Yonsei Med J.
2020 Feb;61(2):161-168. 10.3349/ymj.2020.61.2.161.
Core-Needle Biopsy Does Not Show Superior Diagnostic Performance to Fine-Needle Aspiration for Diagnosing Thyroid Nodules
- Affiliations
-
- 1Department of Radiology, Severance Hospital, Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul, Korea. docjin@yuhs.ac
- 2Biostatistics Collaboration Unit, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2468491
- DOI: http://doi.org/10.3349/ymj.2020.61.2.161
Abstract
- PURPOSE
To compare the diagnostic performances of fine-needle aspiration (FNA) and core-needle biopsy (CNB) for thyroid nodules according to nodule size.
MATERIALS AND METHODS
This retrospective study included 320 thyroid nodules from 320 patients who underwent both FNA and CNB at outside clinics and proceeded with surgery in our institution between July 2012 and May 2019. According to nodule size, the diagnostic performances of FNA and CNB were calculated using various combinations of test-negatives and test-positives defined by the Bethesda categories and were compared using the generalized estimated equation and the Delong method.
RESULTS
There were 279 malignant nodules in 279 patients and 41 benign nodules in 41 patients. The diagnostic performance of FNA was mostly not different from CNB regardless of nodule size, except for negative predictive value, which was better for FNA than CNB when applying Criteria 1 and 2. When applying Criteria 3, the specificity and positive predictive value of FNA were superior to CNB regardless of size. When applying Criteria 4, diagnostic performance did not differ between FNA and CNB regardless of size. After applying Criteria 5, diagnostic performance did not differ between FNA and CNB in nodules ≥2 cm. However, in nodules ≥1 cm and all nodules, the sensitivity, accuracy, and negative predictive value of CNB were better than those of FNA.
CONCLUSION
CNB did not show superior diagnostic performance to FNA for diagnosing thyroid nodules.
MeSH Terms
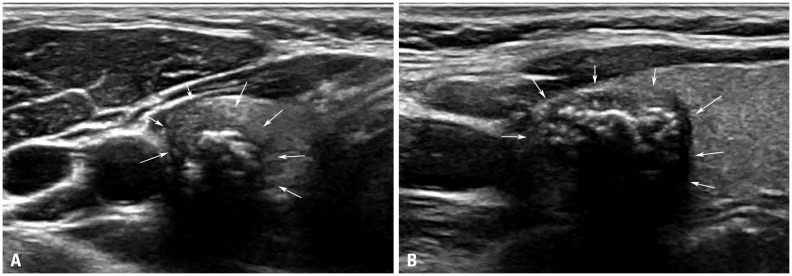
Figure
Reference
-
1. Kim SY, Lee HS, Moon J, Kim EK, Moon HJ, Yoon JH, et al. Fine-needle aspiration versus core needle biopsy for diagnosis of thyroid malignancy and neoplasm: a matched cohort study. Eur Radiol. 2017; 27:801–811. PMID: 27260342.
Article2. Ha EJ, Suh CH, Baek JH. Complications following ultrasound-guided core needle biopsy of thyroid nodules: a systematic review and meta-analysis. Eur Radiol. 2018; 28:3848–3860. PMID: 29589112.
Article3. Park KT, Ahn SH, Mo JH, Park YJ, Park DJ, Choi SI, et al. Role of core needle biopsy and ultrasonographic finding in management of indeterminate thyroid nodules. Head Neck. 2011; 33:160–165. PMID: 20848434.
Article4. Sung JY, Na DG, Kim KS, Yoo H, Lee H, Kim JH, et al. Diagnostic accuracy of fine-needle aspiration versus core-needle biopsy for the diagnosis of thyroid malignancy in a clinical cohort. Eur Radiol. 2012; 22:1564–1572. PMID: 22415411.
Article5. Yeon JS, Baek JH, Lim HK, Ha EJ, Kim JK, Song DE, et al. Thyroid nodules with initially nondiagnostic cytologic results: the role of core-needle biopsy. Radiology. 2013; 268:274–280. PMID: 23525204.
Article6. Paja M, del Cura JL, Zabala R, Corta I, Lizarraga A, Oleaga A, et al. Ultrasound-guided core-needle biopsy in thyroid nodules. A study of 676 consecutive cases with surgical correlation. Eur Radiol. 2016; 26:1–8. PMID: 25956937.
Article7. Suh CH, Baek JH, Park C, Choi YJ, Lee JH. The role of core needle biopsy for thyroid nodules with initially indeterminate results on previous fine-needle aspiration: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2017; 38:1421–1426. PMID: 28473343.
Article8. Hong MJ, Na DG, Kim SJ, Kim DS. Role of core needle biopsy as a first-line diagnostic tool for thyroid nodules: a retrospective cohort study. Ultrasonography. 2018; 37:244–253. PMID: 29113031.
Article9. Xiong Y, Yan L, Nong L, Zheng Y, Li T. Pathological diagnosis of thyroid nodules based on core needle biopsies: comparative study between core needle biopsies and resected specimens in 578 cases. Diagn Pathol. 2019; 14:10. PMID: 30711008.
Article10. Yoon JH, Kwak JY, Moon HJ, Kim EK. Ultrasonography-guided core needle biopsy did not reduce diagnostic lobectomy for thyroid nodules diagnosed as atypia of undetermined significance/follicular lesion of undetermined significance. Ultrasound Q. 2019; 35:253–258. PMID: 30724862.
