Epidemiology and Prognosis of Pheochromocytoma/Paraganglioma in Korea: A Nationwide Study Based on the National Health Insurance Service
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Biostatistics, Korea University College of Medicine, Seoul, Korea.
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea.
- 4Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea. k50367@korea.ac.kr
- KMID: 2471732
- DOI: http://doi.org/10.3803/EnM.2020.35.1.157
Abstract
- BACKGROUND
Pheochromocytomas and paragangliomas (PPGLs) are rare endocrine tumors originating from chromaffin cells. PPGLs are associated with a high mortality rate and several complications. To date, no epidemiological studies have been conducted on PPGLs in Asia. This study aimed to investigate the epidemiology and prognosis of PPGLs in Korea using nationwide data.
METHODS
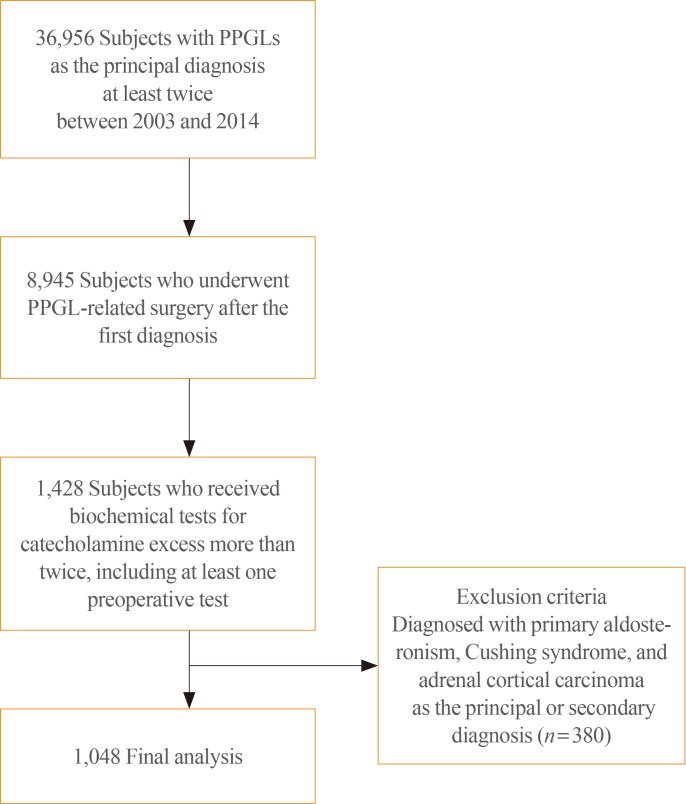
Using the National Health Insurance Service Database, subjects with a principal diagnosis of PPGLs on two or more occasions between 2003 and 2014 who satisfied the operational definition of PPGLs were included. Incidence, prevalence, complications, metastasis, and mortality were investigated.
