J Korean Med Sci.
2016 Oct;31(10):1516-1528. 10.3346/jkms.2016.31.10.1516.
Clinical Practice Guidelines for the Management of Atypical Hemolytic Uremic Syndrome in Korea
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Korea.
- 2Research Coordination Center for Rare Diseases, Seoul National University Hospital, Seoul, Korea.
- 3Division of Nephrology, Department of Internal Medicine, Korea University School of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Seoul National University, Seoul, Korea.
- 5Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Division of Hematology, Department of Internal Medicine, Yonsei University College of Medicine, Severance Hospital, Seoul, Korea.
- 7Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea.
- 8Division of Nephrology, Dongtan Sacred Heart Hospital, Hallym University Medical Center, Hwaseong, Korea.
- 9Division of Hematology, Department of Internal Medicine, Korea University School of Medicine, Seoul, Korea.
- 10Department of Pediatrics, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea.
- 11Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 12Department of Pediatrics, Korea University Guro Hospital, Seoul, Korea.
- 13Department of Internal Medicine, School of Medicine, CHA University, Seongnam, Korea. doh@cha.ac.kr
- KMID: 2468240
- DOI: http://doi.org/10.3346/jkms.2016.31.10.1516
Abstract
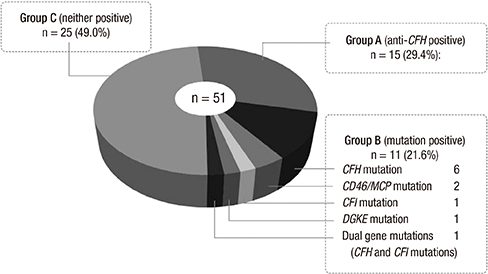
- Atypical hemolytic uremic syndrome (aHUS) is a rare syndrome characterized by micro-angiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury. The major pathogenesis of aHUS involves dysregulation of the complement system. Eculizumab, which blocks complement C5 activation, has recently been proven as an effective agent. Delayed diagnosis and treatment of aHUS can cause death or end-stage renal disease. Therefore, a diagnosis that differentiates aHUS from other forms of thrombotic microangiopathy is very important for appropriate management. These guidelines aim to offer recommendations for the diagnosis and treatment of patients with aHUS in Korea. The guidelines have largely been adopted from the current guidelines due to the lack of evidence concerning the Korean population.
MeSH Terms
-
ADAMTS13 Protein/genetics/metabolism
Acute Kidney Injury/etiology
Antibodies, Monoclonal, Humanized/*therapeutic use
Atypical Hemolytic Uremic Syndrome/*diagnosis/epidemiology/therapy
*Blood Transfusion
Complement Factor H/genetics
Complement System Proteins/genetics/metabolism
Delayed Diagnosis
Humans
Kidney Failure, Chronic/etiology
*Organ Transplantation
Republic of Korea/epidemiology
Antibodies, Monoclonal, Humanized
Complement Factor H
Complement System Proteins
ADAMTS13 Protein
Figure
Cited by 1 articles
-
Kidney Transplantation in Patients with Atypical Hemolytic Uremic Syndrome due to Complement Factor H Deficiency: Impact of Liver Transplantation
Sejin Kim, Eujin Park, Sang-il Min, Nam-Joon Yi, Jongwon Ha, Il-Soo Ha, Hae Il Cheong, Hee Gyung Kang
J Korean Med Sci. 2018;33(1):. doi: 10.3346/jkms.2018.33.e4.
