Diabetes Metab J.
2020 Feb;44(1):56-66. 10.4093/dmj.2018.0227.
An Electronic Health Record-Integrated Computerized Intravenous Insulin Infusion Protocol: Clinical Outcomes and in Silico Adjustment
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. sangman.jin@samsung.com
- 2Department of Creative IT Engineering, Pohang University of Science and Technology (POSTECH), Pohang, Korea. sungminpark@postech.ac.kr
- 3Department of Emergency Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Digital Health, Samsung Advanced Institute for Health Sciences & Technology, Sungkyunkwan University, Seoul, Korea.
- KMID: 2470955
- DOI: http://doi.org/10.4093/dmj.2018.0227
Abstract
- BACKGROUND
We aimed to describe the outcome of a computerized intravenous insulin infusion (CII) protocol integrated to the electronic health record (EHR) system and to improve the CII protocol in silico using the EHR-based predictors of the outcome.
METHODS
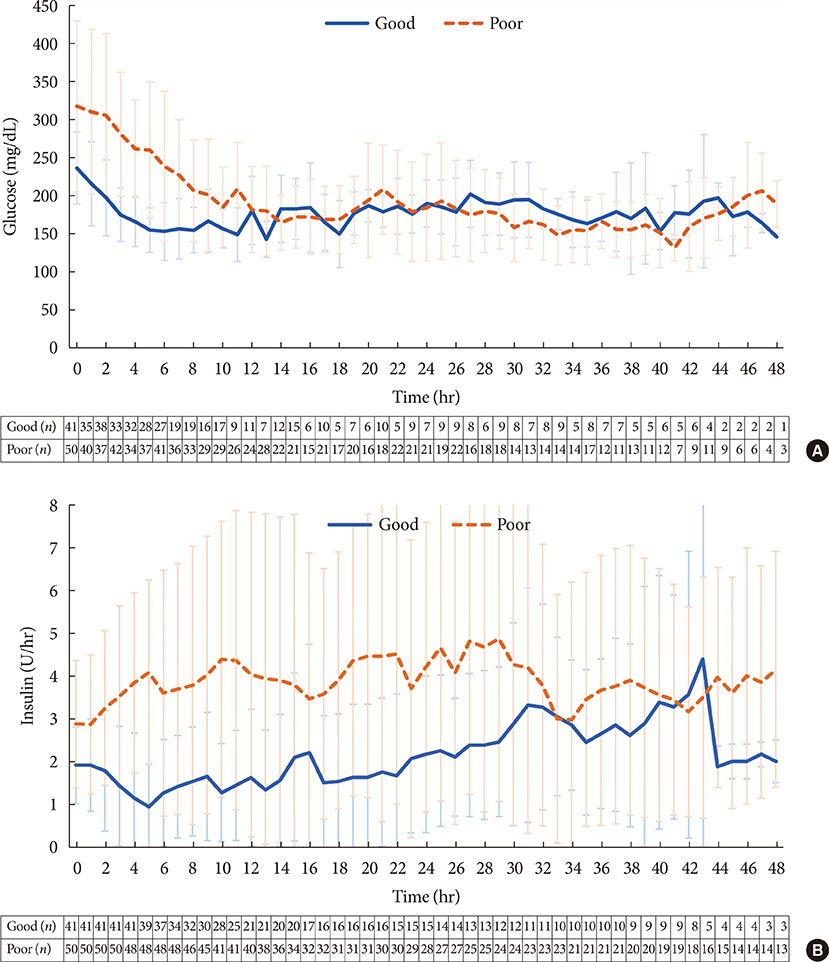
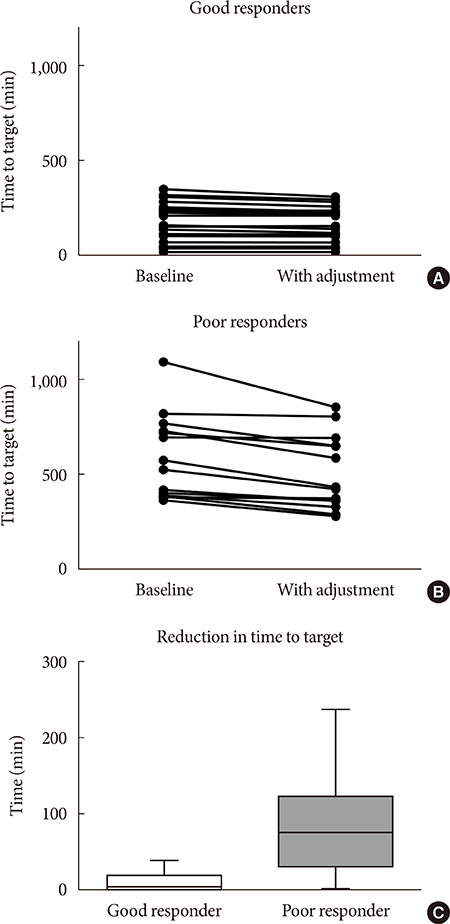
Clinical outcomes of the patients who underwent the CII protocol between July 2016 and February 2017 and their matched controls were evaluated. In the CII protocol group (n=91), multivariable binary logistic regression analysis models were used to determine the independent associates with a delayed response (taking ≥6.0 hours for entering a glucose range of 70 to 180 mg/dL). The CII protocol was adjusted in silico according to the EHR-based parameters obtained in the first 3 hours of CII.
