Ann Dermatol.
2020 Apr;32(2):174-176. 10.5021/ad.2020.32.2.174.
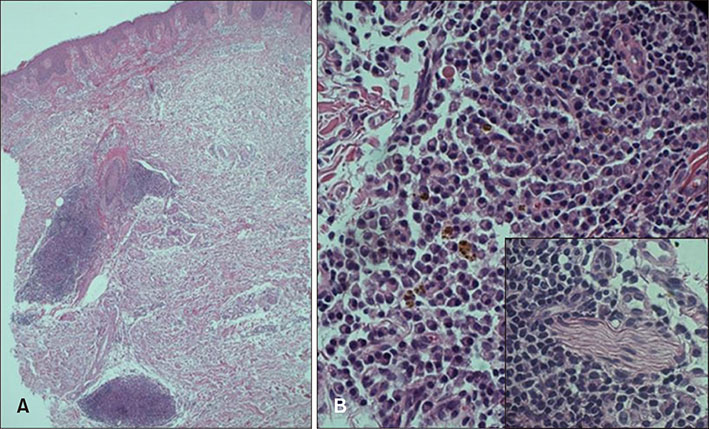
Cutaneous Plasmacytosis Showing a Neuronal Involvement in a 35-Year-Old Female
- Affiliations
-
- 1Department of Dermatology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. etihwevol@naver.com
- KMID: 2471349
- DOI: http://doi.org/10.5021/ad.2020.32.2.174
Abstract
- No abstract available.
Figure
Reference
-
1. Uhara H, Saida T, Ikegawa S, Yamazaki Y, Mikoshiba H, Nijoh S, et al. Primary cutaneous plasmacytosis: report of three cases and review of the literature. Dermatology. 1994; 189:251–255.
Article2. Haque M, Hou JS, Hisamichi K, Tamada K, Cusack CA, Abdelmalek M, et al. Cutaneous and systemic plasmacytosis vs. cutaneous plasmacytic castleman disease: review and speculations about pathogenesis. Clin Lymphoma Myeloma Leuk. 2011; 11:453–461.
Article3. Honda R, Cerroni L, Tanikawa A, Ebihara T, Amagai M, Ishiko A. Cutaneous plasmacytosis: report of 6 cases with or without systemic involvement. J Am Acad Dermatol. 2013; 68:978–985.
Article4. Han XD, Lee SSJ, Tan SH, Chong WS, Ng SK, Ooi MGM, et al. Cutaneous plasmacytosis: a clinicopathologic study of a series of cases and their treatment outcomes. Am J Dermatopathol. 2018; 40:36–42.
Article