Reference
-
1. Gasser C, Gautier E, Steck A, Siebenmann RE, Oechslin R. Hemolytic-uremic syndrome: bilateral necrosis of the renal cortex in acute acquired hemolytic anemia. Schweiz Med Wochenschr. 1955; 85:905–909.2. Gordjani N, Sutor AH, Zimmerhackl LB, Brandis M. Hemolytic uremic syndromes in childhood. Semin Thromb Hemost. 1997; 23:281–293.3. Noris M, Remuzzi G. Atypical hemolytic-uremic syndrome. N Engl J Med. 2009; 361:1676–1687.4. Kavanagh D, Goodship TH, Richards A. Atypical hemolytic uremic syndrome. Semin Nephrol. 2013; 33:508–530.5. Warwicker P, Goodship TH, Donne RL, Pirson Y, Nicholls A, Ward RM, Turnpenny P, Goodship JA. Genetic studies into inherited and sporadic hemolytic uremic syndrome. Kidney Int. 1998; 53:836–844.6. Goicoechea de Jorge E, Harris CL, Esparza-Gordillo J, Carreras L, Arranz EA, Garrido CA, López-Trascasa M, Sánchez-Corral P, Morgan BP, Rodríguez de Córdoba S. Gain-of-function mutations in complement factor B are associated with atypical hemolytic uremic syndrome. Proc Natl Acad Sci USA. 2007; 104:240–245.7. Noris M, Brioschi S, Caprioli J, Todeschini M, Bresin E, Porrati F, Gamba S, Remuzzi G; International Registry of Recurrent and Familial HUS/TTP. Familial haemolytic uraemic syndrome and an MCP mutation. Lancet. 2003; 362:1542–1547.8. Dragon-Durey MA, Loirat C, Cloarec S, Macher MA, Blouin J, Nivet H, Weiss L, Fridman WH, Frémeaux-Bacchi V. Anti-Factor H autoantibodies associated with atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2005; 16:555–563.9. Lemaire M, Frémeaux-Bacchi V, Schaefer F, Choi M, Tang WH, Le Quintrec M, Fakhouri F, Taque S, Nobili F, Martinez F, et al. Recessive mutations in DGKE cause atypical hemolytic-uremic syndrome. Nat Genet. 2013; 45:531–536.10. Legendre CM, Licht C, Muus P, Greenbaum LA, Babu S, Bedrosian C, Bingham C, Cohen DJ, Delmas Y, Douglas K, et al. Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N Engl J Med. 2013; 368:2169–2181.11. Zuber J, Le Quintrec M, Krid S, Bertoye C, Gueutin V, Lahoche A, Heyne N, Ardissino G, Chatelet V, Noël LH, et al. Eculizumab for atypical hemolytic uremic syndrome recurrence in renal transplantation. Am J Transplant. 2012; 12:3337–3354.12. Loirat C, Fakhouri F, Ariceta G, Besbas N, Bitzan M, Bjerre A, Coppo R, Emma F, Johnson S, Karpman D, et al. An international consensus approach to the management of atypical hemolytic uremic syndrome in children. Pediatr Nephrol. 2016; 31:15–39.13. Menne J, Nitschke M, Stingele R, Abu-Tair M, Beneke J, Bramstedt J, Bremer JP, Brunkhorst R, Busch V, Dengler R, et al. Validation of treatment strategies for enterohaemorrhagic Escherichia coli O104:H4 induced haemolytic uraemic syndrome: case-control study. BMJ. 2012; 345:e4565.14. Rock GA, Shumak KH, Buskard NA, Blanchette VS, Kelton JG, Nair RC, Spasoff RA; Canadian Apheresis Study Group. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. N Engl J Med. 1991; 325:393–397.15. Caprioli J, Noris M, Brioschi S, Pianetti G, Castelletti F, Bettinaglio P, Mele C, Bresin E, Cassis L, Gamba S, et al. Genetics of HUS: the impact of MCP, CFH, and IF mutations on clinical presentation, response to treatment, and outcome. Blood. 2006; 108:1267–1279.16. Ariceta G, Besbas N, Johnson S, Karpman D, Landau D, Licht C, Loirat C, Pecoraro C, Taylor CM, Van de Kar N, et al. Guideline for the investigation and initial therapy of diarrhea-negative hemolytic uremic syndrome. Pediatr Nephrol. 2009; 24:687–696.17. Taylor CM, Machin S, Wigmore SJ, Goodship TH. working party from the Renal Association, the British Committee for Standards in Haematology and the British Transplantation Society. Clinical practice guidelines for the management of atypical haemolytic uraemic syndrome in the United Kingdom. Br J Haematol. 