Korean J Adult Nurs.
2020 Feb;32(1):46-56. 10.7475/kjan.2020.32.1.46.
Methodological Study on the Evaluation of Face Mask Use Scale among Public Adult: Cross-Language and Psychometric Testing
- Affiliations
-
- 1Assistant Professor, School of Nursing, The Hong Kong Polytechnic University, Hong Kong SAR. simon.c.lam@polyu.edu.hk, simlc@alumni.cuhk.net
- 2Senior Lecturer, School of Nursing and Health Studies, The Open University of Hong Kong, Hong Kong SAR.
- 3Registered Nurse, Yan Chai Hospital, Hospital Authority, Hong Kong SAR.
- 4Registered Nurse, Caritas Medical Center, Hospital Authority, Hong Kong SAR.
- 5Registered Nurse, Prince of Wales Hospital, Hospital Authority, Hong Kong SAR.
- 6Registered Nurse, Ruttonjee Hospital, Hospital Authority, Hong Kong SAR.
- 7Registered Nurse, Queen Mary Hospital, Hospital Authority, Hong Kong SAR.
- 8Registered Nurse, St. Paul's Hospital, Hong Kong Island, Hong Kong SAR.
- 9Registered Nurse, Department of Health, Hong Kong SAR.
- KMID: 2471028
- DOI: http://doi.org/10.7475/kjan.2020.32.1.46
Abstract
- PURPOSE
This study aimed to establish the translation adequacy and examine the psychometric properties of Face Mask Use Scale (FMUS).
METHODS
This methodological study employed a cross-sectional design with repeated measures. Phase 1 examined the equivalence and relevance of English and Chinese versions of FMUS. Phase 2 examined the internal consistency, stability and construct validity. Different sample batches (213 university students and 971 general public) were used appropriately for psychometric testing. The 2-phase data were collected between January and April 2017.
RESULTS
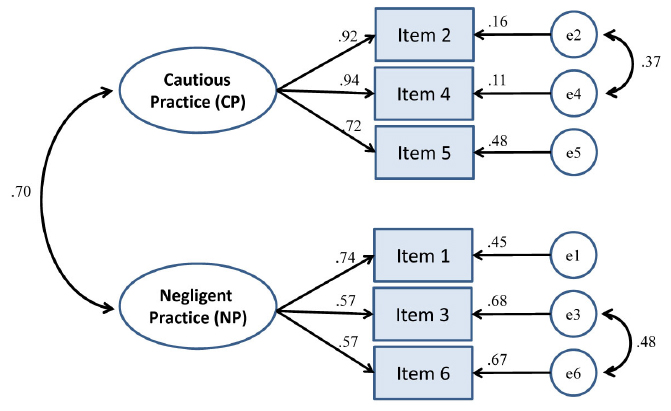
In Phase 1, the semantic equivalence and relevance (item- and scale-level content-validity-index=100%) was satisfactory. Furthermore, from 133 paired test-retest responses, the quadratic weighted kappa (.53~.73, p<.001) and Intraclass Correlation Coefficient (ICC=.81) between the English and Chinese version of FMUS were satisfactory. In Phase 2, FMUS demonstrated satisfactory internal consistency (Cronbach's α=.80~.81; corrected item-total correlation coefficients=.46~.67) and two-week test-retest stability (ICC=.84). The known-groups method (t=3.08, p<.001), exploratory (71.10% of total variance in two-factor model) and confirmatory factory analysis (χ²/df=4.02, Root Mean Square Residual=.03, Root Mean Square Error of Approximation=.06, Goodness of Fit Index=.99, Comparative Fit Index=.99) were all satisfactory for establishing the construct validity.
CONCLUSION
The FMUS has an equivalence Chinese and English versions, satisfactory reliability and validity for measuring the practice of face mask use. This poses clinical and research implications for those community health nurses who works on respiratory protection. Further research should be conducted on the "˜negligent practice' of FMU.
