Korean J Gastroenterol.
2019 Dec;74(6):356-361. 10.4166/kjg.2019.74.6.356.
Magnetic Resonance Imaging Findings of Biliary Adenofibroma
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiological Science, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. kimkw@amc.seoul.kr
- 3Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 5Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2469911
- DOI: http://doi.org/10.4166/kjg.2019.74.6.356
Abstract
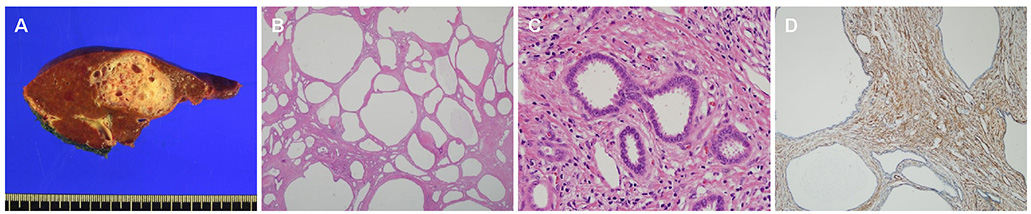
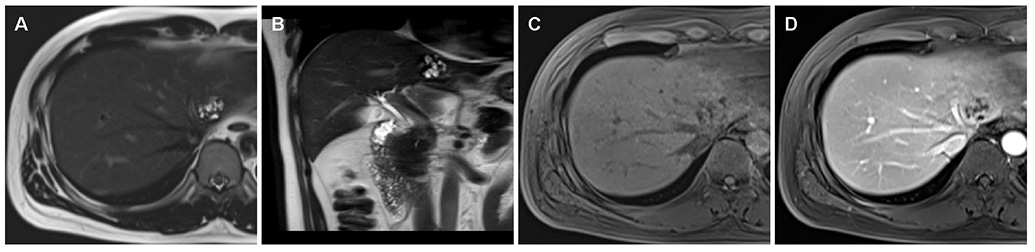
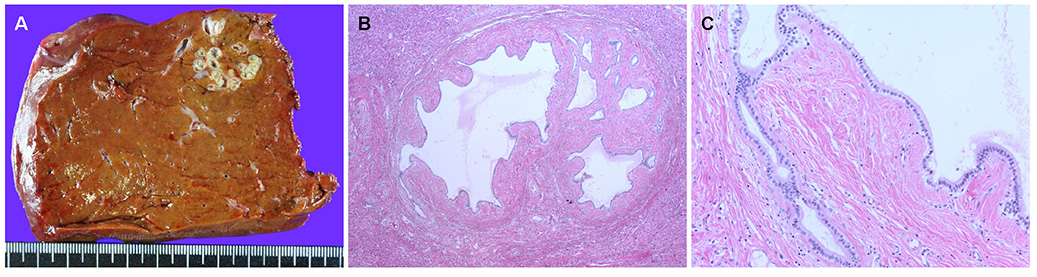
- Biliary adenofibroma is a rare tumor with a bile duct origin characterized by a complex tubulocystic non-mucin secreting biliary epithelium with abundant fibrous stroma. The MRI features of biliary adenofibroma are not well established. The authors encountered two patients with biliary adenofibroma and reviewed the literature focusing on the MRI findings. A well-circumscribed multicystic tumor with septal enhancement and no intrahepatic bile duct communication may be the characteristic MRI findings of biliary adenofibroma.
Keyword
MeSH Terms
Figure
Reference
-
1. Tsui WM, Loo KT, Chow LT, Tse CC. Biliary adenofibroma. A heretofore unrecognized benign biliary tumor of the liver. Am J Surg Pathol. 1993; 17:186–192.2. Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. 4th ed. Lyon: IARC Press;2010.3. Parada LA, Bardi G, Hallén M, et al. Monosomy 22 in a case of biliary adenofibroma. Cancer Genet Cytogenet. 1997; 93:183–184.4. Haberal AN, Bilezikci B, Demirhan B, Karakayali H, Haberal M. Malignant transformation of biliary adenofibroma: a case report. Turk J Gastroenterol. 2001; 12:149–153.5. Akin O, Coskun M. Biliary adenofibroma with malignant transformation and pulmonary metastases: CT findings. AJR Am J Roentgenol. 2002; 179:280–281.6. Garduño-López AL, Mondragón-Sánchez R, Bernal-Maldonado R, Hinojosa-Becerril CA, Meneses-García A. A case of biliary adenofibroma of the liver causing elevated serum CA 19-9 levels. Rev Oncol. 2002; 4:271–273.7. Varnholt H, Vauthey JN, Dal Cin P, et al. Biliary adenofibroma: a rare neoplasm of bile duct origin with an indolent behavior. Am J Surg Pathol. 2003; 27:693–698.8. Gurrera A, Alaggio R, Leone G, Aprile G, Magro G. Biliary adenofibroma of the liver: report of a case and review of the literature. Patholog Res Int. 2010; 2010:504584.9. Kai K, Yakabe T, Kohya N, et al. A case of unclassified multicystic biliary tumor with biliary adenofibroma features. Pathol Int. 2012; 62:506–510.10. Nguyen NT, Harring TR, Holley L, Goss JA, O'Mahony CA. Biliary adenofibroma with carcinoma in situ: a rare case report. Case Reports Hepatol. 2012; 2012:793963.11. Tsutsui A, Bando Y, Sato Y, et al. Biliary adenofibroma with ominous features of imminent malignant changes. Clin J Gastroenterol. 2014; 7:441–448.12. Thai E, Dalla Valle R, Evaristi F, Silini EM. A case of biliary adenofibroma with malignant transformation. Pathol Res Pract. 