J Cardiovasc Imaging.
2020 Jan;28(1):21-32. 10.4250/jcvi.2019.0066.
Simultaneous Assessment of Left Ventricular Function and Coronary Artery Anatomy by Third-generation Dual-source Computed Tomography Using a Low Radiation Dose
- Affiliations
-
- 1Department of Radiology, Pusan National University School of Medicine and Medical Research Institute, Pusan National University Hospital, Busan, Korea.
- 2Department of Radiology, Pusan National University School of Medicine and Medical Research Institute, Pusan National University Yangsan Hospital, Yangsan, Korea. kschoo0618@naver.com
- 3Department of Cardiology, Kim Hae Kangil Hospital, Gimhae, Korea.
- KMID: 2468377
- DOI: http://doi.org/10.4250/jcvi.2019.0066
Abstract
- BACKGROUND
To assess left ventricular function and coronary artery simultaneously by third-generation dual-source computed tomography (CT) using a low radiation dose.
METHODS
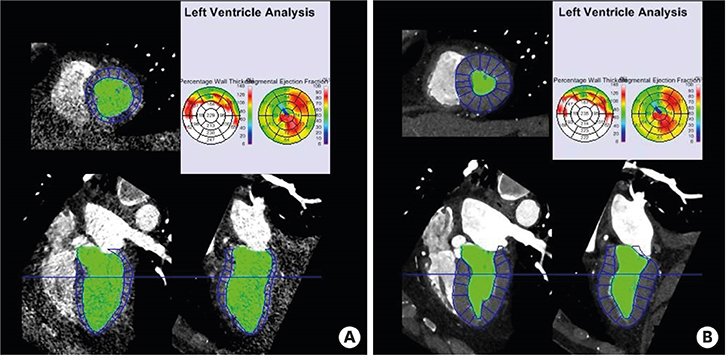
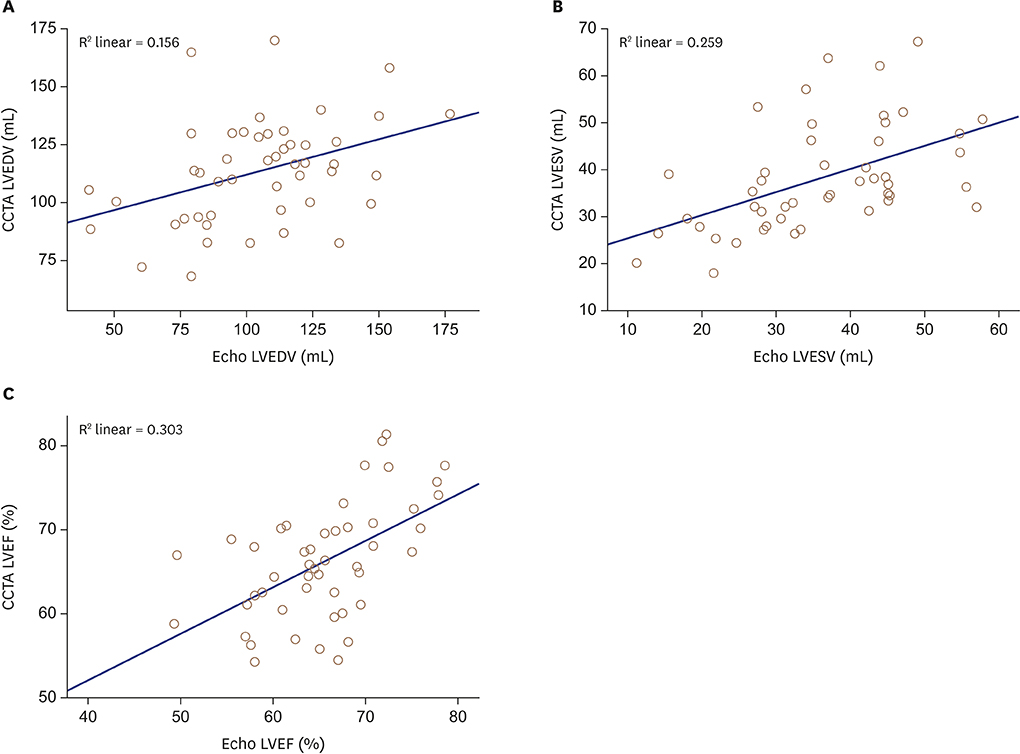
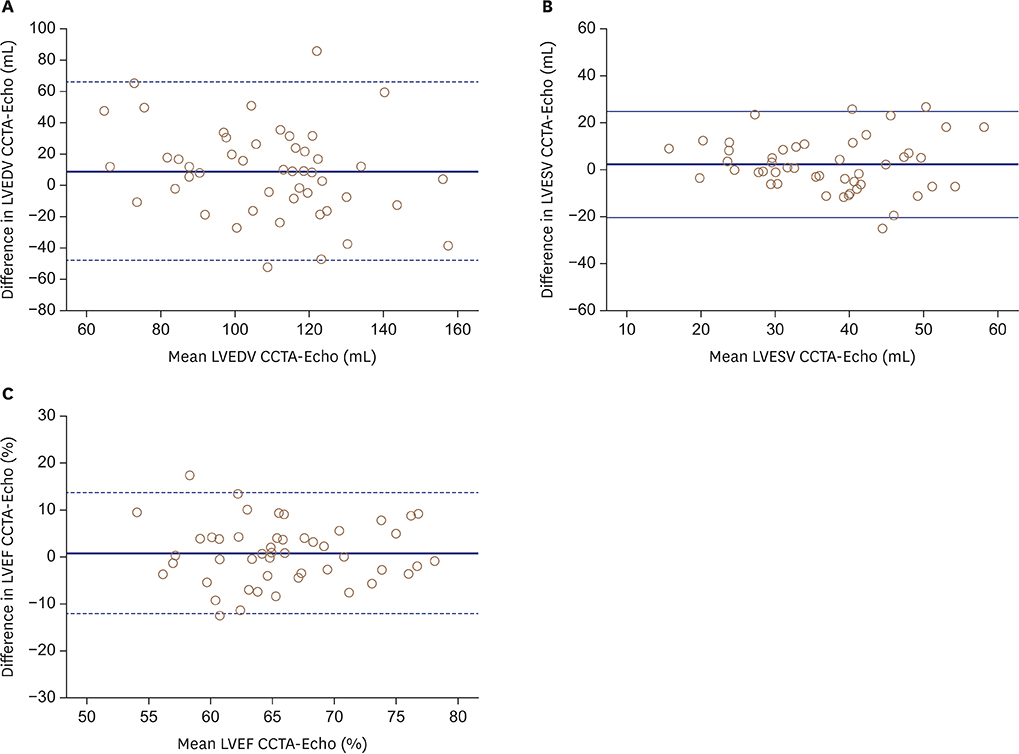
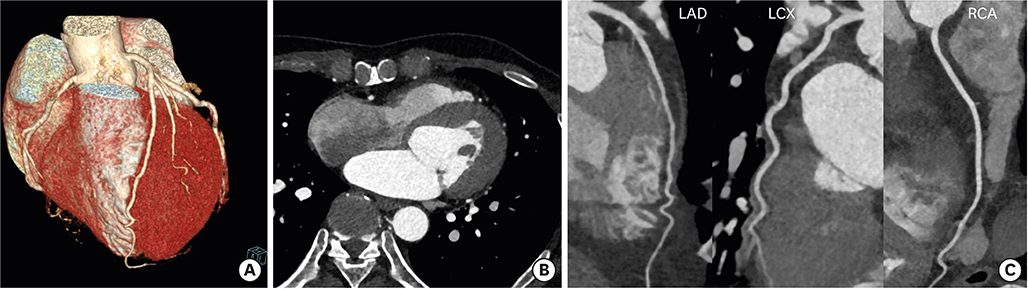
A total of 48 patients (36 men, 12 women; mean age 57.0 ± 9.5 years) who underwent both electrocardiography-gated cardiac CT angiography (CCTA) using 70-90 kVp and echocardiography were included in this retrospective study. The correlation between left ventricular end-diastolic volume (LVEDV), left ventricular end-systolic volume (LVESV), and left ventricular ejection fraction (LVEF) measured using CCTA and echocardiography was determined. The quality of coronary artery images was analyzed using a 4-point scale (1, excellent; 4, poor). The effective radiation dose of CCTA was calculated.
