J Korean Med Sci.
2016 Sep;31(9):1491-1498. 10.3346/jkms.2016.31.9.1491.
A Randomized Controlled Trial of Compression Rates during Cardiopulmonary Resuscitation
- Affiliations
-
- 1Department of Emergency Medicine, Wonju College of Medicine, Yonsei University, Wonju, Korea. shwang@yonsei.ac.kr
- 2Department of Emergency Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 3Department of Emergency Medicine, Yonsei University Kangnam Severance Hospital, Seoul, Korea.
- 4Department of Emergency Medicine, Seoul National University Boramae Hospital, Seoul, Korea.
- 5Department of Emergency Medicine, Yonsei University Severance Hospital, Seoul, Korea.
- 6Department of Emergency Medicine, Ajou University Hospital, Suwon, Korea.
- 7Department of Emergency Medicine, Asan Medical Center, Ulsan University, Seoul, Korea.
- 8Department of Emergency Medicine, Korea University Ansan Hospital, Ansan, Korea.
- 9Department of Emergency Medicine, Kyung Hee University Hospital, Seoul, Korea.
- 10Department of Emergency Medicine, Hanyang University Hospital, Seoul, Korea.
- 11Department of Emergency Medicine, Hallym University Saint Sacred Hospital, Anyang, Korea.
- 12Department of Emergency Medicine, Seoul National University Hospital, Seoul, Korea.
- 13Institute of Lifestyle Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 2468285
- DOI: http://doi.org/10.3346/jkms.2016.31.9.1491
Abstract
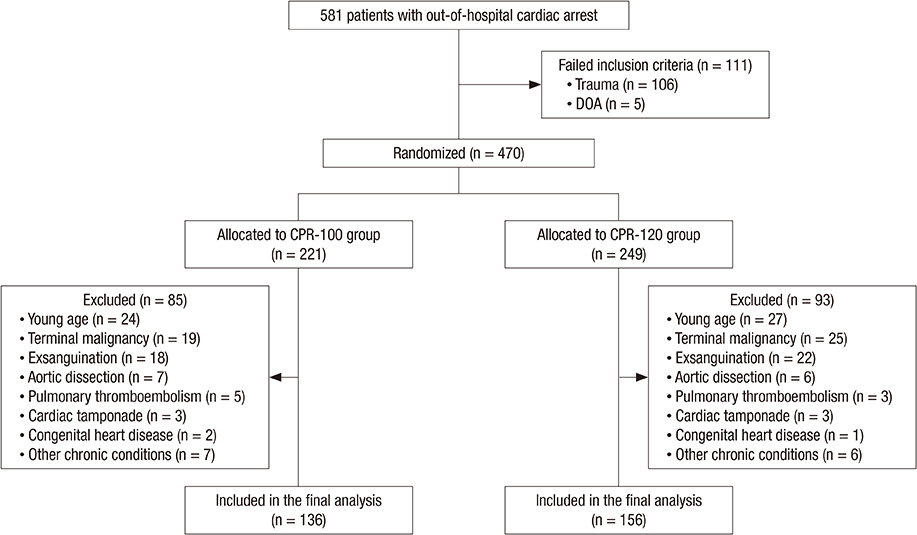
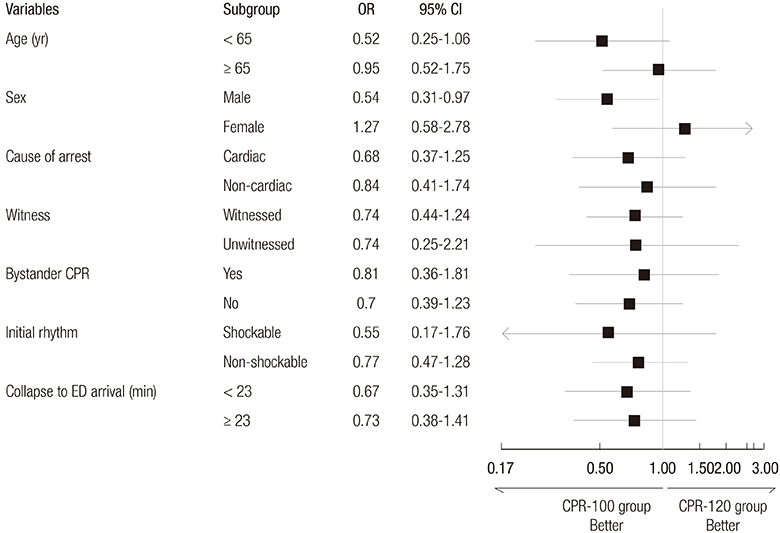
- The objective of this study was to compare the efficacy of cardiopulmonary resuscitation (CPR) with 120 compressions per minute (CPM) to CPR with 100 CPM in patients with non-traumatic out-of-hospital cardiac arrest. We randomly assigned patients with non-traumatic out-of-hospital cardiac arrest into two groups upon arrival to the emergency department (ED). The patients received manual CPR either with 100 CPM (CPR-100 group) or 120 CPM (CPR-120 group). The primary outcome measure was sustained restoration of spontaneous circulation (ROSC). The secondary outcome measures were survival discharge from the hospital, one-month survival, and one-month survival with good functional status. Of 470 patients with cardiac arrest, 136 patients in the CPR-100 group and 156 patients in the CPR-120 group were included in the final analysis. A total of 69 patients (50.7%) in the CPR-100 group and 67 patients (42.9%) in the CPR-120 group had ROSC (absolute difference, 7.8% points; 95% confidence interval [CI], -3.7 to 19.2%; P = 0.183). The rates of survival discharge from the hospital, one-month survival, and one-month survival with good functional status were not different between the two groups (16.9% vs. 12.8%, P = 0.325; 12.5% vs. 6.4%, P = 0.073; 5.9% vs. 2.6%, P = 0.154, respectively). We did not find differences in the resuscitation outcomes between those who received CPR with 100 CPM and those with 120 CPM. However, a large trial is warranted, with adequate power to confirm a statistically non-significant trend toward superiority of CPR with 100 CPM. (Clinical Trial Registration Information: www.cris.nih.go.kr, cris.nih.go.kr number, KCT0000231)