RESULTS
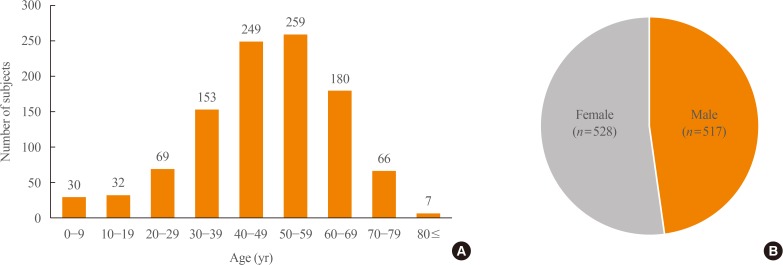
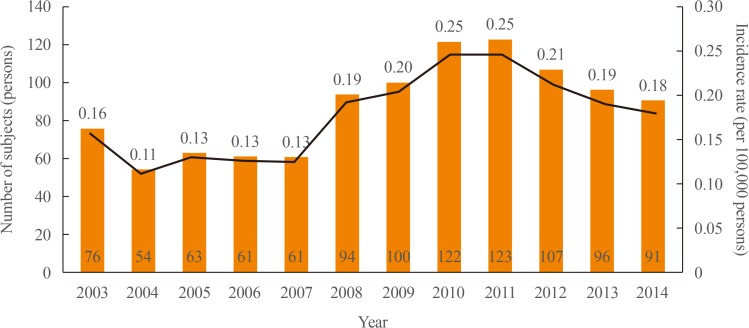
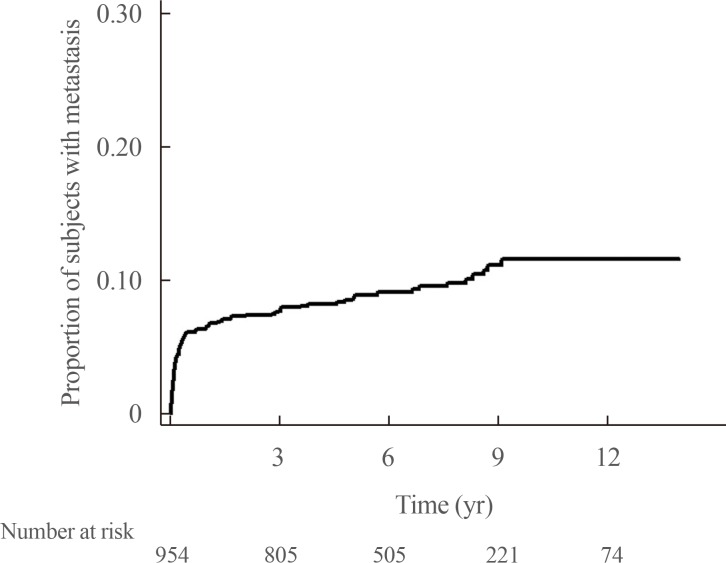
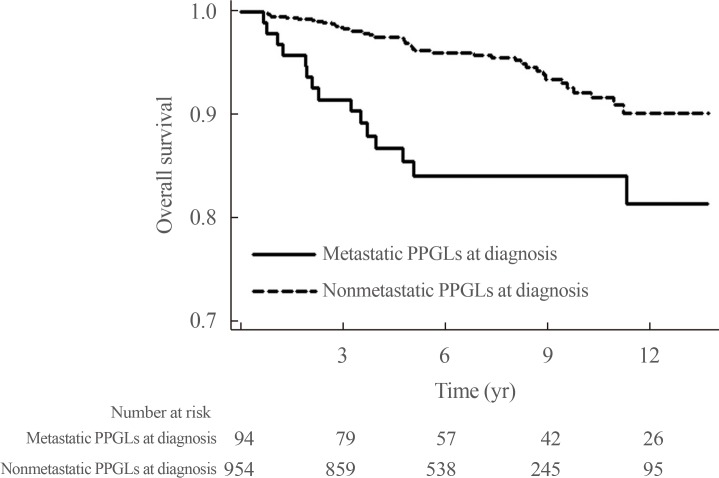
In total, 1048 subjects with a mean age of 47.6±16.1 years were included. There was no sex preponderance. The overall prevalence of PPGLs was 2.13 per 100,000 persons, and the overall age-standardized incidence rate was 0.18 per 100,000 person-years. Malignant PPGLs accounted for 17.7% (185 of 1,048) of cases, and 94 subjects exhibited metastasis at the time of diagnosis. Among initially non-metastatic PPGLs, 9.5% (nine of 954) eventually metastasized after a mean duration of 78.1±41.4 months. The 5-year survival rates for non-metastatic and metastatic PPGLs at diagnosis were 97% and 84%, respectively. Multivariable Cox regression models adjusted for covariates showed that metastatic PPGLs were associated with a 2.40-fold higher risk of mortality than non-metastatic PPGLs (95% confidence interval, 1.38 to 4.17; P=0.002).