2010; 148:37–47.18. Johnson S, Stojanovic J, Ariceta G, Bitzan M, Besbas N, Frieling M, Karpman D, Landau D, Langman C, Licht C, et al. An audit analysis of a guideline for the investigation and initial therapy of diarrhea negative (atypical) hemolytic uremic syndrome. Pediatr Nephrol. 2014; 29:1967–1978.19. Lee JM, Park YS, Lee JH, Park SJ, Shin JI, Park YH, Yoo KH, Cho MH, Kim SY, Kim SH, et al. Atypical hemolytic uremic syndrome: Korean pediatric series. Pediatr Int. 2015; 57:431–438.20. Cho HY, Lee BS, Moon KC, Ha IS, Cheong HI, Choi Y. Complete factor H deficiency-associated atypical hemolytic uremic syndrome in a neonate. Pediatr Nephrol. 2007; 22:874–880.21. Kim JO, Lee SJ, Kim ES, Ko KH, Kim NK, Oh D. Analysis of genetic factors in 9 Korean adult patients with atypical hemolytic uremic syndrome. In : Proceedings of Korean Society on Thrombosis and Hemostasis; 2015. p. 187.22. Niaudet P. Complement-mediated hemolytic uremic syndrome [Internet]. accessed on 15 November 2015. Available at http://www.uptodate.com/contents/complement-mediated-hemolytic-uremic-syndrome?source=search_result&search=Complement-mediated+hemolytic+uremic+syndrome&selectedTitle=1%7E36.23. Nester CM, Barbour T, de Cordoba SR, Dragon-Durey MA, Fremeaux-Bacchi V, Goodship TH, Kavanagh D, Noris M, Pickering M, Sanchez-Corral P, et al. Atypical aHUS: State of the art. Mol Immunol. 2015; 67:31–42.24. George JN, Nester CM. Syndromes of thrombotic microangiopathy. N Engl J Med. 2014; 371:1847–1848.25. Sawai T, Nangaku M, Ashida A, Fujimaru R, Hataya H, Hidaka Y, Kaname S, Okada H, Sato W, Yasuda T, et al. Diagnostic criteria for atypical hemolytic uremic syndrome proposed by the Joint Committee of the Japanese Society of Nephrology and the Japan Pediatric Society. Pediatr Int. 2014; 56:1–5.26. Ohanian M, Cable C, Halka K. Eculizumab safely reverses neurologic impairment and eliminates need for dialysis in severe atypical hemolytic uremic syndrome. Clin Pharmacol. 2011; 3:5–12.27. Zimmerhackl LB, Besbas N, Jungraithmayr T, van de Kar N, Karch H, Karpman D, Landau D, Loirat C, Proesmans W, Prüfer F, et al. Epidemiology, clinical presentation, and pathophysiology of atypical and recurrent hemolytic uremic syndrome. Semin Thromb Hemost. 2006; 32:113–120.28. Fujimura Y, Matsumoto M. Registry of 919 patients with thrombotic microangiopathies across Japan: database of Nara Medical University during 1998-2008. Intern Med. 2010; 49:7–15.29. Licht C, Ardissino G, Ariceta G, Cohen DJ, Gasteyger C, Greenbaum LA, Johnson SA, Ogawa M, Schaefer FS, Walle JV, et al. Characteristics of 681 patients with atypical hemolytic uremic syndrome in the global aHUS registry. In : Proceedings of 2015 American Society of Nephrology (ASN) Annual Meeting; 2015 Nov 3-8; San Diego, CA.30. Sellier-Leclerc AL, Fremeaux-Bacchi V, Dragon-Durey MA, Macher MA, Niaudet P, Guest G, Boudailliez B, Bouissou F, Deschenes G, Gie S, et al. Differential impact of complement mutations on clinical characteristics in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2007; 18:2392–2400.31. Noris M, Caprioli J, Bresin E, Mossali C, Pianetti G, Gamba S, Daina E, Fenili C, Castelletti F, Sorosina A, et al. Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype. Clin J Am Soc Nephrol. 2010; 5:1844–1859.32. Sullivan M, Erlic Z, Hoffmann MM, Arbeiter K, Patzer L, Budde K, Hoppe B, Zeier M, Lhotta K, Rybicki LA, et al. Epidemiological approach to identifying genetic predispositions for atypical hemolytic uremic syndrome. Ann Hum Genet. 2010; 74:17–26.33. Westra D, Volokhina E, van der Heijden E, Vos A, Huigen M, Jansen J, van Kaauwen E, van der Velden T, van de Kar N, van den Heuvel L. Genetic disorders in complement (regulating) genes in patients with atypical haemolytic uraemic syndrome (aHUS). Nephrol Dial Transplant. 