MeSH Terms
Figure
Reference
-
1. World Health Organization. Infection prevention and control of epidemic-and pandemic-prone acute respiratory diseases in health care: World Health Orgianzation guidelines [Internet]. Geneva: World Health Organization;2014. cited 2019 December 23. Available from: https://www.who.int/csr/bioriskreduction/infection_control/publication/en/.2. World Health Organization. Influenza (seasonal) [Internet]. Geneva: World Health Organization;2018. cited 2018 February 8. Available from: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal).3. Ho HSW. Use of face masks in a primary care outpatient setting in Hong Kong: knowledge, attitudes and practices. Public Health. 2012; 126(12):1001–1006. DOI: 10.1016/j.puhe.2012.09.010.
Article4. Wu P, Goldstein E, Ho LM, Wu JT, Tsang T, Leung GM, et al. Excess mortality impact of two epidemics of pandemic influenza A (H1N1pdm09) virus in Hong Kong. Influenza and Other Respiratory Viruses. 2014; 8(1):1–7. DOI: 10.1111/irv.12196.5. Department of health. Weekly consultation rates of influenzalike illness reported by General Out-patient Clinics (GOPC) and Private Medical Practitioner (PMP) Clinics 2017 [Internet]. 2017. cited 2018 February 8. Available from: https://www.chp.gov.hk/en/statistics/data/10/26/44/292/6306.html.6. Centers for Disease Control and Prevention. Influenza (Flu) [Internet]. US: Department of Health & Human Services;2016. cited 2018 February 8. Available from: https://www.cdc.gov/flu/index.htm.7. Brienen NC, Timen A, Wallinga J, van Steenbergen JE, Teunis PF. The effect of mask use on the spread of influenza during a pandemic. Risk Analysis. 2010; 30(8):1210–1218. DOI: 10.1111/j.1539-6924.2010.01428.x.
Article8. Chughtai AA, Seale H, Chi Dung T, Maher L, Nga PT, Mac-Intyre C. Current practices and barriers to the use of facemasks and respirators among hospital-based health care workers in Vietnam. American Journal of Infection Control. 2015; 43(1):72–77. DOI: 10.1016/j.ajic.2014.10.009.
Article9. Makison Booth C, Clayton M, Crook B, Gawn JM. Effectiveness of surgical masks against influenza bioaerosols. Journal of Hospital Infection. 2013; 84(1):22–26. DOI: 10.1016/j.jhin.2013.02.007.
Article10. Sim SW, Moey KSP, Tan NC. The use of facemasks to prevent respiratory infection: a literature review in the context of the Health Belief Model. Singapore Medical Journal. 2014; 55(3):160–167. DOI: 10.11622/smedj.2014037.
Article11. Smith SM, Sonego S, Wallen GR, Waterer G, Cheng AC, Thompson P. Use of non-pharmaceutical interventions to reduce the transmission of influenza in adults: a systematic review. Respirology. 2015; 20(6):896–903. DOI: 10.1111/resp.12541.
Article12. Chan EY, Cheng CK, Tam G, Huang Z, Lee P. Knowledge, attitudes, and practices of Hong Kong population towards human A/H7N9 influenza pandemic preparedness, China, 2014. BMC Public Health. 2015; 15:943. DOI: 10.1186/s12889-015-2245-9.
Article13. Lau JT, Griffiths S, Choi KC, Lin C. Prevalence of preventive behaviors and associated factors during early phase of the H1N1 influenza epidemic. American Journal of Infection Control. 2010; 38(5):374–380. DOI: 10.1016/j.ajic.2010.03.002.
Article14. Lau J, Griffiths S, Au D, Choi K. Changes in knowledge, perceptions, preventive behaviours and psychological responses in the pre-community outbreak phase of the H1N1 epidemic. Epidemiology and Infection. 2011; 139(1):80–90. DOI: 10.1017/S0950268810001925.
Article15. McDowell I. Measuring health: a guide to rating scales and questionnaires. New York: Oxford University Press;2006.16. Lam SC, Chan ZSL, Chong ACY, Wong WWC, Ye J. Adaptation and validation of Richmond Compulsive Buying Scale in Chinese population. Journal of Behavioral Addictions. 2018; 7(3):760–769. DOI: 10.1556/2006.7.2018.94.