MeSH Terms
Figure
Reference
-
1. Bobrow BJ, Spaite DW, Berg RA, Stolz U, Sanders AB, Kern KB, Vadeboncoeur TF, Clark LL, Gallagher JV, Stapczynski JS, et al. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010; 304:1447–1454.2. Iwami T, Kitamura T, Kawamura T, Mitamura H, Nagao K, Takayama M, Seino Y, Tanaka H, Nonogi H, Yonemoto N, et al. Chest compression-only cardiopulmonary resuscitation for out-of-hospital cardiac arrest with public-access defibrillation: a nationwide cohort study. Circulation. 2012; 126:2844–2851.3. Svensson L, Bohm K, Castrèn M, Pettersson H, Engerström L, Herlitz J, Rosenqvist M. Compression-only CPR or standard CPR in out-of-hospital cardiac arrest. N Engl J Med. 2010; 363:434–442.4. Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O'Hearn N, Vanden Hoek TL, Becker LB. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005; 293:305–310.5. Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O'Hearn N, Wigder HN, Hoffman P, Tynus K, Vanden Hoek TL, Becker LB. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005; 111:428–434.6. Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, Callaway CW, Bishop D, Vaillancourt C, Davis D, et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009; 120:1241–1247.7. Pernat A, Weil MH, Sun S, Tang W. Stroke volumes and end-tidal carbon dioxide generated by precordial compression during ventricular fibrillation. Crit Care Med. 2003; 31:1819–1823.8. Swenson RD, Weaver WD, Niskanen RA, Martin J, Dahlberg S. Hemodynamics in humans during conventional and experimental methods of cardiopulmonary resuscitation. Circulation. 1988; 78:630–639.9. Guidelines for cardiopulmonary resuscitation and emergency cardiac care. Emergency Cardiac Care Committee and Subcommittees, American Heart Association. Part II. Adult basic life support. JAMA. 1992; 268:2184–2198.10. Cardiopulmonary resuscitation. JAMA. 1966; 198:372–379.11. Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. JAMA. 1960; 173:1064–1067.12. International Liaison Committee on Resuscitation. 2005 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Part 2: adult basic life support. Resuscitation. 2005; 67:187–201.13. Sayre MR, Koster RW, Botha M, Cave DM, Cudnik MT, Handley AJ, Hatanaka T, Hazinski MF, Jacobs I, Monsieurs K, et al. Part 5: adult basic life support: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2010; 122:S298–324.14. Koster RW, Baubin MA, Bossaert LL, Caballero A, Cassan P, Castrén M, Granja C, Handley AJ, Monsieurs KG, Perkins GD, et al. European Resuscitation Council guidelines for resuscitation 2010 section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2010; 81:1277–1292.15. Perkins GD, Travers AH, Berg RA, Castren M, Considine J, Escalante R, Gazmuri RJ, Koster RW, Lim SH, Nation KJ, et al. Part 3: adult basic life support and automated external defibrillation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2015; 95:e43–69.16. Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975; 1:480–484.17. Maier GW, Tyson GS Jr, Olsen CO, Kernstein KH, Davis JW, Conn EH, Sabiston DC Jr, Rankin JS. The physiology of external cardiac massage: high-impulse cardiopulmonary resuscitation. Circulation. 1984; 70:86–101.18. Feneley MP, Maier GW, Kern KB, Gaynor JW, Gall SA Jr, Sanders AB, Raessler K, Muhlbaier LH, Rankin JS, Ewy GA. Influence of compression rate on initial success of resuscitation and 24 hour survival after prolonged manual cardiopulmonary resuscitation in dogs. Circulation. 1988; 77:240–250.19. Halperin HR, Tsitlik JE, Guerci AD, Mellits ED, Levin HR, Shi AY, Chandra N, Weisfeldt ML. Determinants of blood flow to vital organs during cardiopulmonary resuscitation in dogs. Circulation. 1986; 73:539–550.20. Kern KB, Sanders AB, Raife J, Milander MM, Otto CW, Ewy GA. A study of chest compression rates during cardiopulmonary resuscitation in humans. The importance of rate-directed chest compressions. Arch Intern Med. 1992; 152:145–149.21. Idris AH, Guffey D, Aufderheide TP, Brown S, Morrison LJ, Nichols P, Powell J, Daya M, Bigham BL, Atkins DL, et al. Relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012; 125:3004–3012.22. Wallace SK, Abella BS, Becker LB. Quantifying the effect of cardiopulmonary resuscitation quality on cardiac arrest outcome: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2013; 6:148–156.23. Idris AH, Guffey D, Pepe PE, Brown SP, Brooks SC, Callaway CW, Christenson J, Davis DP, Daya MR, Gray R, et al. Chest compression rates and survival following out-of-hospital cardiac arrest. Crit Care Med. 2015; 43:840–848.24. Wolfe JA, Maier GW, Newton JR Jr, Glower DD, Tyson GS Jr, Spratt JA, Rankin JS, Olsen CO. Physiologic determinants of coronary blood flow during external cardiac massage. J Thorac Cardiovasc Surg. 1988; 95:523–532.25. Field RA, Soar J, Davies RP, Akhtar N, Perkins GD. The impact of chest compression rates on quality of chest compressions - a manikin study. Resuscitation. 2012; 83:360–364.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Augmented-Medication CardioPulmonary Resuscitation (AMCPR) trial: a study protocol for a randomized controlled trial
- The Author's Response: Compression Rate during Cardiopulmonary Resuscitation
- The Effect of a Real Time Audiovisual Feedback System on the Quality of Chest Compressions by Trained Personnel during Resuscitation: A Randomized Controlled Trial using a Manikin Model
- Effects of Virtual Reality Cardiopulmonary Resuscitation Practice on the Knowledge, Skills, and Attitudes of Nursing Students: A single-blind randomized controlled trial (RCT)
- Does Switching Rescuers Every 2 Minutes Improve the Quality of Chest Compression Provided in Cardiopulmonary Resuscitation?