Yonsei Med J.
2020 Mar;61(3):235-242. 10.3349/ymj.2020.61.3.235.
Contra-Lateral Unintended Upper Arm Movement during Unimanual Tasks in Children with Cerebral Palsy
- Affiliations
-
- 1Department of Rehabilitation Medicine, Severance Hospital, Research Institute of Rehabilitation Medicine, Yonsei University College of Medicine, Seoul, Korea. pes1234@yuhs.ac
- KMID: 2470920
- DOI: http://doi.org/10.3349/ymj.2020.61.3.235
Abstract
- PURPOSE
To characterize associated reactions (ARs) in the contralateral arm across multiple muscles during unimanual tasks and to identify factors related to ARs in children with cerebral palsy (CP).
MATERIALS AND METHODS
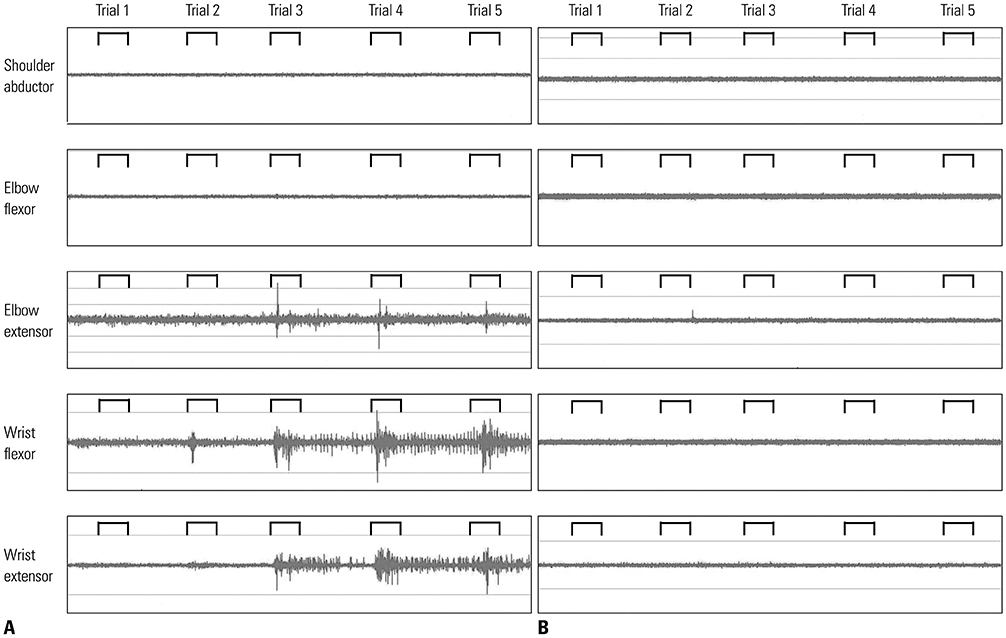
This was a prospective, cross-sectional study of 35 children with CP. The extent of ARs of the contra-lateral, non-task hand was assessed while performing three unimanual tasks (opening and clenching the fist, a finger opposition task, and tapping fingers). The occurrence of ARs in each trial was evaluated separately for each task using a four-point scale (total scores ranged from 0 to 12). Surface electromyography (SEMG) was used to measure the firing activity of the muscles of the opposite arm during the task. The Manual Ability Classification System and Melbourne Assessment 2 (MA-2) were used to evaluate upper limb function.
RESULTS
AR scores were higher in the more-affected limb than in the less-affected limb. SEMG data on the non-task hand showed motor overflow up to the elbow muscles in the more-affected limb. Root mean square ratios of EMG signals were significantly higher in children with ARs than in children without ARs. Multiple regression analysis showed both age and MA-2 to be significant factors related to ARs in the more-affected limb.
CONCLUSION
Children with visible ARs showed motor overflow in the non-task limb during unimanual hand tasks. Age and upper limb function were significantly related to the extent of ARs in the more-affected limb of children with CP.
MeSH Terms
Figure
Reference
-
1. Kim SW, Jeon HR, Shin JC, Youk T, Kim J. Incidence of cerebral palsy in Korea and the effect of socioeconomic status: a population-based nationwide study. Yonsei Med J. 2018; 59:781–786.
Article2. Carr LJ, Harrison LM, Evans AL, Stephens JA. Patterns of central motor reorganization in hemiplegic cerebral palsy. Brain. 1993; 116(Pt 5):1223–1247.