2010; 25:2195–2202.34. Esparza-Gordillo J, Goicoechea de Jorge E, Buil A, Carreras Berges L, López-Trascasa M, Sánchez-Corral P, Rodríguez de Córdoba S. Predisposition to atypical hemolytic uremic syndrome involves the concurrence of different susceptibility alleles in the regulators of complement activation gene cluster in 1q32. Hum Mol Genet. 2005; 14:703–712.35. Dragon-Durey MA, Blanc C, Marliot F, Loirat C, Blouin J, Sautes-Fridman C, Fridman WH, Frémeaux-Bacchi V. The high frequency of complement factor H related CFHR1 gene deletion is restricted to specific subgroups of patients with atypical haemolytic uraemic syndrome. J Med Genet. 2009; 46:447–450.36. Bienaimé F, Dragon-Durey MA, Regnier CH, Nilsson SC, Kwan WH, Blouin J, Jablonski M, Renault N, Rameix-Welti MA, Loirat C, et al. Mutations in components of complement influence the outcome of Factor I-associated atypical hemolytic uremic syndrome. Kidney Int. 2010; 77:339–349.37. Noris M, Mescia F, Remuzzi G. STEC-HUS, atypical HUS and TTP are all diseases of complement activation. Nat Rev Nephrol. 2012; 8:622–633.38. Rayes J, Roumenina LT, Dimitrov JD, Repessé Y, Ing M, Christophe O, Jokiranta TS, Halbwachs-Mecarelli L, Borel-Derlon A, Kaveri SV, et al. The interaction between factor H and VWF increases factor H cofactor activity and regulates VWF prothrombotic status. Blood. 2014; 123:121–125.39. Sadler JE. What's new in the diagnosis and pathophysiology of thrombotic thrombocytopenic purpura. Hematology Am Soc Hematol Educ Program. 2015; 2015:631–636.40. Tsai HM. Untying the knot of thrombotic thrombocytopenic purpura and atypical hemolytic uremic syndrome. Am J Med. 2013; 126:200–209.41. Mele C, Lemaire M, Iatropoulos P, Piras R, Bresin E, Bettoni S, Bick D, Helbling D, Veith R, Valoti E, et al. Characterization of a new DGKE intronic mutation in genetically unsolved cases of familial atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2015; 10:1011–1019.42. Bu F, Maga T, Meyer NC, Wang K, Thomas CP, Nester CM, Smith RJ. Comprehensive genetic analysis of complement and coagulation genes in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2014; 25:55–64.43. Hyvärinen S, Jokiranta TS. Minor role of plasminogen in complement activation on cell surfaces. PLoS One. 2015; 10:e0143707.44. Sharma AP, Greenberg CR, Prasad AN, Prasad C. Hemolytic uremic syndrome (HUS) secondary to cobalamin C (cblC) disorder. Pediatr Nephrol. 2007; 22:2097–2103.45. Labrune P, Zittoun J, Duvaltier I, Trioche P, Marquet J, Niaudet P, Odièvre M. Haemolytic uraemic syndrome and pulmonary hypertension in a patient with methionine synthase deficiency. Eur J Pediatr. 1999; 158:734–739.46. Gottschall JL, Neahring B, McFarland JG, Wu GG, Weitekamp LA, Aster RH. Quinine-induced immune thrombocytopenia with hemolytic uremic syndrome: clinical and serological findings in nine patients and review of literature. Am J Hematol. 1994; 47:283–289.47. Maga TK, Nishimura CJ, Weaver AE, Frees KL, Smith RJ. Mutations in alternative pathway complement proteins in American patients with atypical hemolytic uremic syndrome. Hum Mutat. 2010; 31:E1445–60.48. Lee BH, Kwak SH, Shin JI, Lee SH, Choi HJ, Kang HG, Ha IS, Lee JS, Dragon-Durey MA, Choi Y, et al. Atypical hemolytic uremic syndrome associated with complement factor H autoantibodies and CFHR1/CFHR3 deficiency. Pediatr Res. 2009; 66:336–340.49. Webb RF, Ramirez AM, Hocken AG, Pettit JE. Acute intravascular haemolysis due to quinine. N Z Med J. 1980; 91:14–16.50. Fakhouri F, Roumenina L, Provot F, Sallée M, Caillard S, Couzi L, Essig M, Ribes D, Dragon-Durey MA, Bridoux F, et al. Pregnancy-associated hemolytic uremic syndrome revisited in the era of complement gene mutations. J Am Soc Nephrol. 