Korean J Radiol.
2020 Mar;21(3):325-331. 10.3348/kjr.2019.0508.
Magnetic Resonance Imaging Findings Differentiating Cutaneous Basal Cell Carcinoma from Squamous Cell Carcinoma in the Head and Neck Region
- Affiliations
-
- 1Department of Radiology, Gifu University School of Medicine, Gifu, Japan. hkato@gifu-u.ac.jp
- 2Department of Tumor Pathology, Gifu University School of Medicine, Gifu, Japan.
- 3Department of Pathology, Gifu University School of Medicine, Gifu, Japan.
- 4Department of Dermatology, Gifu University School of Medicine, Gifu, Japan.
- KMID: 2470756
- DOI: http://doi.org/10.3348/kjr.2019.0508
Abstract
OBJECTIVE
This study aimed to evaluate the efficacy of magnetic resonance (MR) imaging in differentiating between cutaneous basal cell carcinoma (cBCC) and cutaneous squamous cell carcinoma (cSCC) in the head and neck region.
MATERIALS AND METHODS
Among patients with cutaneous head and neck cancers, 14 with primary cBCCs and 15 with primary cSCCs with a histologic tumor height of ≥ 4 mm underwent MR examinations; the findings were then examined for correlations.
RESULTS
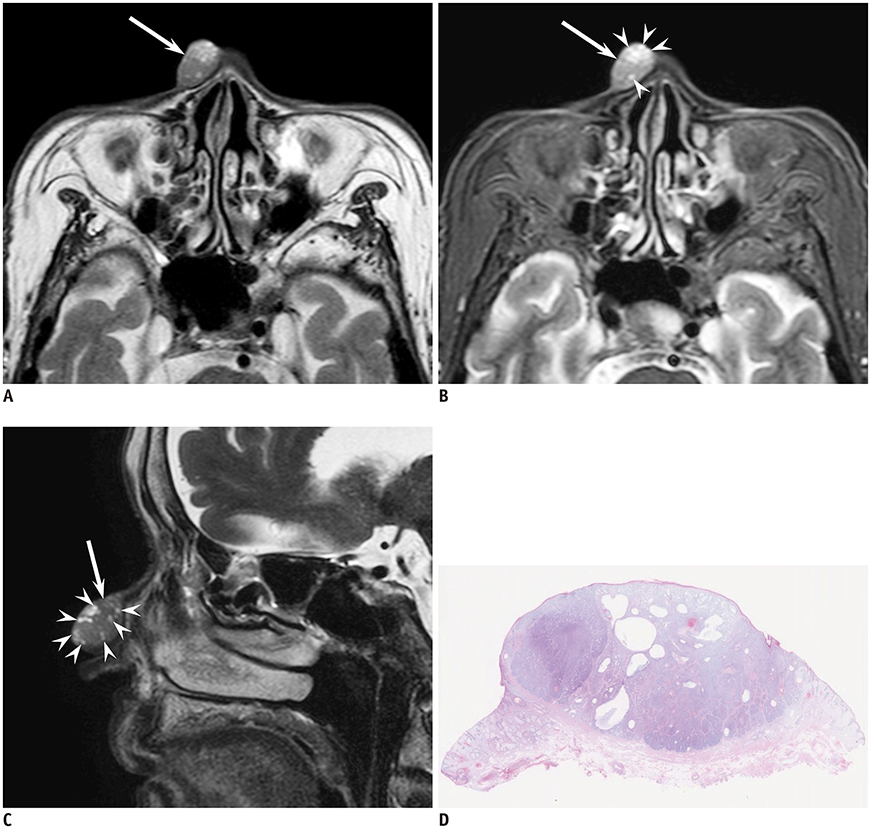
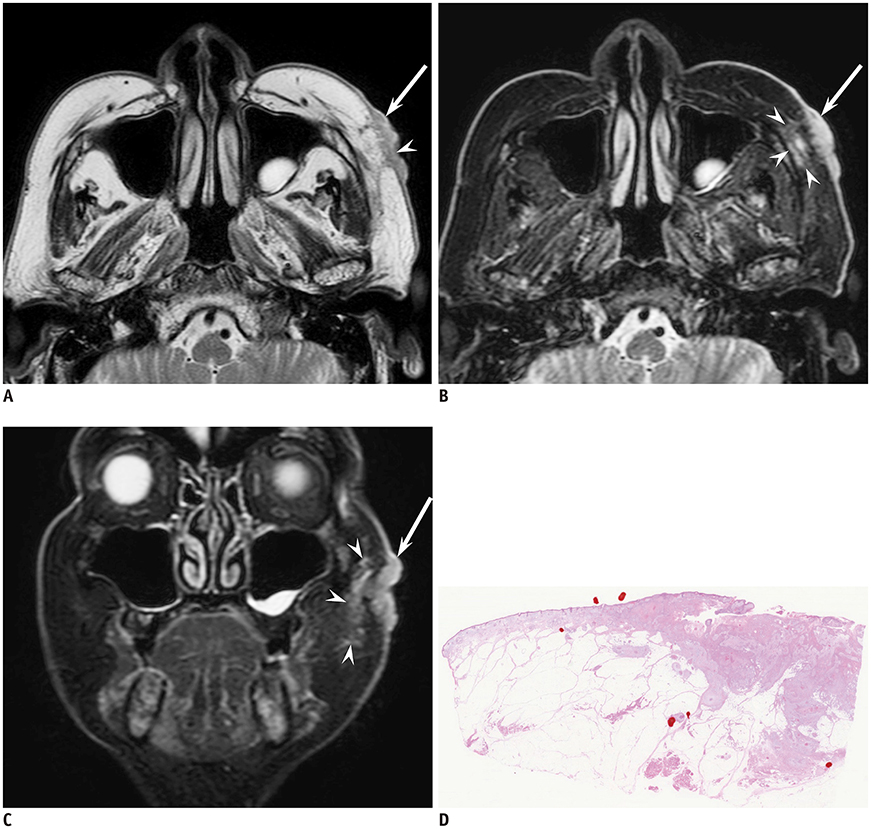
cBCCs (71%) occurred more frequently on the nose than cSCCs (13%) (p < 0.01). The maximum diameter (23.5 ± 7.2 mm vs. 12.7 ± 4.5 mm; p < 0.01) and diameter-to-height ratio (2.8 ± 0.9 vs. 1.7 ± 0.4; p < 0.01) were significantly greater in cSCCs than in cBCCs. Superficial ulcer formation (67% vs. 21%; p < 0.05), protrusion into the subcutaneous