Ann Surg Treat Res.
2020 Feb;98(2):62-71. 10.4174/astr.2020.98.2.62.
What are the most important predictive factors for clinically relevant posthepatectomy liver failure after right hepatectomy for hepatocellular carcinoma?
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. CHOIGH@yuhs.ac
- 2Division of Surgical Oncology, Department of Surgery, Vicente Sotto Memorial Medical Center, Cebu, the Philippines.
- KMID: 2469105
- DOI: http://doi.org/10.4174/astr.2020.98.2.62
Abstract
- PURPOSE
The risk of posthepatectomy liver failure (PHLF) after right hepatectomy remains substantial. Additional parameters such as computed tomography volumetry, liver stiffness measurement by FibroScan, indocyanine green retention rate at 15 minutes, and platelet count used to properly assess future liver remnant volume quality and quantity are of the utmost importance. Thus, we compared the usefulness of these modalities for predicting PHLF among patients with hepatocellular carcinoma after right hepatectomy.
METHODS
We retrospectively reviewed patients who underwent right hepatectomy for hepatocellular carcinoma between 2007 and 2013. PHLF was determined according to International Study Group of Liver Surgery consensus definition and severity grading. Grades B and C were defined as clinically relevant posthepatectomy liver failure (CRPHLF). The results were internally validated using a cohort of 97 patients.
RESULTS
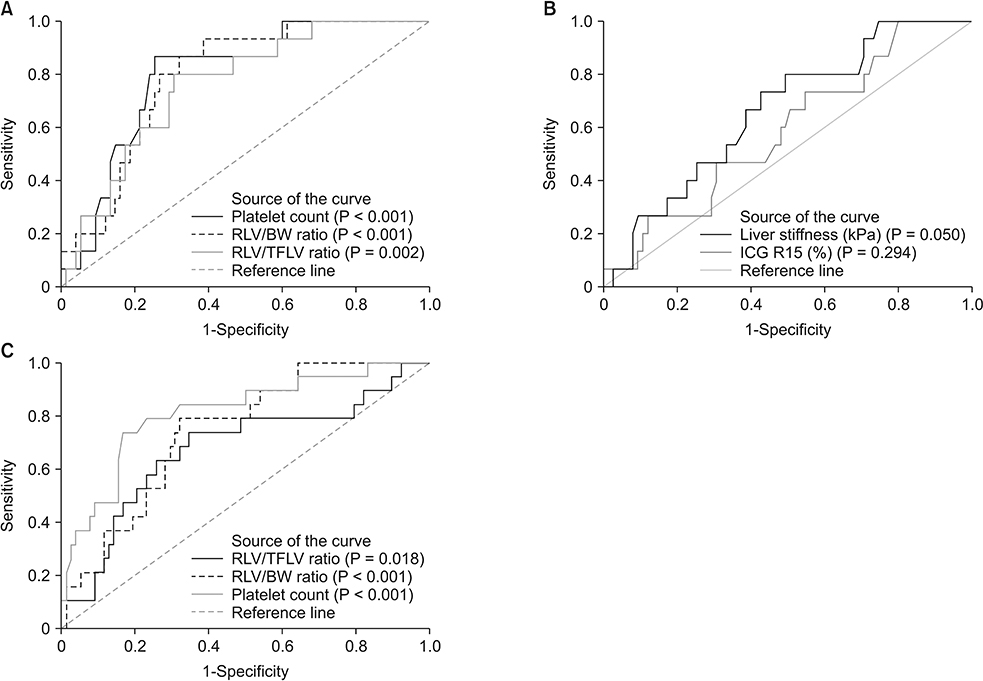
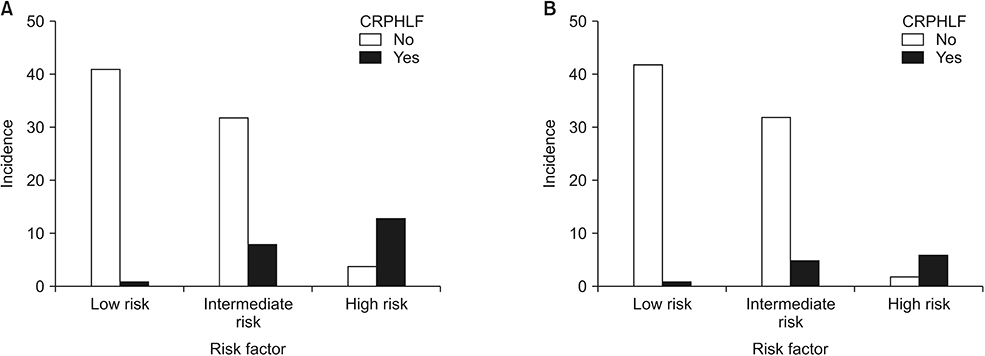
Among the 90 included patients, 15 (16.7%) had CRPHLF. Multivariate analysis confirmed that platelet count < 140 (109/L) (hazard ratio [HR], 24.231; 95% confidence interval [CI], 3.623-161.693; P = 0.001) and remnant liver volume-to-body weight (RVL/BW) ratio < 0.55 (HR, 25.600; 95% CI, 4.185-156.590; P < 0.001) were independent predictors of CRPHLF. Among the 12 patients with a platelet count < 140 (109/L) and RLV/BW ratio < 0.55, 9 (75%) had CRPHLF. Likewise, 5 of 38 (13.2%) with only one risk factor developed CRPHL versus 1 of 40 (2.5%) with no risk factors. These findings were confirmed by the validation cohort.
