univariate and multivariable analyses of clinicopathological parameters, an LNR >20 had the highest hazard ratio for recurrence.
CONCLUSION
LNR may provide useful prognostic information in VC patients with positive inguinal lymph node status.
Keyword
MeSH Terms
Figure
Reference
-
1. de Martel C, Ferlay J, Franceschi S, Vignat J, Bray F, Forman D, et al. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol. 2012; 13:607–615.
Article2. Akerman G, Dussour C, Haddad B, Paniel BJ, Rouzier R. Epidemiology of vulvar intra-epithelial neoplasias. Gynecol Obstet Fertil. 2007; 35:1251–1256.3. Raspagliesi F, Hanozet F, Ditto A, Solima E, Zanaboni F, Vecchione F, et al. Clinical and pathological prognostic factors in squamous cell carcinoma of the vulva. Gynecol Oncol. 2006; 102:333–337.
Article4. Hopkins MP, Reid GC, Vettrano I, Morley GW. Squamous cell carcinoma of the vulva: prognostic factors influencing survival. Gynecol Oncol. 1991; 43:113–117.
Article5. Iacoponi S, Zapardiel I, Diestro MD, Hernandez A, De Santiago J. Prognostic factors associated with local recurrence in squamous cell carcinoma of the vulva. J Gynecol Oncol. 2013; 24:242–248.
Article6. Kunos C, Simpkins F, Gibbons H, Tian C, Homesley H. Radiation therapy compared with pelvic node resection for node-positive vulvar cancer: a randomized controlled trial. Obstet Gynecol. 2009; 114:537–546.
Article9. Stehman FB, Bundy BN, Ball H, Clarke-Pearson DL. Sites of failure and times to failure in carcinoma of the vulva treated conservatively: a Gynecologic Oncology Group study. Am J Obstet Gynecol. 1996; 174:1128–1132.
Article7. Bogani G, Cromi A, Serati M, Uccella S, Donato VD, Casarin J, et al. Predictors and patterns of local, regional, and distant failure in squamous cellcarcinoma of the vulva. Am J Clin Oncol. 2017; 40:235–240.8. Cormio G, Loizzi V, Carriero C, Cazzolla A, Putignano G, Selvaggi L. Groin recurrence in carcinoma of the vulva: management and outcome. Eur J Cancer Care (Engl). 2010; 19:302–307.
Article10. Gonzalez Bosquet J, Magrina JF, Gaffey TA, Hernandez JL, Webb MJ, Cliby WA, et al. Long-term survival and disease recurrence in patients with primary squamous cell carcinoma of the vulva. Gynecol Oncol. 2005; 97:828–833.
Article11. Maggino T, Landoni F, Sartori E, Zola P, Gadducci A, Alessi C, et al. Patterns of recurrence in patients with squamous cell carcinoma of the vulva. A multicenter CTF study. Cancer. 2000; 89:116–122.12. Piura B, Masotina A, Murdoch J, Lopes A, Morgan P, Monaghan J. Recurrent squamous cell carcinoma of the vulva: a study of 73 cases. Gynecol Oncol. 1993; 48:189–195.
Article13. Van Beekhuizen HJ, Auzin M, van den Einden LC, de Hullu JA, van der Velden J, Wildhagen MF, et al. Lymph node count at inguinofemoral lymphadenectomy and groin recurrences in vulvar cancer. Int J Gynecol Cancer. 2014; 24:773–778.
Article14. Heaps JM, Fu YS, Montz FJ, Hacker NF, Berek JS. Surgical-pathologic variables predictive of local recurrence in squamous cell carcinoma of the vulva. Gynecol Oncol. 1990; 38:309–314.
Article15. De Hullu JA, Hollema H, Lolkema S, Boezen M, Boonstra H, Burger MP, et al. Vulvar carcinoma. The price of less radical surgery. Cancer. 2002; 95:2331–2338.16. Mahner S, Jueckstock J, Hilpert F, Neuser P, Harter P, de Gregorio N, et al. Adjuvant therapy in lymph node-positive vulvar cancer: the AGO-CaRE-1 study. J Natl Cancer Inst. 2015; 107:dju426.
Article17. Woelber L, Eulenburg C, Choschzick M, Kruell A, Petersen C, Gieseking F, et al. Prognostic role of lymph node metastases in vulvar cancer and implications for adjuvant treatment. Int J Gynecol Cancer. 2012; 22:503–508.
Article18. Polterauer S, Schwameis R, Grimm C, Macuks R, Iacoponi S, Zalewski K, et al. Prognostic value of lymph node ratio and number of positive inguinal nodes in patients with vulvar cancer. Gynecol Oncol. 2017; 147:92–97.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Significance of Sentinel Lymph Node Detection in Vulvar Cancer
- Supraclavicular Lymph Node Excision Biopsy in Patients with Suspected Supraclavicular Lymph Node Metastasis of Lung Cancer: Experience in a Tertiary Hospital
- Ratio of Involved Lymph Nodes to Resected Lymph Nodesas a Prognostic Factor of Gastric Cancer
- Prognostic value of the lymph node metastasis in patients with ampulla of Vater cancer after surgical resection
- Clinical Implications of Lymph Node Metastasis in Colorectal Cancer: Current Status and Future Perspectives