tissue (60% vs. 21%; p < 0.05), ill-demarcated deep tumor margins (60% vs. 7%; p < 0.01), and peritumoral fat stranding (93% vs. 7%; p < 0.01) were more frequently observed in cSCCs than in cBCCs. Intratumoral T2-hyperintense foci (57% vs. 13%; p < 0.05) were more frequently observed in cBCCs than in cSCCs.
CONCLUSION
cBCCs predominantly occurred on the nose with intratumoral T2-hyperintense foci, whereas cSCCs predominantly exhibited a flattened configuration, superficial ulcer formation, protrusion into the subcutaneous tissue, ill-demarcated deep tumor margin, and peritumoral fat stranding.
MeSH Terms
Figure
Reference
-
1. Demirseren DD, Ceran C, Aksam B, Demirseren ME, Metin A. Basal cell carcinoma of the head and neck region: a retrospective analysis of completely excised 331 cases. J Skin Cancer. 2014; 2014:858636.
Article2. Janjua OS, Qureshi SM. Basal cell carcinoma of the head and neck region: an analysis of 171 cases. J Skin Cancer. 2012; 2012:943472.
Article3. Nakayama M, Tabuchi K, Nakamura Y, Hara A. Basal cell carcinoma of the head and neck. J Skin Cancer. 2011; 2011:496910.
Article4. Narayanan DL, Saladi RN, Fox JL. Ultraviolet radiation and skin cancer. Int J Dermatol. 2010; 49:978–986.5. Gurudutt VV, Genden EM. Cutaneous squamous cell carcinoma of the head and neck. J Skin Cancer. 2011; 2011:502723.
Article6. Nguyen-Nielsen M, Wang L, Pedersen L, Olesen AB, Hou J, Mackey H, et al. The incidence of metastatic basal cell carcinoma (mBCC) in Denmark, 1997-2010. Eur J Dermatol. 2015; 25:463–468.