CONCLUSION
RLV/BW ratio and platelet count are more important than the conventional RLV/TFLV, indocyanine green retention rate at 15 minutes, and liver stiffness measurement in the preoperative risk assessment for CRPHLF.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Robotic major liver resections: Surgical outcomes compared with open major liver resections
Hye Yeon Yang, Seoung Yoon Rho, Dai Hoon Han, Jin Sub Choi, Gi Hong Choi
Ann Hepatobiliary Pancreat Surg. 2021;25(1):8-17. doi: 10.14701/ahbps.2021.25.1.8.
Reference
-
1. Allen PJ, Jarnagin WR. Current status of hepatic resection. Adv Surg. 2003; 37:29–49.2. Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 2002; 236:397–406.3. van den Broek MA, Olde Damink SW, Dejong CH, Lang H, Malago M, Jalan R, et al. Liver failure after partial hepatic resection: definition, pathophysiology, risk factors and treatment. Liver Int. 2008; 28:767–780.
Article4. Mullen JT, Ribero D, Reddy SK, Donadon M, Zorzi D, Gautam S, et al. Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg. 2007; 204:854–862.
Article5. Cauchy F, Soubrane O, Belghiti J. Liver resection for HCC: patient’s selection and controversial scenarios. Best Pract Res Clin Gastroenterol. 2014; 28:881–896.
Article6. Lin XJ, Yang J, Chen XB, Zhang M, Xu MQ. The critical value of remnant liver volume-to-body weight ratio to estimate posthepatectomy liver failure in cirrhotic patients. J Surg Res. 2014; 188:489–495.
Article7. Truant S, Oberlin O, Sergent G, Lebuffe G, Gambiez L, Ernst O, et al. Remnant liver volume to body weight ratio > or =0.5%: a new cut-off to estimate postoperative risks after extended resection in noncirrhotic liver. J Am Coll Surg. 2007; 204:22–33.8. Manizate F, Hiotis SP, Labow D, Roayaie S, Schwartz M. Liver functional reserve estimation: state of the art and relevance for local treatments: the Western perspective. J Hepatobiliary Pancreat Sci. 2010; 17:385–388.9. Yokoyama Y, Nishio H, Ebata T, Igami T, Sugawara G, Nagino M. Value of indocyanine green clearance of the future liver remnant in predicting outcome after resection for biliary cancer. Br J Surg. 2010; 97:1260–1268.
Article10. Yokoyama Y, Ebata T, Igami T, Sugawara G, Mizuno T, Yamaguchi J, et al. The Predictive value of indocyanine green clearance in future liver remnant for posthepatectomy liver failure following hepatectomy with extrahepatic bile duct resection. World J Surg. 2016; 40:1440–1447.
Article11. Kim JM, Kwon CH, Joh JW, Park JB, Lee JH, Kim GS, et al. Can the model for end-stage liver disease score replace the indocyanine green clearance test in the selection of right hemihepatectomy in Child-Pugh class A? Ann Surg Treat Res. 2014; 86:122–129.
Article12. Venkat R, Hannallah JR, Krouse RS, Maegawa FB. Preoperative thrombocytopenia and outcomes of hepatectomy for hepatocellular carcinoma. J Surg Res. 2016; 201:498–505.
Article13. Pavlov CS, Casazza G, Nikolova D, Tsochatzis E, Burroughs AK, Ivashkin VT, et al. Transient elastography for diagnosis of stages of hepatic fibrosis and cirrhosis in people with alcoholic liver disease. Cochrane Database Syst Rev. 2015; 1:CD010542.
