Ann Hepatobiliary Pancreat Surg.
2021 Feb;25(1):90-96. 10.14701/ahbps.2021.25.1.90.
Prognostic value of the lymph node metastasis in patients with ampulla of Vater cancer after surgical resection
- Affiliations
-
- 1Department of Surgery, Korea University College of Medicine, Seoul, Korea
- KMID: 2513181
- DOI: http://doi.org/10.14701/ahbps.2021.25.1.90
Abstract
- Backgrounds/Aims
Patients with Ampulla of Vater cancer have a better prognosis than those with other periampullary cancers. This study aimed to determine the prognostic impact of lymph node metastasis on survival in patients with ampulla of Vater cancer after surgical resection.
Methods
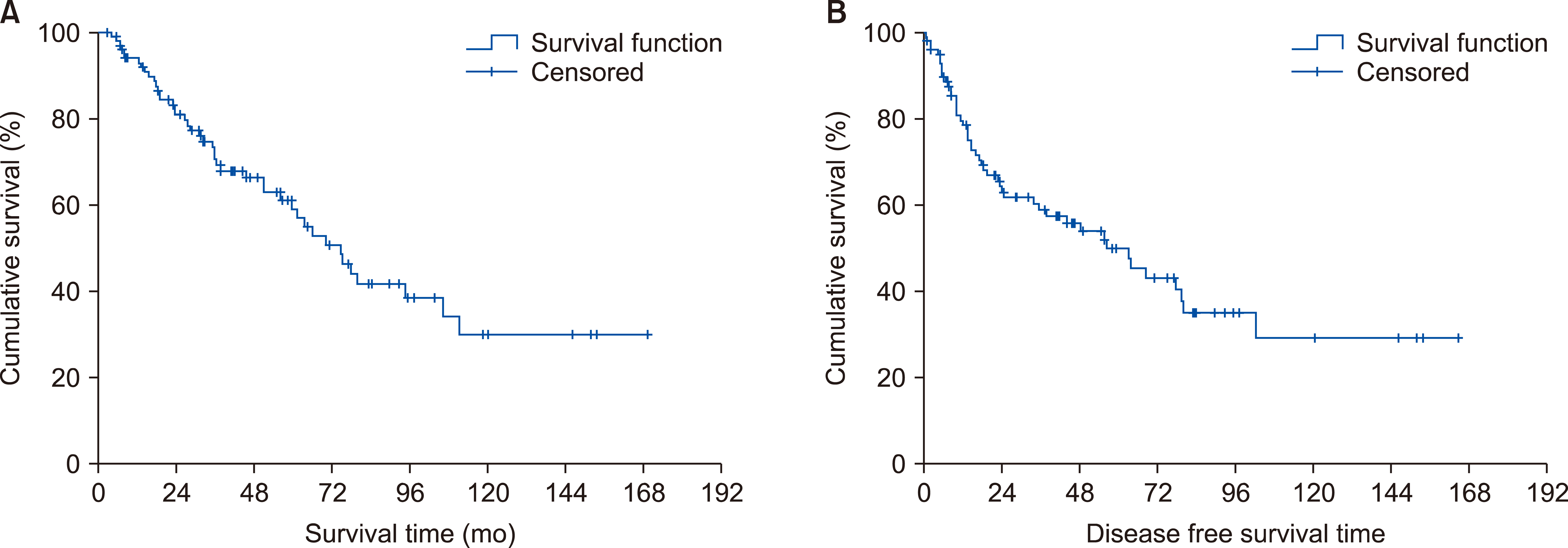
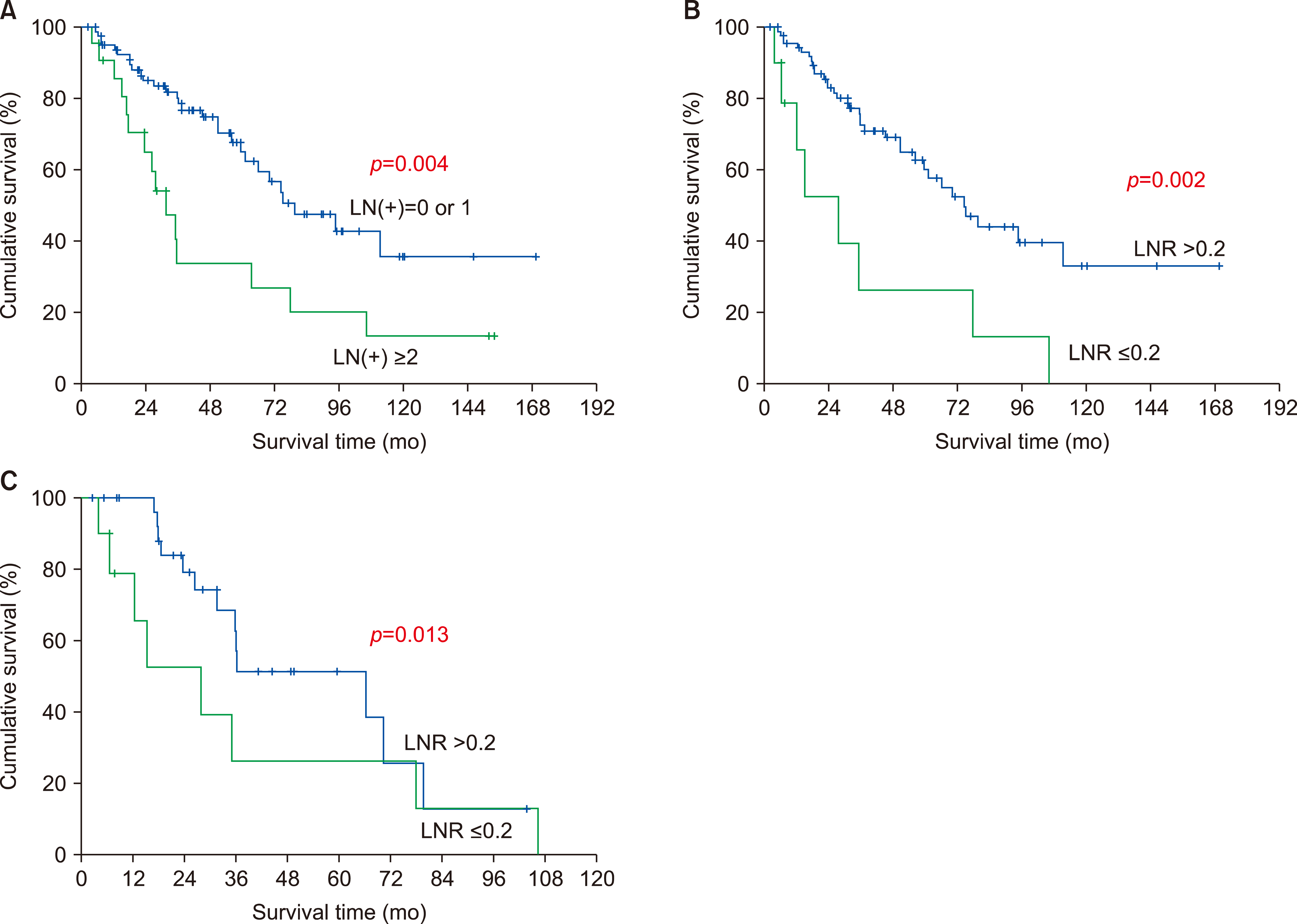
From 1991 to 2016, we retrospectively reviewed data on 104 patients with ampulla of Vater cancer who had received pancreaticoduodenectomy. Clinicopathologic factors such as lymph node ratio (LNR) and number of metastatic lymph nodes that influence survival were statistically analyzed.
Results
5-year survival rate after resection was 57.8%. Mean number of retrieved and metastatic lymph nodes was 13 and 0.95, respectively. In patients with lymph node metastasis, the median number of metastatic lymph nodes and was 1, and the mean LNR was 0.18. LNR >0.2 was a significant prognostic factor for overall survival. Patients with 0 or 1 metastatic lymph nodes had better survival than those with ≥2 metastatic lymph nodes. Univariate analysis revealed that histologic differentiation of tumor, lymph node metastasis, and T stage were significant prognostic factors for overall survival. Multivariate analysis revealed that tumor differentiation and number of metastatic lymph nodes were independent prognostic factors for survival.