Article7. Joseph MG, Zulueta WP, Kennedy PJ. Squamous cell carcinoma of the skin of the trunk and limbs: the incidence of metastases and their outcome. Aust N Z J Surg. 1992; 62:697–701.
Article8. Brantsch KD, Meisner C, Schönfisch B, Trilling B, Wehner-Caroli J, Röcken M, et al. Analysis of risk factors determining prognosis of cutaneous squamous-cell carcinoma: a prospective study. Lancet Oncol. 2008; 9:713–720.
Article9. Brougham ND, Dennett ER, Cameron R, Tan ST. The incidence of metastasis from cutaneous squamous cell carcinoma and the impact of its risk factors. J Surg Oncol. 2012; 106:811–815.
Article10. Work Group. Invited Reviewers. Kim JYS, Kozlow JH, Mittal B, Moyer J, Olencki T, Rodgers P. Guidelines of care for the management of basal cell carcinoma. J Am Acad Dermatol. 2018; 78:540–559.
Article11. Work Group. Invited Reviewers. Kim JYS, Kozlow JH, Mittal B, Moyer J, Olenecki T, Rodgers P. Guidelines of care for the management of cutaneous squamous cell carcinoma. J Am Acad Dermatol. 2018; 78:560–578.
Article12. Baheti AD, Tirumani SH, Giardino A, Rosenthal MH, Tirumani H, Krajewski K, et al. Basal cell carcinoma: a comprehensive review for the radiologist. AJR Am J Roentgenol. 2015; 204:W132–W140.
Article13. Kim JH, Kim JY, Chun KA, Jee WH, Sung MS. MR imaging manifestations of skin tumors. Eur Radiol. 2008; 18:2652–2661.
Article14. Gufler H, Franke FE, Rau WS. High-resolution MRI of basal cell carcinomas of the face using a microscopy coil. AJR Am J Roentgenol. 2007; 188:W480–W484.
Article15. Budak MJ, Weir-McCall JR, Yeap PM, White RD, Waugh SA, Sudarshan TA, et al. High-resolution microscopy-coil MR imaging of skin tumors: techniques and novel clinical applications. Radiographics. 2015; 35:1077–1090.
Article16. Juan YH, Saboo SS, Tirumani SH, Khandelwal A, Shinagare AB, Ramaiya N, et al. Malignant skin and subcutaneous neoplasms in adults: multimodality imaging with CT, MRI, and 18F-FDG PET/CT. AJR Am J Roentgenol. 2014; 202:W422–W438.17. Choi JH, Kim YJ, Kim H, Nam SH, Choi YW. Distribution of basal cell carcinoma and squamous cell carcinoma by facial esthetic unit. Arch Plast Surg. 2013; 40:387–391.
Article18. Szewczyk M, Pazdrowski J, Golusiński P, Dańczak-Pazdrowska A, Marszałek S, Golusiński W. Analysis of selected risk factors for nodal metastases in head and neck cutaneous squamous cell carcinoma. Eur Arch Otorhinolaryngol. 2015; 272:3007–3012.
Article19. Chiang KH, Chou AS, Hsu YH, Lee SK, Lee CC, Yen PS, et al. Marjolin's ulcer: MR appearance. AJR Am J Roentgenol. 2006; 186:819–820.
Article20. Singer AD, Datir A, Tresley J, Langley T, Clifford PD, Jose J, et al. Benign and malignant tumors of the foot and ankle. Skeletal Radiol. 2016; 45:287–305.
Article21. Uhara H, Hayashi K, Koga H, Saida T. Multiple hypersonographic spots in basal cell carcinoma. Dermatol Surg. 2007; 33:1215–1219.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Squamous Cell Carcinoma of the Pancreas: A Case Report
- Comments to "A Case of Squamous Cell Carcinoma Developing in a Nevus Sebaceus of the Scalp"
- Synchronous thyroid carcinoma and squamous cell carcinoma: A case report
- Coexistence of Intracranial Squamous Cell Carcinoma and Epidermoid Cyst: a Case with Consecutive Imaging Findings
- Nevoid Basal Cell Carcinoma Syndrome: A Case Report and Literature Review