J Korean Acad Nurs.
2012 Dec;42(7):1079-1086. 10.4040/jkan.2012.42.7.1079.
Development and Psychometric Evaluation of the Resuscitation Self-efficacy Scale for Nurses
- Affiliations
-
- 1Red Cross College of Nursing, Chung-Ang University (CAU), CAU Healthcare System, Seoul, Korea.
- 2Gordon Center for Research in Medical Education, University of Miami Miller School of Medicine, Miami, USA.
- 3Department of Emergency Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 4College of Nursing, The Nursing Policy Research Institute, Yonsei University, Seoul, Korea. soskim@yuhs.ac
- KMID: 1739546
- DOI: http://doi.org/10.4040/jkan.2012.42.7.1079
Abstract
- PURPOSE
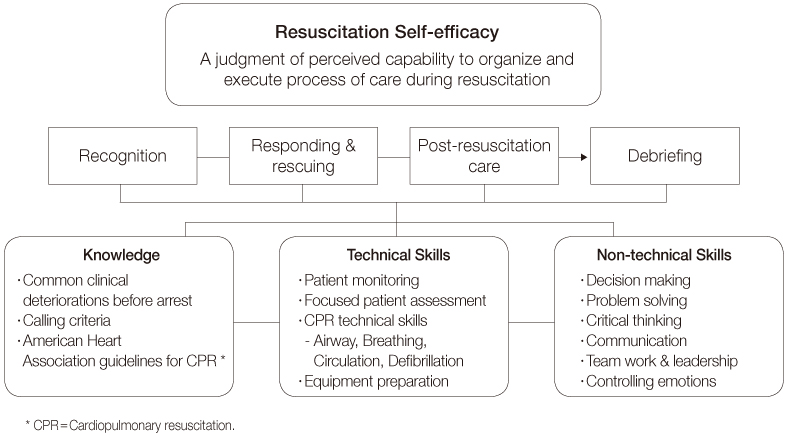
The purpose of this study was to develop and evaluate psychometric properties of the instrument, Resuscitation Self-Efficacy Scale for nurses.
METHODS
This was a methodological study for instrument development and psychometric testing. The initial item pool derived from literature review and experts resulted in 30 items linked to resuscitation self-efficacy. A convenience sample of 509 Korean nurses from eleven academic teaching hospitals participated in a survey to examine psychometric properties of the scale. To examine construct validity, exploratory factor analysis and known-group comparison were used. Cronbach's coefficient alpha was used to determine the scale's internal consistency reliability.
RESULTS
The final scale included 17 items with four-component structure termed 'Recognition', 'Debriefing and recording', 'Responding and rescuing', and 'Reporting'. These four factors accounted for 57.5% of the variance. Each subscale and the total scale demonstrated satisfactory internal consistency: .82; .88; .87; .83; and .91 respectively. Experienced nurses reported significantly higher self-efficacy mean scores in both total and subscales compared to new graduate nurses.
CONCLUSION
The Resuscitation Self-Efficacy Scale for nurses yields reliable and valid results in appraising the level of resuscitation self-efficacy for Korean nurses. Further study is needed to test and refine the scale.
Keyword
MeSH Terms
Figure
Reference
-
1. Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O'Hearn N, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005. 293(3):305–310. http://dx.doi.org/10.1001/jama.293.3.305.2. Bandura A. Self-efficacy: The exercise of control. 1997. New York: Freeman.3. Cant RP, Cooper SJ. Simulation-based learning in nurse education: Systematic review. J Adv Nurs. 2010. 66(1):3–15. http://dx/doi.org/10.1111/j.1365-2648.2009.05240.x.4. Carlo WA, Wright LL, Chomba E, McClure EM, Carlo ME, Bann CM, et al. Educational impact of the neonatal resuscitation program in low-risk delivery centers in a developing country. J Pediatr. 2009. 154:504–508. http://dx/doi.org/10.1016/j.jpeds.2008.10.005.5. Fuhrmann L, Lippert A, Perner A, Østergaard D. Incidence, staff awareness and mortality of patients at risk on general wards. Resuscitation. 2008. 77:325–330. http://dx/doi.org/10.1016/j.resuscitation.2008.01.009.6. Gordon CJ, Buckley T. The effect of high-fidelity simulation training on medical-surgical graduate nurses perceived ability to respond to patient clinical emergencies. J Contin Educ Nurs. 2009. 40:491–498. http://dx/doi.org/10.1016/j.resuscitation.2008.01.009.7. Hicks CM, Bandiera GW, Denny CJ. Building a simulation-based crisis resource management course for emergency medicine, phase 1: Results from an interdisciplinary needs assessment survey. Acad Emerg Med. 2008. 15:1136–1143. http://dx/doi.org/10.1111/j.1553-2712.2008.00185.x.8. Kim EJ, Lee KR, Lee MH, Kim JY. Nurses' cardiopulmonary resuscitation performance during the first 5 minutes in in-situ simulated cardiac arrest. J Korean Acad Nurs. 2012. 