2010; 21:859–867.51. Lechner K, Obermeier HL. Cancer-related microangiopathic hemolytic anemia: clinical and laboratory features in 168 reported cases. Medicine (Baltimore). 2012; 91:195–205.52. Ho VT, Cutler C, Carter S, Martin P, Adams R, Horowitz M, Ferrara J, Soiffer R, Giralt S. Blood and marrow transplant clinical trials network toxicity committee consensus summary: thrombotic microangiopathy after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2005; 11:571–575.53. Kavanagh D, Goodship T. Genetics and complement in atypical HUS. Pediatr Nephrol. 2010; 25:2431–2442.54. Hofer J, Giner T, Józsi M. Complement factor H-antibody-associated hemolytic uremic syndrome: pathogenesis, clinical presentation, and treatment. Semin Thromb Hemost. 2014; 40:431–443.55. Laurence J. Atypical hemolytic uremic syndrome (aHUS): making the diagnosis. Clin Adv Hematol Oncol. 2012; 10:1–12.56. Fremeaux-Bacchi V, Fakhouri F, Garnier A, Bienaimé F, Dragon-Durey MA, Ngo S, Moulin B, Servais A, Provot F, Rostaing L, et al. Genetics and outcome of atypical hemolytic uremic syndrome: a nationwide French series comparing children and adults. Clin J Am Soc Nephrol. 2013; 8:554–562.57. Keir LS, Saleem MA. Current evidence for the role of complement in the pathogenesis of Shiga toxin haemolytic uraemic syndrome. Pediatr Nephrol. 2014; 29:1895–1902.58. Poolpol K, Orth-Höller D, Speth C, Zipfel PF, Skerka C, de Córdoba SR, Brockmeyer J, Bielaszewska M, Würzner R. Interaction of Shiga toxin 2 with complement regulators of the factor H protein family. Mol Immunol. 2014; 58:77–84.59. Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A; Acute Kidney Injury Network. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007; 11:R31.60. Thomas ME, Blaine C, Dawnay A, Devonald MA, Ftouh S, Laing C, Latchem S, Lewington A, Milford DV, Ostermann M. The definition of acute kidney injury and its use in practice. Kidney Int. 2015; 87:62–73.61. Reischl U, Youssef MT, Kilwinski J, Lehn N, Zhang WL, Karch H, Strockbine NA. Real-time fluorescence PCR assays for detection and characterization of Shiga toxin, intimin, and enterohemolysin genes from Shiga toxin-producing Escherichia coli. J Clin Microbiol. 2002; 40:2555–2565.62. El Sayed Zaki M, El-Adrosy H. Diagnosis of Shiga toxin producing Escherichia coli infection, contribution of genetic amplification technique. Microbes Infect. 2007; 9:200–203.63. Pulz M, Matussek A, Monazahian M, Tittel A, Nikolic E, Hartmann M, Bellin T, Buer J, Gunzer F. Comparison of a shiga toxin enzyme-linked immunosorbent assay and two types of PCR for detection of shiga toxin-producing Escherichia coli in human stool specimens. J Clin Microbiol. 2003; 41:4671–4675.64. Teel LD, Daly JA, Jerris RC, Maul D, Svanas G, O'Brien AD, Park CH. Rapid detection of Shiga toxin-producing Escherichia coli by optical immunoassay. J Clin Microbiol. 2007; 45:3377–3380.65. Park CH, Kim HJ, Hixon DL, Bubert A. Evaluation of the duopath verotoxin test for detection of shiga toxins in cultures of human stools. J Clin Microbiol. 2003; 41:2650–2653.66. Kehl KS, Havens P, Behnke CE, Acheson DW. Evaluation of the premier EHEC assay for detection of Shiga toxin-producing Escherichia coli. J Clin Microbiol. 1997; 35:2051–2054.67. Gavin PJ, Peterson LR, Pasquariello AC, Blackburn J, Hamming MG, Kuo KJ, Thomson RB Jr. Evaluation of performance and potential clinical impact of ProSpecT Shiga toxin Escherichia coli microplate assay for detection of Shiga Toxin-producing E. coli in stool samples. J Clin Microbiol. 2004; 42:1652–1656.68. Vallières E, Saint-Jean M, Rallu F. Comparison of three different methods for detection of Shiga toxin-producing Escherichia coli in a tertiary pediatric care center. J Clin Microbiol. 