Ann Rehabil Med.
2019 Dec;43(6):725-729. 10.5535/arm.2019.43.6.725.
Secondary Lymphedema After Intestinal Tuberculosis: A Case Report
- Affiliations
-
- 1Department of Rehabilitation Medicine, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea. yjk5289@naver.com
- KMID: 2468699
- DOI: http://doi.org/10.5535/arm.2019.43.6.725
Abstract
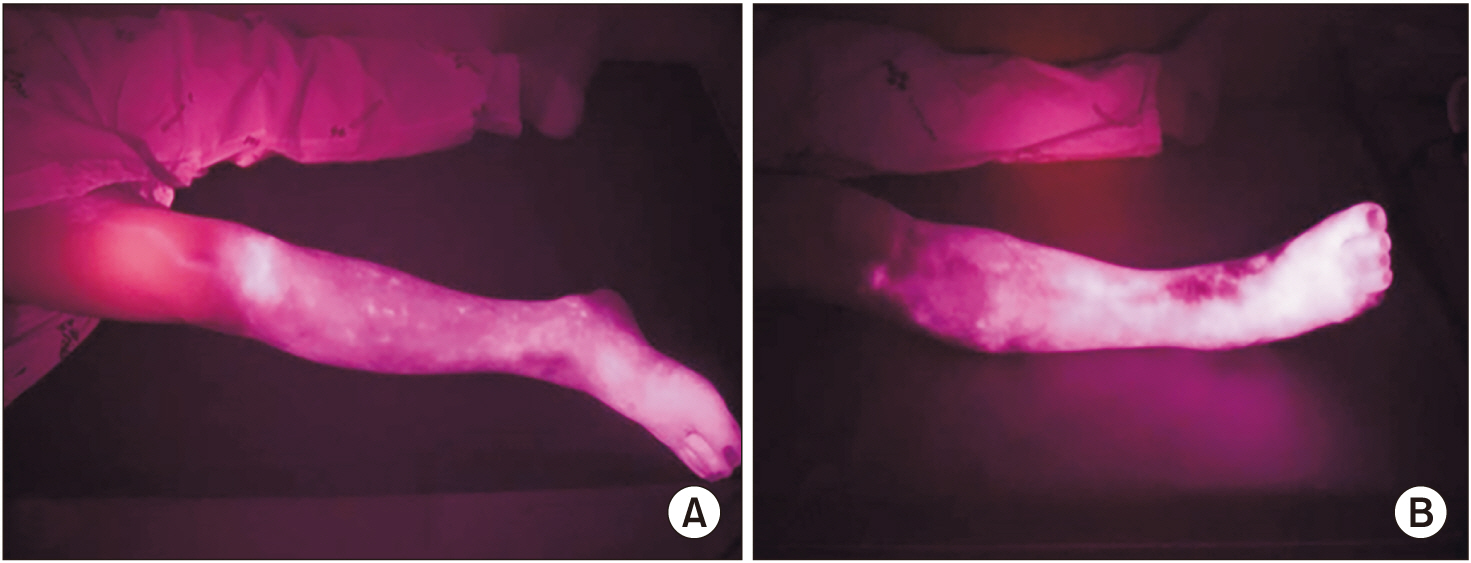
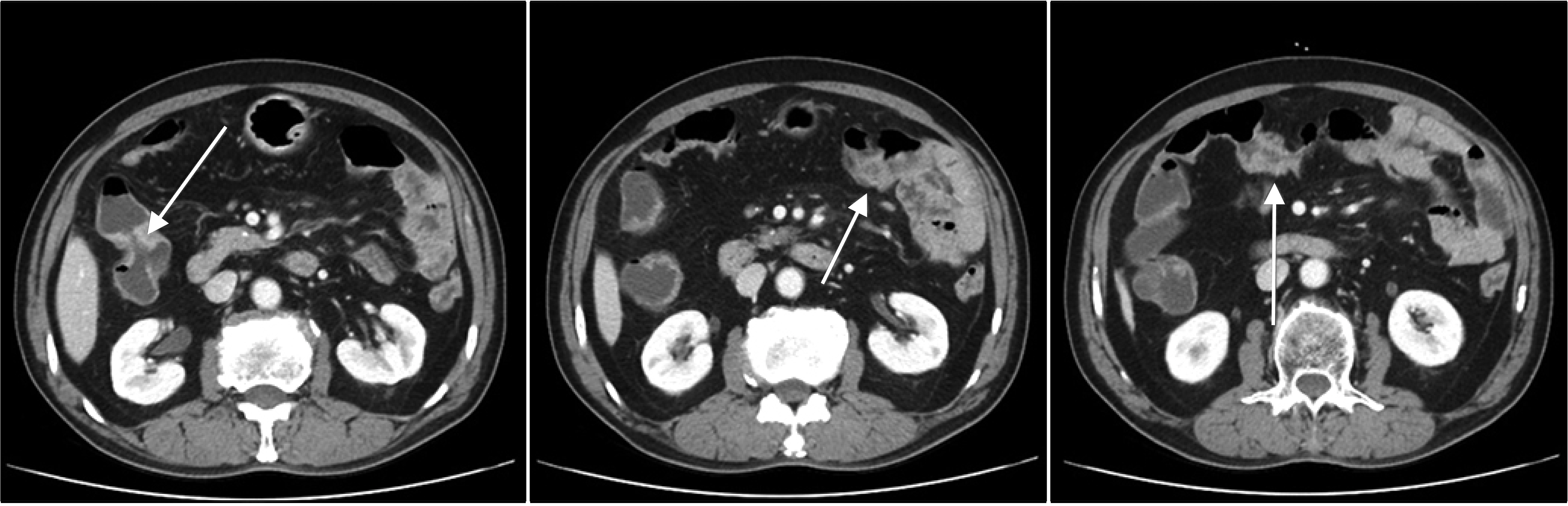
- Lymphedema, a chronic disease that lowers patients' quality of life, is categorized as primary or secondary. Secondary lymphedema can be improved by treating the underlying cause. However, in many cases, efforts are not made to identify the primary cause of lymphedema and treatment is targeted at the edema itself, resulting in misdiagnosis. Here, we describe the case of a 61-year-old man with right leg edema of unknown cause that had persisted for 3 years. Intestinal tuberculosis was confirmed during a re-evaluation of the cause, and his symptoms improved after anti-tuberculous treatment. This improvement was assessed qualitatively by indocyanine green lymphography before and after treatment, as well as by observation of the clinical symptoms. Lower extremity lymphedema caused by intestinal tuberculosis is extremely rare, and this case reveals the importance of continuing to identify the causes of resistant pathologies.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee SY, Pack YJ, Kim HS, Min DJ, Kim WU. A case of lymphedema associated with juvenile rheumatoid arthritis. Korean J Med. 2008; 74:S239–44.2. Sim YJ, Seo JH, Ko MH, Jung SH. Post traumatic chronic lymphedema: a case report. J Korean Acad Rehabil Med. 2007; 31:261–4.3. Kang SH, Sim YJ, Jeong HJ, Kim GC. Acute lymphedema after coronary angiography: a case report. J Korean Acad Rehabil Med. 2010; 34:767–70.4. Arrault M, Blanchard M, Vignes S. Inflammatory bowel disease and lower limb lymphedema: a fortuitous association? Rev Med Interne. 