42(3):361–368. http://dx.doi.org/10.4040/jkan.2012.42.3.361.9. Maibach EW, Schieber RA, Carroll MF. Self-efficacy in pediatric resuscitation: Implications for education and performance. Pediatrics. 1996. 97:94–99.10. May BA, Limandri BJ. Instrument development of the Self-Efficacy Scale for abused women. Res Nurs Health. 2004. 27:208–214. http://dx/doi.org/10.1002/nur.20018.11. Moretti MA, Cesar LA, Nusbacher A, Kern KB, Timerman S, Ramires JA. Advanced cardiac life support training improves long-term survival from in-hospital cardiac arrest. Resuscitation. 2007. 72(3):458–465. http://dx.doi.org/10.1016/j.resuscitation.2006.06.039.12. Odell M, Victor C, Oliver D. Nurses' role in detecting deterioration in ward patients: Systematic literature review. J Adv Nurs. 2009. 65:1992–2006. http://dx/doi.org/10.1111/j.1365-2648.2009.05109.x.13. Pett MA, Lackey NR, Sullivan JJ. Making sense of factor analysis: The use of factor analysis for instrument development in health care research. 2003. London: Sage Publications.14. Pothitakis C, Ekmektzoglou KA, Piagkou M, Karatzas T, Xanthos T. Nursing role in monitoring during cardiopulmonary resuscitation and in the peri-arrest period: A review. Heart Lung. 2011. 40:530–544. http://dx/doi.org/10.1016/j.hrtlng.2010.11.006.15. Roh YS, Lee WS, Chung HS, Park YM. The effects of simulation-based resuscitation training on nurses' self-efficacy and satisfaction. Nurse Educ Today. 2011. http://dx/doi.org/10.1016/j.nedt.2011.11.008.16. Smith GB. In-hospital cardiac arrest: Is it time for an in-hospital 'chain of prevention'? Resuscitation. 2010. 81:1209–1211. http://dx/doi.org/10.1016/j.resuscitation.2010.04.017.17. Stump GS, Husman J, Brem SK. The Nursing Student Self-Efficacy Scale: Development using item response theory. Nurs Res. 2012. 61(3):149–158. http://dx/doi.org/10.1097/NNR.0b013e318253a750.18. Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR, et al. Part 4: CPR overview: 2010 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010. 122:18 Suppl 3. S676–S684. http://dx/doi.org/10.1161/CIRCULATIONAHA.110.970913.19. Turner NM, Lukkassen I, Bakker N, Draaisma J, ten Cate OT. The effect of the APLS-course on self-efficacy and its relationship to behavioural decisions in paediatric resuscitation. Resuscitation. 2009. 80:913–918. http://dx/doi.org/10.1016/j.resuscitation. 2009.03.028.20. Turner NM, van de Leemput AJ, Draaisma JM, Oosterveld P, ten Cate OT. Validity of the visual analogue scale as an instrument to measure self-efficacy in resuscitation skills. Med Educ. 2008. 42:503–511. http://dx/doi.org/doi:10.1111/j.1365-2923.2007.02950.x.21. van Schaik SM, Plant JL, Diane S, Tsang L, O'Sullivan P. Interprofessional team training in pediatric resuscitation: A low-cost, in situ simulation program that enhances self-efficacy among participants. Clin Pediatr (Phila). 2011. 50:807–815. http://dx/doi.org/10.1177/0009922811405518.22. Wayne DB, Didwania A, Feinglass J, Fudala MJ, Barsuk JH, McGaghie WC. Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: A case-control study. Chest. 2008. 133(1):56–61. http://dx/doi.org/10.1378/chest.07-0131.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and psychometric evaluation of Clinical Practice Self-Efficacy Scale for nursing students
- Corrigendum: Development and Psychometric Evaluation of the Transcultural Self-efficacy Scale for Nurses
- Development and Psychometric Evaluation of the Transcultural Self-efficacy Scale for Nurses
- Development and Psychometric Evaluation of the Career Growth Scale for Nurses
- Review of the Psychometric Evidence of the Perceived Stress Scale