2013; 51:481–486.69. Furlan M, Robles R, Galbusera M, Remuzzi G, Kyrle PA, Brenner B, Krause M, Scharrer I, Aumann V, Mittler U, et al. von Willebrand factor-cleaving protease in thrombotic thrombocytopenic purpura and the hemolytic-uremic syndrome. N Engl J Med. 1998; 339:1578–1584.70. Tsai HM, Lian EC. Antibodies to von Willebrand factor-cleaving protease in acute thrombotic thrombocytopenic purpura. N Engl J Med. 1998; 339:1585–1594.71. Veyradier A, Obert B, Houllier A, Meyer D, Girma JP. Specific von Willebrand factor-cleaving protease in thrombotic microangiopathies: a study of 111 cases. Blood. 2001; 98:1765–1772.72. Cataland SR, Wu HM. How I treat: the clinical differentiation and initial treatment of adult patients with atypical hemolytic uremic syndrome. Blood. 2014; 123:2478–2484.73. Sarode R, Bandarenko N, Brecher ME, Kiss JE, Marques MB, Szczepiorkowski ZM, Winters JL. Thrombotic thrombocytopenic purpura: 2012 American Society for Apheresis (ASFA) consensus conference on classification, diagnosis, management, and future research. J Clin Apher. 2014; 29:148–167.74. Tsai HM. Thrombotic thrombocytopenic purpura and the atypical hemolytic uremic syndrome: an update. Hematol Oncol Clin North Am. 2013; 27:565–584.75. Remuzzi G, Galbusera M, Noris M, Canciani MT, Daina E, Bresin E, Contaretti S, Caprioli J, Gamba S, Ruggenenti P, et al. Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome. von Willebrand factor cleaving protease (ADAMTS13) is deficient in recurrent and familial thrombotic thrombocytopenic purpura and hemolytic uremic syndrome. Blood. 2002; 100:778–785.76. Cataland SR, Wu HM. Atypical hemolytic uremic syndrome and thrombotic thrombocytopenic purpura: clinically differentiating the thrombotic microangiopathies. Eur J Intern Med. 2013; 24:486–491.77. Bell WR, Braine HG, Ness PM, Kickler TS. Improved survival in thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Clinical experience in 108 patients. N Engl J Med. 1991; 325:398–403.78. Mitra D, Jaffe EA, Weksler B, Hajjar KA, Soderland C, Laurence J. Thrombotic thrombocytopenic purpura and sporadic hemolytic-uremic syndrome plasmas induce apoptosis in restricted lineages of human microvascular endothelial cells. Blood. 1997; 89:1224–1234.79. Tsai HM. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol. 2010; 91:1–19.80. Hosler GA, Cusumano AM, Hutchins GM. Thrombotic thrombocytopenic purpura and hemolytic uremic syndrome are distinct pathologic entities. A review of 56 autopsy cases. Arch Pathol Lab Med. 2003; 127:834–839.81. Magro CM, Momtahen S, Mulvey JJ, Yassin AH, Kaplan RB, Laurence JC. Role of the skin biopsy in the diagnosis of atypical hemolytic uremic syndrome. Am J Dermatopathol. 2015; 37:349–356.82. Coppo P, Bengoufa D, Veyradier A, Wolf M, Bussel A, Millot GA, Malot S, Heshmati F, Mira JP, Boulanger E, et al. Severe ADAMTS13 deficiency in adult idiopathic thrombotic microangiopathies defines a subset of patients characterized by various autoimmune manifestations, lower platelet count, and mild renal involvement. Medicine (Baltimore). 2004; 83:233–244.83. Jang MJ, Chong SY, Kim IH, Kim JH, Jung CW, Kim JY, Park JC, Lee SM, Kim YK, Lee JE, et al. Clinical features of severe acquired ADAMTS13 deficiency in thrombotic thrombocytopenic purpura: the Korean TTP registry experience. Int J Hematol. 2011; 93:163–169.84. Kremer Hovinga JA, Vesely SK, Terrell DR, Lämmle B, George JN. Survival and relapse in patients with thrombotic thrombocytopenic purpura. Blood. 2010; 115:1500–1511.85. Matsumoto M, Bennett CL, Isonishi A, Qureshi Z, Hori Y, Hayakawa M, Yoshida Y, Yagi H, Fujimura Y. Acquired idiopathic ADAMTS13 activity deficient thrombotic thrombocytopenic purpura in a population from Japan. PLoS One. 2012; 7:e33029.86. Zheng XL, Kaufman RM, Goodnough LT, Sadler JE. Effect of plasma exchange on plasma ADAMTS13 metalloprotease activity, inhibitor level, and clinical outcome in patients with idiopathic and nonidiopathic thrombotic thrombocytopenic purpura. Blood. 