RESULTS
Use of the CII protocol was associated with fewer subjects with hypoglycemia alert values (P=0.003), earlier (P=0.002), and more stable (P=0.017) achievement of a glucose range of 70 to 180 mg/dL. Initial glucose level (P=0.001), change in glucose during the first 2 hours (P=0.026), and change in insulin infusion rate during the first 3 hours (P=0.029) were independently associated with delayed responses. Increasing the insulin infusion rate temporarily according to these parameters in silico significantly reduced delayed responses (P<0.0001) without hypoglycemia, especially in refractory patients.
CONCLUSION
Our CII protocol enabled faster and more stable glycemic control than conventional care with minimized risk of hypoglycemia. An EHR-based adjustment was simulated to reduce delayed responses without increased incidence of hypoglycemia.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Letter: An Electronic Health Record-Integrated Computerized Intravenous Insulin Infusion Protocol: Clinical Outcomes and
in Silico Adjustment (Diabetes Metab J 2020;44:56–66)
Dongwon Yi
Diabetes Metab J. 2020;44(2):354-355. doi: 10.4093/dmj.2020.0071.Response: An Electronic Health Record-Integrated Computerized Intravenous Insulin Infusion Protocol: Clinical Outcomes and
in Silico Adjustment (Diabetes Metab J 2020;44:56–66)
Sung Woon Park, Seunghyun Lee, Won Chul Cha, Kyu Yeon Hur, Jae Hyeon Kim, Moon-Kyu Lee, Sung-Min Park, Sang-Man Jin
Diabetes Metab J. 2020;44(2):358-359. doi: 10.4093/dmj.2020.0080.
Reference
-
1. Falciglia M, Freyberg RW, Almenoff PL, D'Alessio DA, Render ML. Hyperglycemia-related mortality in critically ill patients varies with admission diagnosis. Crit Care Med. 2009; 37:3001–3009.
Article2. Norhammar AM, Ryden L, Malmberg K. Admission plasma glucose. Independent risk factor for long-term prognosis after myocardial infarction even in nondiabetic patients. Diabetes Care. 1999; 22:1827–1831.
Article3. Yendamuri S, Fulda GJ, Tinkoff GH. Admission hyperglycemia as a prognostic indicator in trauma. J Trauma. 2003; 55:33–38.
Article4. Golden SH, Peart-Vigilance C, Kao WH, Brancati FL. Perioperative glycemic control and the risk of infectious complications in a cohort of adults with diabetes. Diabetes Care. 1999; 22:1408–1414.
Article5. van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001; 345:1359–1367.
Article6. Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S, Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C, Natanson C, Loeffler M, Reinhart K. German Competence Network Sepsis (SepNet). Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008; 358:125–139.
Article7. NICE-SUGAR Study Investigators. Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hebert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009; 360:1283–1297.
Article8. Preiser JC, Devos P, Ruiz-Santana S, Melot C, Annane D, Groeneveld J, Iapichino G, Leverve X, Nitenberg G, Singer P, Wernerman J, Joannidis M, Stecher A, Chiolero R. A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med. 2009; 35:1738–1748.
Article9. Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, Inzucchi SE, Ismail-Beigi F, Kirkman MS, Umpierrez GE. American Association of Clinical Endocrinologists. American Diabetes Association. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Endocr Pract. 2009; 15:353–369.
Article10. Wilson M, Weinreb J, Hoo GW. Intensive insulin therapy in critical care: a review of 12 protocols. Diabetes Care. 2007; 30:1005–1011.
Article11. Zhang Y. Predicting occurrences of acute hypoglycemia during insulin therapy in the intensive care unit. Conf Proc IEEE Eng Med Biol Soc. 2008; 2008:3297–3300.
Article12. Boord JB, Sharifi M, Greevy RA, Griffin MR, Lee VK, Webb TA, May ME, Waitman LR, May AK, Miller RA. Computer-based insulin infusion protocol improves glycemia control over manual protocol. J Am Med Inform Assoc. 2007; 14:278–287.
Article13. Davidson PC, Steed RD, Bode BW. Glucommander: a computer-directed intravenous insulin system shown to be safe, simple, and effective in 120,618 h of operation. Diabetes Care. 2005; 28:2418–2423.
Article14. Dortch MJ, Mowery NT, Ozdas A, Dossett L, Cao H, Collier B, Holder G, Miller RA, May AK. A computerized insulin infusion titration protocol improves glucose control with less hypoglycemia compared to a manual titration protocol in a trauma intensive care unit. JPEN J Parenter Enteral Nutr. 2008; 32:18–27.