Article3. Abercrombie ML, Lindon RL, Tyson MC. Associated movements in normal and physically hadicapped children. Dev Med Child Neurol. 1964; 6:573–580.4. D'Agati E, Casarelli L, Pitzianti MB, Pasini A. Overflow movements and white matter abnormalities in ADHD. Prog Neuropsychopharmacol Biol Psychiatry. 2010; 34:441–445.5. Kuhtz-Buschbeck JP, Sundholm LK, Eliasson AC, Forssberg H. Quantitative assessment of mirror movements in children and adolescents with hemiplegic cerebral palsy. Dev Med Child Neurol. 2000; 42:728–736.
Article6. Connolly K, Stratton P. Developmental changes in associated movements. Dev Med Child Neurol. 1968; 10:49–56.
Article7. Zielinski IM, Green D, Rudisch J, Jongsma ML, Aarts PB, Steenbergen B. The relation between mirror movements and non-use of the affected hand in children with unilateral cerebral palsy. Dev Med Child Neurol. 2017; 59:152–159.
Article8. Klingels K, Jaspers E, Staudt M, Guzzetta A, Mailleux L, Ortibus E, et al. Do mirror movements relate to hand function and timing of the brain lesion in children with unilateral cerebral palsy? Dev Med Child Neurol. 2016; 58:735–742.
Article9. Adler C, Berweck S, Lidzba K, Becher T, Staudt M. Mirror movements in unilateral spastic cerebral palsy: specific negative impact on bimanual activities of daily living. Eur J Paediatr Neurol. 2015; 19:504–509.
Article10. Chiu HC, Halaki M, O'Dwyer N. Associated reactions during a visual pursuit position tracking task in hemiplegic and quadriplegic cerebral palsy. Chin J Physiol. 2013; 56:117–126.11. Eliasson AC, Krumlinde-Sundholm L, Rösblad B, Beckung E, Arner M, Ohrvall AM, et al. The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol. 2006; 48:549–554.
Article12. Ozer K, Chesher SP, Scheker LR. Neuromuscular electrical stimulation and dynamic bracing for the management of upper-extremity spasticity in children with cerebral palsy. Dev Med Child Neurol. 2006; 48:559–563.
Article13. Randall M, Imms C, Carey LM, Pallant JF. Rasch analysis of the Melbourne Assessment of Unilateral Upper Limb Function. Dev Med Child Neurol. 2014; 56:665–672.
Article14. Zielinski IM, Steenbergen B, Schmidt A, Klingels K, Simon Martinez C, de Water P, et al. Windmill-task as a new quantitative and objective assessment for mirror movements in unilateral cerebral palsy: a pilot study. Arch Phys Med Rehabil. 2018; 99:1547–1552.
Article15. Woods BT, Teuber HL. Mirror movements after childhood hemiparesis. Neurology. 1978; 28:1152–1157.
Article16. Swinscow TDV, Campbell MJ. Statistics at square one. 9th (online) ed. Southampton: BMJ Publishing Group;1997.17. Cohen HJ, Taft LT, Mahadeviah MS, Birch HG. Developmental changes in overflow in normal and aberrantly functioning children. J Pediatr. 1967; 71:39–47.
Article18. Schott GD, Wyke MA. Congenital mirror movements. J Neurol Neurosurg Psychiatry. 1981; 44:586–599.
Article19. Wolff PH, Gunnoe CE, Cohen C. Associated movements as a measure of developmental age. Dev Med Child Neurol. 1983; 25:417–429.
Article20. Mayston MJ, Harrison LM, Stephens JA. A neurophysiological study of mirror movements in adults and children. Ann Neurol. 1999; 45:583–594.
Article21. Seo NJ. Involuntary contralateral upper extremity muscle activation pattern during unilateral pinch grip following stroke. J Hand Ther. 2013; 26:272–277.
Article22. Sukal-Moulton T, Murray TM, Dewald JP. Loss of independent limb control in childhood hemiparesis is related to time of brain injury onset. Exp Brain Res. 2013; 225:455–463.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relation among the Gross Motor Function, Manual Performance and Upper Limb Functional Measures in Children with Spastic Cerebral Palsy
- Brain SPECT Analysis After Constraint-Induced Movement Therapy in Young Children with Hemiplegic Cerebral Palsy: Case Report
- Effects of the Constraint-Induced Movement Therapy on Cortical Reorganization in Patients with Hemiplegic Cerebral Palsy
- The Effect of a Task-oriented Upper Arm Exercise on Stable and Unstable Surfaces on Dynamic Balance and Hand Function in Patient with Cerebral Palsy
- The Effects of Single Event Multi-level Chemoneurolysis on Upper Extremity Function in Children with Cerebral Palsy