2004; 103:4043–4049.87. Gulleroglu K, Fidan K, Hançer VS, Bayrakci U, Baskin E, Soylemezoglu O. Neurologic involvement in atypical hemolytic uremic syndrome and successful treatment with eculizumab. Pediatr Nephrol. 2013; 28:827–830.88. Ohanian M, Cable C, Halka K. Reduced dose maintenance eculizumab in atypical hemolytic uremic syndrome (aHUS): an update on a previous case report. Clin Pharmacol. 2011; 3:45–50.89. Salem G, Flynn JM, Cataland SR. Profound neurological injury in a patient with atypical hemolytic uremic syndrome. Ann Hematol. 2013; 92:557–558.90. George JN. How I treat patients with thrombotic thrombocytopenic purpura: 2010. Blood. 2010; 116:4060–4069.91. Coppo P, Schwarzinger M, Buffet M, Wynckel A, Clabault K, Presne C, Poullin P, Malot S, Vanhille P, Azoulay E, et al. Predictive features of severe acquired ADAMTS13 deficiency in idiopathic thrombotic microangiopathies: the French TMA reference center experience. PLoS One. 2010; 5:e10208.92. Loirat C, Frémeaux-Bacchi V. Atypical hemolytic uremic syndrome. Orphanet J Rare Dis. 2011; 6:60.93. Ståhl AL, Vaziri-Sani F, Heinen S, Kristoffersson AC, Gydell KH, Raafat R, Gutierrez A, Beringer O, Zipfel PF, Karpman D. Factor H dysfunction in patients with atypical hemolytic uremic syndrome contributes to complement deposition on platelets and their activation. Blood. 2008; 111:5307–5315.94. Dragon-Durey MA, Blanc C, Roumenina LT, Poulain N, Ngo S, Bordereau P, Frémeaux-Bacchi V. Anti-factor H autoantibodies assay. Methods Mol Biol. 2014; 1100:249–256.95. Saland JM, Ruggenenti P, Remuzzi G; Consensus Study Group. Liver-kidney transplantation to cure atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2009; 20:940–949.96. Nürnberger J, Philipp T, Witzke O, Opazo Saez A, Vester U, Baba HA, Kribben A, Zimmerhackl LB, Janecke AR, Nagel M, et al. Eculizumab for atypical hemolytic-uremic syndrome. N Engl J Med. 2009; 360:542–544.97. Cofiell R, Kukreja A, Bedard K, Yan Y, Mickle AP, Ogawa M, Bedrosian CL, Faas SJ. Eculizumab reduces complement activation, inflammation, endothelial damage, thrombosis, and renal injury markers in aHUS. Blood. 2015; 125:3253–3262.98. Fakhouri F, Delmas Y, Provot F, Barbet C, Karras A, Makdassi R, Courivaud C, Rifard K, Servais A, Allard C, et al. Insights from the use in clinical practice of eculizumab in adult patients with atypical hemolytic uremic syndrome affecting the native kidneys: an analysis of 19 cases. Am J Kidney Dis. 2014; 63:40–48.99. Ardissino G, Testa S, Possenti I, Tel F, Paglialonga F, Salardi S, Tedeschi S, Belingheri M, Cugno M. Discontinuation of eculizumab maintenance treatment for atypical hemolytic uremic syndrome: a report of 10 cases. Am J Kidney Dis. 2014; 64:633–637.100. Cugno M, Gualtierotti R, Possenti I, Testa S, Tel F, Griffini S, Grovetti E, Tedeschi S, Salardi S, Cresseri D, et al. Complement functional tests for monitoring eculizumab treatment in patients with atypical hemolytic uremic syndrome. J Thromb Haemost. 2014; 12:1440–1448.101. Ardissino G, Possenti I, Tel F, Testa S, Salardi S, Ladisa V. Discontinuation of eculizumab treatment in atypical hemolytic uremic syndrome: an update. Am J Kidney Dis. 2015; 66:172–173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A clinical aspect of the hemolytic uremic syndrome
- Case Report of Pregnancy Induced Atypical Hemolytic-uremic Syndrome
- Atypical Hemolytic Uremic Syndrome Associated with Streptococcus pneumoniae Infection
- Delayed Hemolytic Uremic Syndrome Presenting as Diffuse Alveolar Hemorrhage
- A Case of the Diarrhea-associated Hemolytic Uremic Syndrome Developing Simultaneously with an Acute Appendicitis