Clin Orthop Surg.
2020 Mar;12(1):55-59. 10.4055/cios.2020.12.1.55.
Review of Physician Referrals to Orthopedic Spine versus Neurosurgery
- Affiliations
-
- 1Department of Orthopedic Surgery, St. Luke's University Health Network, Bethlehem, PA, USA. ajith.malige@gmail.com
- 2Rothman Orthopedic Institute, Philadelphia, PA, USA.
- KMID: 2470051
- DOI: http://doi.org/10.4055/cios.2020.12.1.55
Abstract
- BACKGROUND
Previous studies have reported what patients value while choosing their surgeon, but there are no studies exploring the patterns of referral to spine surgeons among primary care physicians (PCPs). This study aims to identify any trends in PCPs' referral to orthopedic surgery versus neurosurgery for spinal pathology.
METHODS
In total, 450 internal medicine, family medicine, emergency medicine, neurology, and pain management physicians who practice at one of three locations (suburban community hospital, urban academic university hospital, and urban private practice) were asked to participate in the study. Consenting physicians completed our 24-question survey addressing their beliefs according to pathologies, locations of pathologies, and surgical interventions.
RESULTS
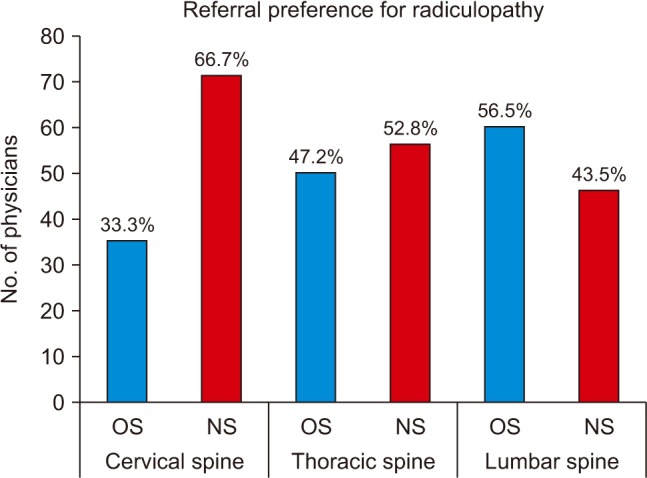
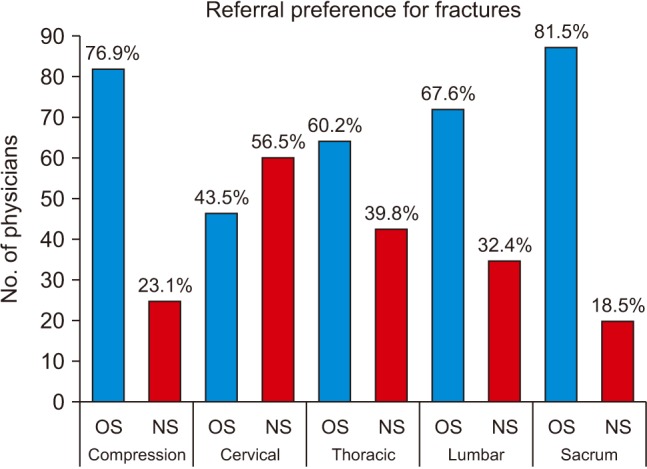
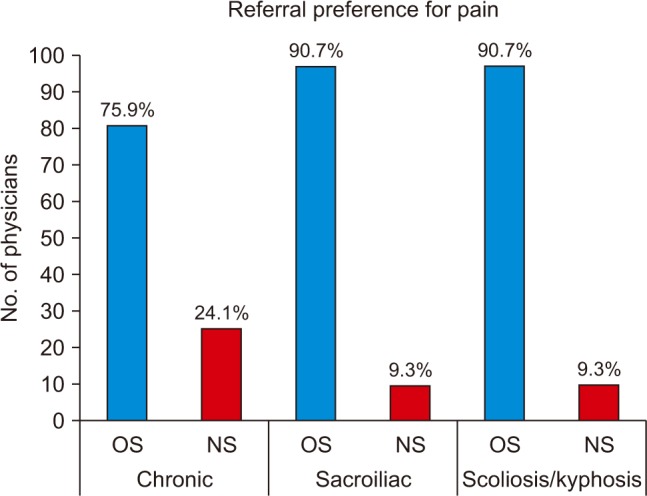
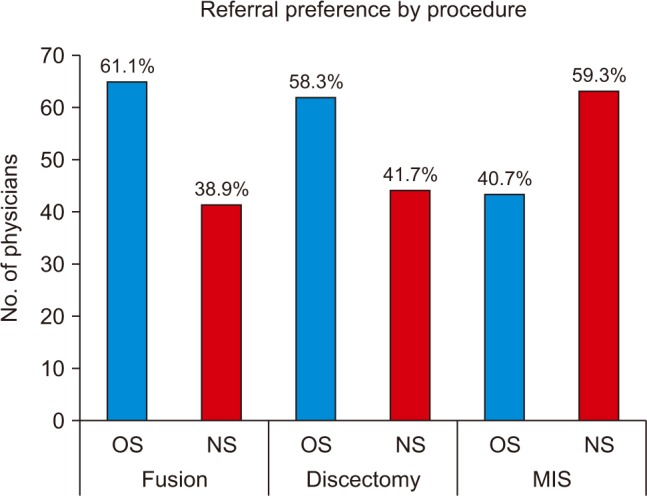
Overall, 108 physicians (24%) completed our survey. Fifty-seven physicians (52.8%) felt that neurosurgeons would provide better long-term comprehensive spinal care. Overall, 66.7% of physicians would refer to neurosurgery for cervical spine radiculopathy; 52.8%, to neurosurgery for thoracic spine radiculopathy; and 56.5%, to orthopedics for lumbar spine radiculopathy. Most physicians would refer all spine fractures to orthopedics for treatment except cervical spine fractures (56.5% to neurosurgeons). Most physicians would refer to neurosurgery for extradural tumors (91.7%) and intradural tumors (96.3%). Most would refer to orthopedic surgeons for chronic pain. Finally, physicians would refer to orthopedics for spine fusion (61.1%) and discectomy (58.3%) and to neurosurgery for minimally invasive surgery (59.3%).