Conclusions
Pancreaticoduodenectomy is an appropriate surgical procedure with acceptable long-term survival for ampulla of Vater cancer. Patients with LNR >0.2 and ≥2 positive lymph node metastasis had a poor survival. Tumor differentiation and ≥2 metastatic lymph nodes were independent significant prognostic factors for overall survival. Curative resection with lymph node dissection might control lymph node spread and enhance survival outcomes.
Figure
Reference
-
1. Howe JR, Klimstra DS, Moccia RD, Conlon KC, Brennan MF. 1998; Factors predictive of survival in ampullary carcinoma. Ann Surg. 228:87–94. DOI: 10.1097/00000658-199807000-00013. PMID: 9671071. PMCID: PMC1191432.
Article2. Carter JT, Grenert JP, Rubenstein L, Stewart L, Way LW. 2008; Tumors of the ampulla of vater: histopathologic classification and predictors of survival. J Am Coll Surg. 207:210–218. DOI: 10.1016/j.jamcollsurg.2008.01.028. PMID: 18656049.
Article3. Lazaryan A, Kalmadi S, Almhanna K, Pelley R, Kim R. 2011; Predictors of clinical outcomes of resected ampullary adenocarcinoma: a single-institution experience. Eur J Surg Oncol. 37:791–797. DOI: 10.1016/j.ejso.2011.06.008. PMID: 21741199.
Article4. Kiriyama M, Ebata T, Aoba T, Kaneoka Y, Arai T, Shimizu Y, et al. 2015; Prognostic impact of lymph node metastasis in distal cholangiocarcinoma. Br J Surg. 102:399–406. DOI: 10.1002/bjs.9752. PMID: 25611179.5. Kang HJ, Eo SH, Kim SC, Park KM, Lee YJ, Lee SK, et al. 2014; Increased number of metastatic lymph nodes in adenocarcinoma of the ampulla of Vater as a prognostic factor: a proposal of new nodal classification. Surgery. 155:74–84. DOI: 10.1016/j.surg.2013.08.004. PMID: 24238122.
Article6. Amin MB, Edge S, Greene F, Byrd DR Byrd, Brookland RK, Washington MK, et al. 2017. AJCC cancer staging manual. 8th ed. Springer;New York: DOI: 10.1007/978-3-319-40618-3.7. Pawlik TM, Gleisner AL, Cameron JL, Winter JM, Assumpcao L, Lillemoe KD, et al. 2007; Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery. 141:610–618. DOI: 10.1016/j.surg.2006.12.013. PMID: 17462460.
Article8. Kwon J, Kim K, Chie EK, Kim BH, Jang JY, Kim SW, et al. 2017; Prognostic relevance of lymph node status for patients with ampullary adenocarcinoma after radical resection followed by adjuvant treatment. Eur J Surg Oncol. 43:1690–1696. DOI: 10.1016/j.ejso.2017.05.024. PMID: 28648977.
Article9. Malleo G, Maggino L, Capelli P, Gulino F, Segattini S, Scarpa A, et al. 2015; Reappraisal of nodal staging and study of lymph node station involvement in pancreaticoduodenectomy with the standard International Study Group of Pancreatic Surgery definition of lymphadenectomy for cancer. J Am Coll Surg. 221:367–379. e4. DOI: 10.1016/j.jamcollsurg.2015.02.019. PMID: 26081176.
Article10. Robinson SM, Rahman A, Haugk B, French JJ, Manas DM, Jaques BC, et al. 2012; Metastatic lymph node ratio as an important prognostic factor in pancreatic ductal adenocarcinoma. Eur J Surg Oncol. 38:333–339. DOI: 10.1016/j.ejso.2011.12.020. PMID: 22317758.
Article11. Kim HJ, Kim CY, Hur YH, Koh YS, Kim JC, Kim HJ, et al. 2014; Prognostic factors for survival after curative resection of distal cholangiocarcinoma: perineural invasion and lymphovascular invasion. Surg Today. 44:1879–1886. DOI: 10.1007/s00595-014-0846-z. PMID: 24535697.12. Choi SB, Park SW, Kim KS, Choi JS, Lee WJ. 2009; The survival outcome and prognostic factors for middle and distal bile duct cancer following surgical resection. J Surg Oncol. 99:335–342. DOI: 10.1002/jso.21238. PMID: 19226533.