Article15. Newton CA, Smiley D, Bode BW, Kitabchi AE, Davidson PC, Jacobs S, Steed RD, Stentz F, Peng L, Mulligan P, Freire AX, Temponi A, Umpierrez GE. A comparison study of continuous insulin infusion protocols in the medical intensive care unit: computer-guided vs. standard column-based algorithms. J Hosp Med. 2010; 5:432–437.
Article16. Saur NM, Kongable GL, Holewinski S, O'Brien K, Nasraway SA Jr. Software-guided insulin dosing: tight glycemic control and decreased glycemic derangements in critically ill patients. Mayo Clin Proc. 2013; 88:920–929.
Article17. Kelly JL. Continuous insulin infusion: when, where, and how? Diabetes Spectr. 2014; 27:218–223.
Article18. Marvin MR, Inzucchi SE, Besterman BJ. Computerization of the Yale insulin infusion protocol and potential insights into causes of hypoglycemia with intravenous insulin. Diabetes Technol Ther. 2013; 15:246–252.
Article19. Maahs DM, Buckingham BA, Castle JR, Cinar A, Damiano ER, Dassau E, DeVries JH, Doyle FJ 3rd, Griffen SC, Haidar A, Heinemann L, Hovorka R, Jones TW, Kollman C, Kovatchev B, Levy BL, Nimri R, O'Neal DN, Philip M, Renard E, Russell SJ, Weinzimer SA, Zisser H, Lum JW. Outcome measures for artificial pancreas clinical trials: a consensus report. Diabetes Care. 2016; 39:1175–1179.20. Van Herpe T, Pluymers B, Espinoza M, Van den Berghe G, De Moor B. A minimal model for glycemia control in critically ill patients. Conf Proc IEEE Eng Med Biol Soc. 2006; 1:5432–5435.
Article21. Bergman RN, Phillips LS, Cobelli C. Physiologic evaluation of factors controlling glucose tolerance in man: measurement of insulin sensitivity and beta-cell glucose sensitivity from the response to intravenous glucose. J Clin Invest. 1981; 68:1456–1467.
Article22. Juneja R, Roudebush CP, Nasraway SA, Golas AA, Jacobi J, Carroll J, Nelson D, Abad VJ, Flanders SJ. Computerized intensive insulin dosing can mitigate hypoglycemia and achieve tight glycemic control when glucose measurement is performed frequently and on time. Crit Care. 2009; 13:R163.
Article23. Dumont C, Bourguignon C. Effect of a computerized insulin dose calculator on the process of glycemic control. Am J Crit Care. 2012; 21:106–115.
Article24. Marvin MR, Inzucchi SE, Besterman BJ. Minimization of hypoglycemia as an adverse event during insulin infusion: further refinement of the Yale protocol. Diabetes Technol Ther. 2016; 18:480–486.
Article25. Telford ED, Franck AJ, Hendrickson AL, Dietrich NM. A bedside computerized decision-support tool for intravenous insulin infusion management in critically ill patients. Jt Comm J Qual Patient Saf. 2018; 44:299–303.
Article26. Hanazaki K, Kitagawa H, Yatabe T, Munekage M, Dabanaka K, Takezaki Y, Tsukamoto Y, Asano T, Kinoshita Y, Namikawa T. Perioperative intensive insulin therapy using an artificial endocrine pancreas with closed-loop glycemic control system: the effects of no hypoglycemia. Am J Surg. 2014; 207:935–941.
Article27. Ichimori S, Nishida K, Shimoda S, Sekigami T, Matsuo Y, Ichinose K, Shichiri M, Sakakida M, Araki E. Development of a highly responsive needle-type glucose sensor using polyimide for a wearable artificial endocrine pancreas. J Artif Organs. 2006; 9:105–113.
Article28. Matsuo Y, Shimoda S, Sakakida M, Nishida K, Sekigami T, Ichimori S, Ichinose K, Shichiri M, Araki E. Strict glycemic control in diabetic dogs with closed-loop intraperitoneal insulin infusion algorithm designed for an artificial endocrine pancreas. J Artif Organs. 2003; 6:55–63.
Article29. Namikawa T, Munekage M, Kitagawa H, Yatabe T, Maeda H, Tsukamoto Y, Hirano K, Asano T, Kinoshita Y, Hanazaki K. Comparison between a novel and conventional artificial pancreas for perioperative glycemic control using a closed-loop system. J Artif Organs. 2017; 20:84–90.
Article30. Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D. Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg. 2013; 257:8–14.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Electronic Health Record-Integrated Computerized Intravenous Insulin Infusion Protocol: Clinical Outcomes and in Silico Adjustment (Diabetes Metab J 2020;44:56-66)
- An Electronic Health Record-Integrated Computerized Intravenous Insulin Infusion Protocol: Clinical Outcomes and in Silico Adjustment (Diabetes Metab J 2020;44:56-66)
- Efficiency of Computerized Insulin Infusion Glucose Control in Critically Ill Patients
- Clinical Terminologies: A Solution for Semantic Interoperability
- The Application and Effect of the Nursing Protocol of Pediatric Peripheral Intravenous Infusion