2016; 212:468–470.13. Elpek GÖ, Ünal B, BaXMLLink_XYZsorgun CXMLLink_XYZ, Ayik E. A problematic case of unclassified multicystic biliary tumor with adenofibroma features. Turk Patoloji Derg. 2016; 32:60–62.14. Godambe A, Brunt EM, Fulling KH, Reza Kermanshahi T. Biliary adenofibroma with invasive carcinoma: case report and review of the literature. Case Rep Pathol. 2016; 2016:8068513.15. Thompson SM, Zendejas-Mummert B, Hartgers ML, et al. Malignant transformation of biliary adenofibroma: a rare biliary cystic tumor. J Gastrointest Oncol. 2016; 7:E107–E112.16. Kaminsky P, Preiss J, Sasatomi E, Gerber DA. Biliary adenofibroma: a rare hepatic lesion with malignant features. Hepatology. 2017; 65:380–383.17. Arnason T, Borger DR, Corless C, et al. Biliary adenofibroma of liver: morphology, tumor genetics, and outcomes in 6 cases. Am J Surg Pathol. 2017; 41:499–505.18. Chua D, Chiow AKH, Ang TL, Wang LM. Malignant transformation arising within unusual and rare hepatic lesions: fibropolycystic disease form of ductal plate malformation and biliary adenofibroma. Int J Surg Pathol. 2018; 26:542–550.19. Esteban M, Amin J, Hertl M, Jakate S, Singh A. Double trouble: a rare case of concurrent biliary adenofibroma and hepatobiliary mucinous cystic neoplasm. ACG Case Rep J. 2018; 5:e72.20. Joo I, Lee JM, Yoon JH. Imaging diagnosis of intrahepatic and perihilar cholangiocarcinoma: recent advances and challenges. Radiology. 2018; 288:7–13.21. Lee S, Kim MJ, Kim S, Choi D, Jang KT, Park YN. Intraductal papillary neoplasm of the bile duct: assessment of invasive carcinoma and long-term outcomes using MRI. J Hepatol. 2019; 70:692–699.22. Park HJ, Kim SY, Kim HJ, et al. Intraductal papillary neoplasm of the bile duct: clinical, imaging, and pathologic features. AJR Am J Roentgenol. 2018; 211:67–75.23. Hong GS, Byun JH, Kim JH, et al. Thread sign in biliary intraductal papillary mucinous neoplasm: a novel specific finding for MRI. Eur Radiol. 2016; 26:3112–3120.24. Soares KC, Arnaoutakis DJ, Kamel I, et al. Cystic neoplasms of the liver: biliary cystadenoma and cystadenocarcinoma. J Am Coll Surg. 2014; 218:119–128.25. Lewin M, Mourra N, Honigman I, et al. Assessment of MRI and MRCP in diagnosis of biliary cystadenoma and cystadenocarcinoma. Eur Radiol. 2006; 16:407–413.26. Kim HJ, Yu ES, Byun JH, et al. CT differentiation of mucin-producing cystic neoplasms of the liver from solitary bile duct cysts. AJR Am J Roentgenol. 2014; 202:83–91.27. Pakala T, Molina M, Wu GY. Hepatic echinococcal cysts: a review. J Clin Transl Hepatol. 2016; 4:39–46.28. Qian LJ, Zhu J, Zhuang ZG, Xia Q, Liu Q, Xu JR. Spectrum of multilocular cystic hepatic lesions: CT and MR imaging findings with pathologic correlation. Radiographics. 2013; 33:1419–1433.29. WHO Classification of Tumours Editorial Board. WHO classification of tumours of the digestive system. 5th ed. Lyon: IARC Press;2019.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Ultrasound and MRI Findings of Uterine Adenofibroma: A Case Report
- A Case Report of Cholangiocarcinoma Arising from a Biliary Adenofibroma: Radiologic Findings and Review of Literature
- Diagnostic Approach to Indeterminate Biliary Stricture
- A Case of Uterine Adenofibroma
- MR Imaging Findings of Ovarian Cystadenofibroma: Clues for Making the Differential Diagnosis from Ovarian Malignancy