Article13. Hsu CH, Chen TD, Tsai CY, Hsu JT, Yeh CN, Jan YY, et al. 2015; Prognostic value of the metastatic lymph node ratio in patients with resectable carcinoma of ampulla of Vater. Medicine (Baltimore). 94:e1859. DOI: 10.1097/MD.0000000000001859. PMID: 26496337. PMCID: PMC4620839.
Article14. Kim WS, Choi DW, Choi SH, Heo JS, You DD, Lee HG. 2012; Clinical significance of pathologic subtype in curatively resected ampulla of vater cancer. J Surg Oncol. 105:266–272. DOI: 10.1002/jso.22090. PMID: 21882202.
Article15. Okano K, Asano E, Kushida Y, Kamada H, Mori H, Suzuki Y. 2014; Factors influencing lymph node metastasis in patients with ampullary adenocarcinoma. Dig Surg. 31:459–467. DOI: 10.1159/000370251. PMID: 25613423.
Article16. Zhou J, Zhang Q, Li P, Shan Y, Zhao D, Cai J. 2013; Prognostic relevance of number and ratio of metastatic lymph nodes in resected carcinoma of the ampulla of Vater. Chin J Cancer Res. 25:735–742. DOI: 10.3978/j.issn.1000-9604.2013.12.03. PMID: 24385702. PMCID: PMC3872556.17. Kayahara M, Ohta T. 2010; Gross appearance of the ampullary tumor predicts lymph node metastasis and outcome. Dig Surg. 27:127–131. DOI: 10.1159/000286839. PMID: 20551657.
Article18. Balci S, Basturk O, Saka B, Bagci P, Postlewait LM, Tajiri T, et al. 2015; Substaging nodal status in ampullary carcinomas has significant prognostic value: proposed revised staging based on an analysis of 313 well-characterized cases. Ann Surg Oncol. 22:4392–4401. DOI: 10.1245/s10434-015-4499-y. PMID: 25783680. PMCID: PMC4575255.
Article19. Sakata J, Shirai Y, Wakai T, Ajioka Y, Akazawa K, Hatakeyama K. 2011; Assessment of the nodal status in ampullary carcinoma: the number of positive lymph nodes versus the lymph node ratio. World J Surg. 35:2118–2124. DOI: 10.1007/s00268-011-1175-7. PMID: 21717240.
Article20. Jiang C, Wang F, Guo G, Dong J, Liu S, He W, et al. 2019; Metastatic lymph node ratio as a prognostic indicator in patients with stage IV colon cancer undergoing resection. J Cancer. 10:2534–2540. DOI: 10.7150/jca.29216. PMID: 31258759. PMCID: PMC6584347.
Article21. Kutlu OC, Watchell M, Dissanaike S. 2015; Metastatic lymph node ratio successfully predicts prognosis in western gastric cancer patients. Surg Oncol. 24:84–88. DOI: 10.1016/j.suronc.2015.03.001. PMID: 25912951.
Article22. Roland CL, Katz MH, Gonzalez GM, Pisters PW, Vauthey JN, Wolff RA, et al. 2012; A high positive lymph node ratio is associated with distant recurrence after surgical resection of ampullary carcinoma. J Gastrointest Surg. 16:2056–2063. DOI: 10.1007/s11605-012-2015-2. PMID: 22914983. PMCID: PMC5131719.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ki-67 and VEGF as Possible Prognostic Factors in Radically-resected Ampulla of Vater Cancer
- Prognostic Factors and Survival Rate of Ampulla of Vater Cancer after Curative Surgery
- Prognostic Significance of Angiogenesis by Chalkley Counting in Node Negative Cancer of the Ampulla of Vater
- Recurrence Patterns and Risk Factors of Early Recurrence after Curative Resection of Ampulla of Vater Cancer
- A Case of Signet-ring Cell Carcinoma of the Ampulla of Vater