CONCLUSION
PPGLs are rare in Korea, and the prognosis of these endocrine tumors varies depending on whether they are benign or malignant. This epidemiological study paves the way for further research on PPGLs.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
A Brief Overview of the Epidemiology of Pheochromocytoma and Paraganglioma in Korea
Yun Mi Choi
Endocrinol Metab. 2020;35(1):95-96. doi: 10.3803/EnM.2020.35.1.95.Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force
Eu Jeong Ku, Kyoung Jin Kim, Jung Hee Kim, Mi Kyung Kim, Chang Ho Ahn, Kyung Ae Lee, Seung Hun Lee, You-Bin Lee, Kyeong Hye Park, Yun Mi Choi, Namki Hong, A Ram Hong, Sang-Wook Kang, Byung Kwan Park, Moon-Woo Seong, Myungshin Kim, Kyeong Cheon Jung, Chan Kwon Jung, Young Seok Cho, Jin Chul Paeng, Jae Hyeon Kim, Ohk-Hyun Ryu, Yumie Rhee, Chong Hwa Kim, Eun Jig Lee
Endocrinol Metab. 2021;36(2):322-338. doi: 10.3803/EnM.2020.908.Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinol Metab. 2023;38(1):10-24. doi: 10.3803/EnM.2023.102.
Reference
-
1. Lenders JWM, Eisenhofer G. Update on modern management of pheochromocytoma and paraganglioma. Endocrinol Metab (Seoul). 2017; 32:152–161. PMID: 28685506.
Article2. Plouin PF, Duclos JM, Soppelsa F, Boublil G, Chatellier G. Factors associated with perioperative morbidity and mortality in patients with pheochromocytoma: analysis of 165 operations at a single center. J Clin Endocrinol Metab. 2001; 86:1480–1486. PMID: 11297571.
Article3. Khorram-Manesh A, Ahlman H, Nilsson O, Oden A, Jansson S. Mortality associated with pheochromocytoma in a large Swedish cohort. Eur J Surg Oncol. 2004; 30:556–559. PMID: 15135486.
Article4. Prejbisz A, Lenders JW, Eisenhofer G, Januszewicz A. Cardiovascular manifestations of phaeochromocytoma. J Hypertens. 2011; 29:2049–2060. PMID: 21826022.
Article5. Zelinka T, Petrak O, Turkova H, Holaj R, Strauch B, Krsek M, et al. High incidence of cardiovascular complications in pheochromocytoma. Horm Metab Res. 2012; 44:379–384. PMID: 22517556.
Article6. Kim KY, Kim JH, Hong AR, Seong MW, Lee KE, Kim SJ, et al. Disentangling of malignancy from benign pheochromocytomas/paragangliomas. PLoS One. 2016; 11:e0168413. PMID: 27992508.
Article7. Plouin PF, Fitzgerald P, Rich T, Ayala-Ramirez M, Perrier ND, Baudin E, et al. Metastatic pheochromocytoma and paraganglioma: focus on therapeutics. Horm Metab Res. 2012; 44:390–399. PMID: 22314389.
Article8. Hong AR, Kim JH, Park KS, Kim KY, Lee JH, Kong SH, et al. Optimal follow-up strategies for adrenal incidentalomas: reappraisal of the 2016 ESE-ENSAT guidelines in real clinical practice. Eur J Endocrinol. 2017; 177:475–483. PMID: 28870984.
Article9. Mantero F, Terzolo M, Arnaldi G, Osella G, Masini AM, Ali A, et al. A survey on adrenal incidentaloma in Italy. Study Group on Adrenal Tumors of the Italian Society of Endocrinology. J Clin Endocrinol Metab. 2000; 85:637–644. PMID: 10690869.10. McNeil AR, Blok BH, Koelmeyer TD, Burke MP, Hilton JM. Phaeochromocytomas discovered during coronial autopsies in Sydney, Melbourne and Auckland. Aust N Z J Med. 2000; 30:648–652. PMID: 11198571.
Article11. Berends AMA, Buitenwerf E, de Krijger RR, Veeger NJGM, van der Horst-Schrivers ANA, Links TP, et al. Incidence of pheochromocytoma and sympathetic paraganglioma in the Netherlands: a nationwide study and systematic review. Eur J Intern Med. 2018; 51:68–73. PMID: 29361475.
Article12. Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800. PMID: 27794523.
Article13. Sinclair AM, Isles CG, Brown I, Cameron H, Murray GD, Robertson JW. Secondary hypertension in a blood pressure clinic. Arch Intern Med. 1987; 147:1289–1293. PMID: 3606286.
Article14. Anderson GH Jr, Blakeman N, Streeten DH. The effect of age on prevalence of secondary forms of hypertension in 4429 consecutively referred patients. J Hypertens. 1994; 12:609–615. PMID: 7930562.