Article14. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.15. Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011; 149:713–724.
Article16. Shirabe K, Shimada M, Gion T, Hasegawa H, Takenaka K, Utsunomiya T, et al. Postoperative liver failure after major hepatic resection for hepatocellular carcinoma in the modern era with special reference to remnant liver volume. J Am Coll Surg. 1999; 188:304–309.
Article17. Schindl MJ, Redhead DN, Fearon KC, Garden OJ, Wigmore SJ. Edinburgh Liver Surgery and Transplantation Experimental Research Group (eLISTER). The value of residual liver volume as a predictor of hepatic dysfunction and infection after major liver resection. Gut. 2005; 54:289–296.
Article18. Abdalla EK, Denys A, Chevalier P, Nemr RA, Vauthey JN. Total and segmental liver volume variations: implications for liver surgery. Surgery. 2004; 135:404–410.
Article19. Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012; 255:405–414.
Article20. Torzilli G, Makuuchi M, Inoue K, Takayama T, Sakamoto Y, Sugawara Y, et al. No-mortality liver resection for hepatocellular carcinoma in cirrhotic and noncirrhotic patients: is there a way? A prospective analysis of our approach. Arch Surg. 1999; 134:984–992.21. Fan ST, Lai EC, Lo CM, Ng IO, Wong J. Hospital mortality of major hepatectomy for hepatocellular carcinoma associated with cirrhosis. Arch Surg. 1995; 130:198–203.
Article22. Cescon M, Colecchia A, Cucchetti A, Peri E, Montrone L, Ercolani G, et al. Value of transient elastography measured with FibroScan in predicting the outcome of hepatic resection for hepatocellular carcinoma. Ann Surg. 2012; 256:706–712.
Article23. Kim SU, Ahn SH, Park JY, Kim DY, Chon CY, Choi JS, et al. Prediction of postoperative hepatic insufficiency by liver stiffness measurement (FibroScan((R))) before curative resection of hepatocellular carcinoma: a pilot study. Hepatol Int. 2008; 2:471–477.24. Zhang Z, Zhang Y, Wang W, Hua Y, Liu L, Shen S, et al. Thrombocytopenia and the outcomes of hepatectomy for hepatocellular carcinoma: a meta-analysis. J Surg Res. 2017; 210:99–107.
Article25. Mehrabi A, Golriz M, Khajeh E, Ghamarnejad O, Probst P, Fonouni H, et al. Meta-analysis of the prognostic role of perioperative platelet count in posthepatectomy liver failure and mortality. Br J Surg. 2018; 105:1254–1261.
Article26. Lim JH, Choi GH, Choi SH, Lee HS, Kim KS, Choi JS. Ventral segment-preserving right hepatectomy in patients with hepatocellular carcinoma. World J Surg. 2015; 39:1034–1043.
Article27. Satou S, Sugawara Y, Tamura S, Yamashiki N, Kaneko J, Aoki T, et al. Discrepancy between estimated and actual weight of partial liver graft from living donors. J Hepatobiliary Pancreat Sci. 2011; 18:586–591.
Article28. Mussin N, Sumo M, Lee KW, Choi Y, Choi JY, Ahn SW, et al. The correlation between preoperative volumetry and real graft weight: comparison of two volumetry programs. Ann Surg Treat Res. 2017; 92:214–220.
Article29. Chapelle T, Op De Beeck B, Huyghe I, Francque S, Driessen A, Roeyen G, et al. Future remnant liver function estimated by combining liver volumetry on magnetic resonance imaging with total liver function on (99m)Tc-mebrofenin hepatobiliary scintigraphy: can this tool predict post-hepatectomy liver failure? HPB (Oxford). 2016; 18:494–503.30. Kim DK, Choi JI, Choi MH, Park MY, Lee YJ, Rha SE, et al. Prediction of posthepatectomy liver failure: MRI with hepatocyte-specific contrast agent versus indocyanine green clearance test. AJR Am J Roentgenol. 2018; 211:580–587.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two-Stage Hepatectomy for Bilateral Hepatocellular Carcinoma with Bile Duct Tumor Thrombi
- Prognostic Factors and Clinicopathologic Features after Resection of Small Hepatocellular Carcinoma (< or =2 cm)
- Associating microwave ablation and portal vein ligation for staged hepatectomy for the treatment of huge hepatocellular carcinoma with cirrhosis
- Predictors of post-hepatectomy liver failure in patients undergoing extensive liver resections for hepatocellular carcinoma
- Liver resection after sorafenib therapy in advanced hepatocellular carcinoma: a case report