RESULTS
Mean heart rate during the CT examination was 59.9 ± 9.9 bpm (range 38-79) and the body mass index of 48 patients was 24.5 ± 2.6 kg/m² (range 17.0-29.4). LVEDV, LVESV, and LVEF measured using CCTA and echocardiography demonstrated a fair to moderate correlation (Pearson correlation coefficient: r = 0.395, p = 0.005 for LVEDV; r = 0.509. p < 0.001 for LVESV; r = 0.551, p < 0.001 for LVEF). Average image quality score of coronary arteries was 1.0 ± 0.1 (range 1-2). A total of 99.0% (783 of 791) of segments had an excellent image quality score, and 1.0% (8 of 791) of segments had a good score. Mean effective radiation dose was 2.2 ± 0.7 mSv.
CONCLUSIONS
Third-generation dual-source CT using a low tube voltage simultaneously provides information regarding LV function and coronary artery disease at a low radiation dose. It can serve as an alternative option for functional assessment, particularly when other imaging modalities are inadequate.
Keyword
MeSH Terms
Figure
Reference
-
1. White HD, Norris RM, Brown MA, Brandt PW, Whitlock RM, Wild CJ. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation. 1987; 76:44–51.
Article2. Norris RM, White HD, Cross DB, Wild CJ, Whitlock RM. Prognosis after recovery from myocardial infarction: the relative importance of cardiac dilatation and coronary stenoses. Eur Heart J. 1992; 13:1611–1618.
Article3. Arsanjani R, Berman DS, Gransar H, et al. Left ventricular function and volume with coronary CT angiography improves risk stratification and identification of patients at risk for incident mortality: results from 7758 patients in the prospective multinational CONFIRM observational cohort study. Radiology. 2014; 273:70–77.
Article4. Malm S, Frigstad S, Sagberg E, Larsson H, Skjaerpe T. Accurate and reproducible measurement of left ventricular volume and ejection fraction by contrast echocardiography: a comparison with magnetic resonance imaging. J Am Coll Cardiol. 2004; 44:1030–1035.5. Rizvi A, Deaño RC, Bachman DP, Xiong G, Min JK, Truong QA. Analysis of ventricular function by CT. J Cardiovasc Comput Tomogr. 2015; 9:1–12.
Article6. Dill T. Contraindications to magnetic resonance imaging: non-invasive imaging. Heart. 2008; 94:943–948.7. Ko SM, Hwang SH, Lee HJ. Role of cardiac computed tomography in the diagnosis of left ventricular myocardial diseases. J Cardiovasc Imaging. 2019; 27:73–92.
Article8. Henneman MM, Schuijf JD, Jukema JW, et al. Assessment of global and regional left ventricular function and volumes with 64-slice MSCT: a comparison with 2D echocardiography. J Nucl Cardiol. 2006; 13:480–487.
Article9. Butler J, Shapiro MD, Jassal DS, et al. Comparison of multidetector computed tomography and two-dimensional transthoracic echocardiography for left ventricular assessment in patients with heart failure. Am J Cardiol. 2007; 99:247–249.
Article10. Abbara S, Chow BJ, Pena AJ, et al. Assessment of left ventricular function with 16- and 64-slice multi-detector computed tomography. Eur J Radiol. 2008; 67:481–486.
Article11. Wu YW, Tadamura E, Kanao S, et al. Left ventricular functional analysis using 64-slice multidetector row computed tomography: comparison with left ventriculography and cardiovascular magnetic resonance. Cardiology. 2008; 109:135–142.
Article12. Greupner J, Zimmermann E, Grohmann A, et al. Head-to-head comparison of left ventricular function assessment with 64-row computed tomography, biplane left cineventriculography, and both 2- and 3-dimensional transthoracic echocardiography: comparison with magnetic resonance imaging as the reference standard. J Am Coll Cardiol. 2012; 59:1897–1907.13. Lim SJ, Choo KS, Park YH, et al. Assessment of left ventricular function and volume in patients undergoing 128-slice coronary CT angiography with ECG-based maximum tube current modulation: a comparison with echocardiography. Korean J Radiol. 2011; 12:156–162.
Article14. Bak SH, Ko SM, Jeon HJ, Yang HS, Hwang HK, Song MG. Assessment of global left ventricular function with dual-source computed tomography in patients with valvular heart disease. Acta Radiol. 2012; 53:270–277.
Article15. Palazzuoli A, Cademartiri F, Geleijnse ML, et al. Left ventricular remodelling and systolic function measurement with 64 multi-slice computed tomography versus second harmonic echocardiography in patients with coronary artery disease: a double blind study. Eur J Radiol. 2010; 73:82–88.