2011; 32:43–5.5. Hoda S, Rab SM. Two cases of tuberculous lymphoedema. Br Med J. 1974; 3:786.
Article6. Abramowitz I. Secondary lymphoedema. S Afr J Surg. 1970; 8:57–9.7. Becker F, Yi P, Al-Kofahi M, Ganta VC, Morris J, Alexander JS. Lymphatic dysregulation in intestinal inflammation: new insights into inflammatory bowel disease pathomechanisms. Lymphology. 2014; 47:3–27.8. Sato S, Yao K, Yao T, Schlemper RJ, Matsui T, Sakurai T, et al. Colonoscopy in the diagnosis of intestinal tuberculosis in asymptomatic patients. Gastrointest Endosc. 2004; 59:362–8.
Article9. Yamamoto T, Matsuda N, Doi K, Oshima A, Yoshimatsu H, Todokoro T, et al. The earliest finding of indocyanine green lymphography in asymptomatic limbs of lower extremity lymphedema patients secondary to cancer treatment: the modified dermal backflow stage and concept of subclinical lymphedema. Plast Reconstr Surg. 2011; 128:314e–321e.10. Narushima M, Yamamoto T, Ogata F, Yoshimatsu H, Mihara M, Koshima I. Indocyanine green lymphography findings in limb lymphedema. J Reconstr Microsurg. 2016; 32:72–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Hepatic Tuberculosis Secondary to Intestinal Tuberculosis
- A Case of Conjunctival and Lid Lymphedema Confirmed with Lymphoscintigraphy
- Lymphaticovenous Anastomosis in Lower Extremity Lymphedema: A Case Report
- Secondary Lymphedema after Femoral Venous Catheterization
- A Case of Vulvar Lymphangiectasia secondary to Primary Lymphedema