CONCLUSIONS
Even though both orthopedic surgeons and neurosurgeons are intensively trained to treat a similar breath of spinal pathology, physicians vary in their referring patterns according to spinal pathology, location of pathology, and intended surgery. Education on the role of spine surgeons among PCPs is essential in ensuring unbiased referral patterns.
Keyword
MeSH Terms
Figure
Reference
-
1. Marketos SG, Skiadas P. Hippocrates: the father of spine surgery. Spine (Phila Pa 1976). 1999; 24(13):1381–1387. PMID: 10404583.2. Tarpada SP, Morris MT, Burton DA. Spinal fusion surgery: a historical perspective. J Orthop. 2017; 14(1):134–136. PMID: 27872518.
Article3. Hoy D, March L, Brooks P, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014; 73(6):968–974. PMID: 24665116.
Article4. Davis H. Increasing rates of cervical and lumbar spine surgery in the United States, 1979–1990. Spine (Phila Pa 1976). 1994; 19(10):1117–1123. PMID: 8059266.
Article5. Agency for Healthcare Research and Quality. Healthcare cost and utilization project, HCUPnet [Internet]. Rockville, MD: Agency for Healthcare Research and Quality;cited 2019 Dec 14. Available from: http://www.ahrq.gov/data/hcup/.6. Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States' trends and regional variations in lumbar spine surgery: 1992–2003. Spine (Phila Pa 1976). 2006; 31(23):2707–2714. PMID: 17077740.
Article7. Atlas SJ, Deyo RA. Evaluating and managing acute low back pain in the primary care setting. J Gen Intern Med. 2001; 16(2):120–131. PMID: 11251764.
Article8. Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010; 19(12):2075–2094. PMID: 20602122.
Article9. Dvorak MF, Collins JB, Murnaghan L, et al. Confidence in spine training among senior neurosurgical and orthopedic residents. Spine (Phila Pa 1976). 2006; 31(7):831–837. PMID: 16582858.
Article10. Daniels AH, Ames CP, Smith JS, Hart RA. Variability in spine surgery procedures performed during orthopaedic and neurological surgery residency training: an analysis of ACGME case log data. J Bone Joint Surg Am. 2014; 96(23):e196. PMID: 25471922.11. Herkowitz HN, Connolly PJ, Gundry CR, Varlotta GP, Zdeblick TA, Truumees E. Resident and fellowship guidelines: educational guidelines for resident training in spinal surgery. Spine (Phila Pa 1976). 2000; 25(20):2703–2707. PMID: 11034660.12. Raja Rampersaud Y, Fisher C, Wilsey J, et al. Agreement between orthopedic surgeons and neurosurgeons regarding a new algorithm for the treatment of thoracolumbar injuries: a multicenter reliability study. J Spinal Disord Tech. 2006; 19(7):477–482. PMID: 17021410.13. Grauer JN, Vaccaro AR, Beiner JM, et al. Similarities and differences in the treatment of spine trauma between surgical specialties and location of practice. Spine (Phila Pa 1976). 2004; 29(6):685–696. PMID: 15014280.
Article14. Epstein NE, Schwall G, Reillly T, Insinna T, Bahnken A, Hood DC. Surgeon choices, and the choice of surgeons, affect total hospital charges for single-level anterior cervical surgery. Spine (Phila Pa 1976). 2011; 36(11):905–909. PMID: 20890263.
Article15. Hijji FY, Narain AS, Haws BE, et al. Variation in spine surgeon selection criteria between neurosurgery and orthopedic surgery patients. Clin Spine Surg. 2018; 31(2):E127–E132. PMID: 28945643.
Article16. Manning BT, Ahn J, Bohl DD, Mayo BC, Louie PK, Singh K. Spine Surgeon Selection Criteria: Factors Influencing Patient Choice. Spine (Phila Pa 1976). 2016; 41(13):E814–E819. PMID: 26656051.
Article17. Harris KM. How do patients choose physicians? Evidence from a national survey of enrollees in employment-related health plans. Health Serv Res. 2003; 38(2):711–732. PMID: 12785569.
Article19. Mulholland RC, Clamp JC, Boszczyk BM. A short history of spinal training and outlook on spine speciality development in the UK 1948–2013. Eur Spine J. 2013; 22 Suppl 1:S1–S4. PMID: 23328876.
Article20. Eismont FJ. The education, training, and evaluation of a spine surgeon. Spine (Phila Pa 1976). 1996; 21(18):2059–2063. PMID: 8893427.
Article21. Kellerman SE, Herold J. Physician response to surveys: a review of the literature. Am J Prev Med. 2001; 20(1):61–67.
Article22. Cummings SM, Savitz LA, Konrad TR. Reported response rates to mailed physician questionnaires. Health Serv Res. 2001; 35(6):1347–1355. PMID: 11221823.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influence of Physician-Rating Websites on Patient Physician Preference
- Preservation Versus Elimination of Segmental Motion in Anterior Cervical Spine Surgery
- Korean Journal of Spine, the Long History of Archives of Spine Academia and the Beginning of a New Era
- Concepts and Techniques to Prevent Cervical Spine Deformity After Spine Surgery: A Narrative Review
- Commentary on “History of Spinal Neurosurgery and Spine Societies”