Article17. Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. 5th ed. New York: Oxford University Press;2015.18. Lam SC, Yeung CCY, Chan JHM, Lam DWC, Lam AHY, Annesi-Maesano I, et al. Adaptation of the score for allergic rhinitis in the Chinese population: psychometric properties and diagnostic accuracy. International Archives of Allergy and Immunology. 2017; 173(4):213–224. DOI: 10.1159/000477727.
Article19. Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed. NJ: Prentice Hall Upper Saddle River;2009.20. Polit DF, Beck CT. The content validity index: are you sure you know what's being reported? Critique and recommendations. Research in Nursing & Health. 2006; 29(5):489–497. DOI: 10.1002/nur.20147.
Article21. Tabachnick BG, Fidell LS, Ullman JB. Using multivariate statistics. 7th ed. MA: Pearson Boston;2019.22. Lam C. Development and validation of a quality of life instrument for older Chinese people in residential care homes [dissertation]. Hong Kong: The Chinese University of Hong Kong;2015.23. Chau J, Thompson DR, Lee D, Twinn S. Infection control practices among hospital health and support workers in Hong Kong. Journal of Hospital Infection. 2010; 75(4):299–303. DOI: 10.1016/j.jhin.2009.10.014.
Article24. Yang P, Seale H, MacIntyre CR, Zhang H, Zhang Z, Zhang Y, et al. Mask-wearing and respiratory infection in healthcare workers in Beijing, China. The Brazilian Journal of Infectious Diseases. 2011; 15(2):102–108.
Article25. Floyd FJ, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment. 1995; 7(3):286–299. DOI: 10.1037/1040-3590.7.3.286.
Article26. Costello A, Osborne J. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Practical Assessment, Research & Evaluation. 2005; 10(7):1–9.27. Byrne BM. Structural equation modeling with AMOS: basic concepts, applications, and programming. 3rd ed. New York: Routledge;2016.28. Chong ACY, Lam SC, Chan LM, Lam MY, Tong KY, Lam MT, et al. Psychometric properties of Face Mask Use Scale. American Journal of Infection Control. 2017; 45(6):47–48. DOI: 10.1016/j.ajic.2017.04.075.
Article29. Chung JYS, Cheung JHM, Chong ACY, Lam SC. Practice of Face Mask Use Scale: cross-language testing of Chinese and English versions. American Journal of Infection Control. 2017; 45(6):162–163. DOI: 10.1016/j.ajic.2017.04.230.
Article30. Gaskin J. Confirmatory factor analysis [Internet]. Statwiki;2019. cited 2018 February 8. Available from: http://statwiki.kolobkreations.com/index.php?title=Confirmatory_Factor_Analysis.31. Ferng YH, Wong-McLoughlin J, Barrett A, Currie L, Larson E. Barriers to mask wearing for influenza-like illnesses among urban Hispanic households. Public Health Nursing. 2011; 28(1):13–23. DOI: 10.1111/j.1525-1446.2010.00918.x.
Article32. Petrie JG, Ohmit SE, Cowling BJ, Johnson E, Cross RT, Malosh RE, et al. Influenza transmission in a cohort of households with children: 2010-2011. PloS One. 2013; 8(9):e75339. DOI: 10.1371/journal.pone.0075339.
Article33. Mukerji S, MacIntyre CR, Newall AT. Review of economic evaluations of mask and respirator use for protection against respiratory infection transmission. BMC Infectious Diseases. 2015; 15:413. DOI: 10.1186/s12879-015-1167-6.
Article34. Polit DF. Getting serious about test-retest reliability: a critique of retest research and some recommendations. Quality of Life Research. 2014; 23(6):1713–1720. DOI: 10.1007/s11136-014-0632-9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Evaluation of the Validity and Reliability of the Face Mask Use Scale’s Korean Version among Community-Dwelling Adults
- Development and Psychometric Evaluation of the Resuscitation Self-efficacy Scale for Nurses
- Development and Psychometric Evaluation of the Transcultural Self-efficacy Scale for Nurses
- Review of the Psychometric Evidence of the Perceived Stress Scale
- Face Mask Usage, Knowledge and Behavior of Face Mask Usage in Older Adults Living Alone in the COVID-19 Era