Article15. Ariton M, Juan CS, AvRuskin TW. Pheochromocytoma: clinical observations from a Brooklyn tertiary hospital. Endocr Pract. 2000; 6:249–252. PMID: 11421540.
Article16. Omura M, Saito J, Yamaguchi K, Kakuta Y, Nishikawa T. Prospective study on the prevalence of secondary hypertension among hypertensive patients visiting a general outpatient clinic in Japan. Hypertens Res. 2004; 27:193–202. PMID: 15080378.
Article17. Beard CM, Sheps SG, Kurland LT, Carney JA, Lie JT. Occurrence of pheochromocytoma in Rochester, Minnesota, 1950 through 1979. Mayo Clin Proc. 1983; 58:802–804. PMID: 6645626.18. Guerrero MA, Schreinemakers JM, Vriens MR, Suh I, Hwang J, Shen WT, et al. Clinical spectrum of pheochromocytoma. J Am Coll Surg. 2009; 209:727–732. PMID: 19959041.
Article19. Mesmar B, Poola-Kella S, Malek R. The physiology behind diabetes mellitus in patients with pheochromocytoma: a review of the literature. Endocr Pract. 2017; 23:999–1005. PMID: 28613940.
Article20. Beninato T, Kluijfhout WP, Drake FT, Lim J, Kwon JS, Xiong M, et al. Resection of pheochromocytoma improves diabetes mellitus in the majority of patients. Ann Surg Oncol. 2017; 24:1208–1213. PMID: 27896511.
Article21. Kim BJ, Kwak MK, Ahn SH, Kim H, Lee SH, Song KH, et al. Lower bone mass and higher bone resorption in pheochromocytoma: importance of sympathetic activity on human bone. J Clin Endocrinol Metab. 2017; 102:2711–2718. PMID: 28582552.
Article22. Kim BJ, Lee SH, Koh JM. Bone health in adrenal disorders. Endocrinol Metab (Seoul). 2018; 33:1–8. PMID: 29589383.
Article23. Hamidi O, Young WF Jr, Iniguez-Ariza NM, Kittah NE, Gruber L, Bancos C, et al. Malignant pheochromocytoma and paraganglioma: 272 patients over 55 years. J Clin Endocrinol Metab. 2017; 102:3296–3305. PMID: 28605453.
Article24. Choi YM, Sung TY, Kim WG, Lee JJ, Ryu JS, Kim TY, et al. Clinical course and prognostic factors in patients with malignant heochromocytoma and paraganglioma: a single institution experience. J Surg Oncol. 2015; 112:815–821. PMID: 26464058.25. Li ML, Fitzgerald PA, Price DC, Norton JA. Iatrogenic pheochromocytomatosis: a previously unreported result of laparoscopic adrenalectomy. Surgery. 2001; 130:1072–1077. PMID: 11742341.
Article26. Bosca Robledo A, Ponce Marco JL, Belda Ibanez T, Meseguer Anastasio MF, Gomez Gavara C. Pheochromocytomatosis: a risk after pheochromocytoma surgery. Am Surg. 2010; 76:E122–E124. PMID: 21513631.27. Hamidi O, Young WF Jr, Gruber L, Smestad J, Yan Q, Ponce OJ, et al. Outcomes of patients with metastatic phaeochromocytoma and paraganglioma: a systematic review and meta-analysis. Clin Endocrinol (Oxf). 2017; 87:440–450. PMID: 28746746.
Article28. Ayala-Ramirez M, Feng L, Johnson MM, Ejaz S, Habra MA, Rich T, et al. Clinical risk factors for malignancy and overall survival in patients with pheochromocytomas and sympathetic paragangliomas: primary tumor size and primary tumor location as prognostic indicators. J Clin Endocrinol Metab. 2011; 96:717–725. PMID: 21190975.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Brief Overview of the Epidemiology of Pheochromocytoma and Paraganglioma in Korea
- Non-Functional Retroperitoneal Paraganglioma Mimicking an Ovary Mass: A Case Report
- A case of benign nonfunctioning retroperitoneal paraganglioma
- Risk Factors for Malignancy of Pheochromocytoma and Abdominal Paraganglioma in Children: Clinicopathologic Perspectives
- Clinical Analysis of Pheochromocytoma and Abdominal Paragangliomas