Article16. Jakobs TF, Becker CR, Ohnesorge B, et al. Multislice helical CT of the heart with retrospective ECG gating: reduction of radiation exposure by ECG-controlled tube current modulation. Eur Radiol. 2002; 12:1081–1086.
Article17. Hausleiter J, Meyer TS, Martuscelli E, et al. Image quality and radiation exposure with prospectively ECG-triggered axial scanning for coronary CT angiography: the multicenter, multivendor, randomized PROTECTION-III study. JACC Cardiovasc Imaging. 2012; 5:484–493.18. Achenbach S, Marwan M, Ropers D, et al. Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J. 2010; 31:340–346.
Article19. Austen WG, Edwards JE, Frye RL, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975; 51:5–40.
Article20. Farshad-Amacker NA, Alkadhi H, Leschka S, Frauenfelder T. Effect of high-pitch dual-source CT to compensate motion artifacts: a phantom study. Acad Radiol. 2013; 20:1234–1239.21. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.
Article22. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007; 37:1–332.23. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016; 15:155–163.
Article24. Juergens KU, Grude M, Maintz D, et al. Multi-detector row CT of left ventricular function with dedicated analysis software versus MR imaging: initial experience. Radiology. 2004; 230:403–410.
Article25. Ko SM, Kim YJ, Park JH, Choi NM. Assessment of left ventricular ejection fraction and regional wall motion with 64-slice multidetector CT: a comparison with two-dimensional transthoracic echocardiography. Br J Radiol. 2010; 83:28–34.
Article26. Cury RC, Nieman K, Shapiro MD, et al. Comprehensive assessment of myocardial perfusion defects, regional wall motion, and left ventricular function by using 64-section multidetector CT. Radiology. 2008; 248:466–475.
Article27. Marano R, Merlino B, Natale L, et al. Cross-modality accuracy of dual-step, prospectively electrocardiography-triggered dual-source computed tomorgaphy compared with same-day echocardiography and cardiac magnetic resonance imaging in the follow-up of heart-transplant patients. J Thorac Imaging. 2018; 33:217–224.
Article28. de Graaf FR, Schuijf JD, van Velzen JE, et al. Assessment of global left ventricular function and volumes with 320-row multidetector computed tomography: A comparison with 2D-echocardiography. J Nucl Cardiol. 2010; 17:225–231.
Article29. Chuang ML, Gona P, Hautvast GL, et al. Correlation of trabeculae and papillary muscles with clinical and cardiac characteristics and impact on CMR measures of LV anatomy and function. JACC Cardiovasc Imaging. 2012; 5:1115–1123.
Article30. Mao SS, Li D, Rosenthal DG, et al. Dual-standard reference values of left ventricular volumetric parameters by multidetector CT angiography. J Cardiovasc Comput Tomogr. 2013; 7:234–240.
Article31. Meyersohn NM, Szilveszter B, Staziaki PV, et al. Coronary CT angiography in the emergency department utilizing second and third generation dual source CT. J Cardiovasc Comput Tomogr. 2017; 11:249–257.
Article32. Meyer M, Haubenreisser H, Schoepf UJ, et al. Closing in on the K edge: coronary CT angiography at 100, 80, and 70 kV-initial comparison of a second- versus a third-generation dual-source CT system. Radiology. 2014; 273:373–382.
Article33. Dewey M, Vavere AL, Arbab-Zadeh A, et al. Patient characteristics as predictors of image quality and diagnostic accuracy of MDCT compared with conventional coronary angiography for detecting coronary artery stenoses: CORE-64 Multicenter International Trial. AJR Am J Roentgenol. 2010; 194:93–102.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Utility of Third-generation Dual-source Computed Tomography for Left Ventricular Function Analysis and Coronary Artery Evaluation with Minimal Radiation Exposure
- Multi-Detector Computed Tomography for Assessing the Left Ventricular Function, Perfusion and Viability
- Unusual Coronary Artery Fistula: Left Anterior Descending Coronary Artery - Left Ventricular Fistula Diagnosed by ECG-Gated Multi-Detector Row Coronary CT Angiography
- Comparison of Radiation Dose and Image Quality between the 2nd Generation and 3rd Generation Dual-Source Single-Energy and Dual-Source Dual-Energy CT of the Abdomen
- Type 4 Dual Left Anterior Descending Artery: A Case Report of a Rare Congenital Coronary Anomaly