Article11. Yoon JH, Kim EK, Kwak JY, Moon HJ. Effectiveness and limitations of core needle biopsy in the diagnosis of thyroid nodules: review of current literature. J Pathol Transl Med. 2015; 49:230–235. PMID: 26018514.
Article12. Cibas ES, Ali SZ. The Bethesda System for Reporting Thyroid Cytopathology. Thyroid. 2009; 19:1159–1165. PMID: 19888858.
Article13. Lee HJ, Kim YJ, Han HY, Seo JY, Hwang CM, Kim K. Ultrasound-guided needle biopsy of large thyroid nodules: core needle biopsy yields more reliable results than fine needle aspiration. J Clin Ultrasound. 2019; 47:255–260. PMID: 30820986.
Article14. Kim HC, Kim YJ, Han HY, Yi JM, Baek JH, Park SY, et al. First-line use of core needle biopsy for high-yield preliminary diagnosis of thyroid nodules. AJNR Am J Neuroradiol. 2017; 38:357–363. PMID: 27932508.
Article15. Choi YJ, Baek JH, Suh CH, Shim WH, Jeong B, Kim JK, et al. Core-needle biopsy versus repeat fine-needle aspiration for thyroid nodules initially read as atypia/follicular lesion of undetermined significance. Head Neck. 2017; 39:361–369. PMID: 27704650.
Article16. Suh CH, Baek JH, Lee JH, Choi YJ, Kim JK, Sung TY, et al. The role of core-needle biopsy as a first-line diagnostic tool for initially detected thyroid nodules. Thyroid. 2016; 26:395–403. PMID: 26651390.
Article17. Chae IH, Kim EK, Moon HJ, Yoon JH, Park VY, Kwak JY. Ultrasound-guided fine needle aspiration versus core needle biopsy: comparison of post-biopsy hematoma rates and risk factors. Endocrine. 2017; 57:108–114. PMID: 28508192.
Article18. Chung SR, Baek JH, Lee JH, Lee YM, Sung TY, Chung KW, et al. Risk of malignancy according to the sub-classification of atypia of undetermined significance and suspicious follicular neoplasm categories in thyroid core needle biopsies. Endocr Pathol. 2019; 30:146–154. PMID: 31044350.
Article19. Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, Teefey SA, et al. ACR Thyroid Imaging, Reporting and Data System (TIRADS): white paper of the ACR TI-RADS Committee. J Am Coll Radiol. 2017; 14:587–595. PMID: 28372962.
Article20. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133. PMID: 26462967.
Article21. Yoon JH, Lee HS, Kim EK, Moon HJ, Kwak JY. Malignancy risk stratification of thyroid nodules: comparison between the Thyroid Imaging Reporting and Data System and the 2014 American Thyroid Association management guidelines. Radiology. 2016; 278:917–924. PMID: 26348102.
Article22. Jung CK, Min HS, Park HJ, Song DE, Kim JH, Park SY, et al. Pathology reporting of thyroid core needle biopsy: a proposal of the Korean Endocrine Pathology Thyroid Core Needle Biopsy Study Group. J Pathol Transl Med. 2015; 49:288–299. PMID: 26081825.
Article23. Eszlinger M, Ullmann M, Ruschenburg I, Böhme K, Görke F, Franzius C, et al. Low malignancy rates in fine-needle aspiration cytologies in a primary care setting in Germany. Thyroid. 2017; 27:1385–1392. PMID: 28982301.
Article24. Ke J, Jianyong L, Ying L, Genpeng L, Linlin S, Zhihui L, et al. The use of The Bethesda System for Reporting Thyroid Cytopathology in a Chinese population: an analysis of 13 351 specimens. Diagn Cytopathol. 2019; 47:876–880. PMID: 31074206.25. Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedüs L, et al. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association Medical guidelines for clinical practice for the diagnosis and management of thyroid nodules: executive summary of recommendations. Endocr Pract. 2010; 16:468–475. PMID: 20551008.
Article26. Schizas N, Lazopoulos A, Krimiotis D, Rallis T, Paliouras D, Gogakos A, et al. Beware of hemopneumothorax following core needle breast biopsy. Respir Med Case Rep. 2018; 25:49–51. PMID: 30013911.
Article27. Kim SY, Chung HW, Oh TS, Lee JS. Practical guidelines for ultrasound-guided core needle biopsy of soft-tissue lesions: transformation from beginner to specialist. Korean J Radiol. 2017; 18:361–369. PMID: 28246516.
Article28. Kwak JY, Kim EK, Ko KH, Yang WI, Kim MJ, Son EJ, et al. Primary thyroid lymphoma: role of ultrasound-guided needle biopsy. J Ultrasound Med. 2007; 26:1761–1765. PMID: 18029928.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thyroid Nodules with Nondiagnostic FNA Results: Role of Core Needle Biopsy
- Indications for Fine Needle Aspiration in Thyroid Nodules
- Effectiveness and Limitations of Core Needle Biopsy in the Diagnosis of Thyroid Nodules: Review of Current Literature
- Combined fine-needle aspiration with core needle biopsy for assessing thyroid nodules: a more valuable diagnostic method?
- Arterial Bleeding of a Thyroid Mass After Thyroid Fine-Needle Aspiration Biopsy: A Case Report