Korean J Transplant.
2019 Dec;33(4):106-111. 10.4285/jkstn.2019.33.4.106.
Long-term results of conjoined unification venoplasty for multiple portal vein branches of the right liver graft in living donor liver transplantations
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- 2Department of Surgery, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2468160
- DOI: http://doi.org/10.4285/jkstn.2019.33.4.106
Abstract
- BACKGROUND
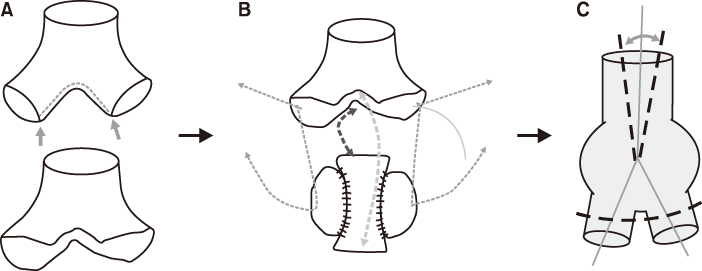
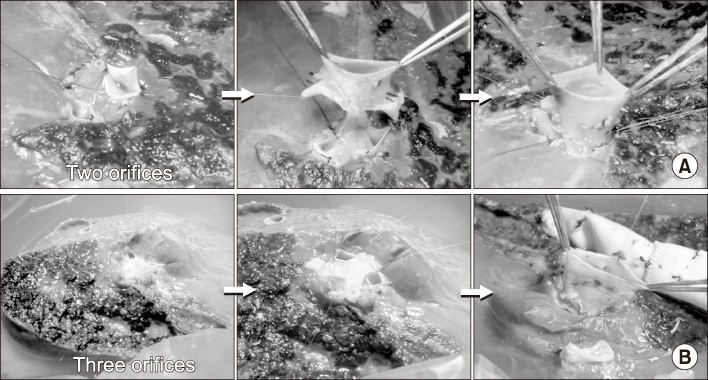
Autologous portal vein Y-graft (PYG) interposition has been the standard procedure for reconstruction of double portal vein (PV) orifices of right liver grafts during living donor liver transplantations. However, it has the disadvantage of being vulnerable to anastomotic stenosis. A refined technique of conjoined unification venoplasty (CUV) was developed to secure PV reconstruction.
METHODS
We reviewed the surgical outcomes in PV reconstructions using CUVs in 21 cases which were followed up for >3 years.
RESULTS
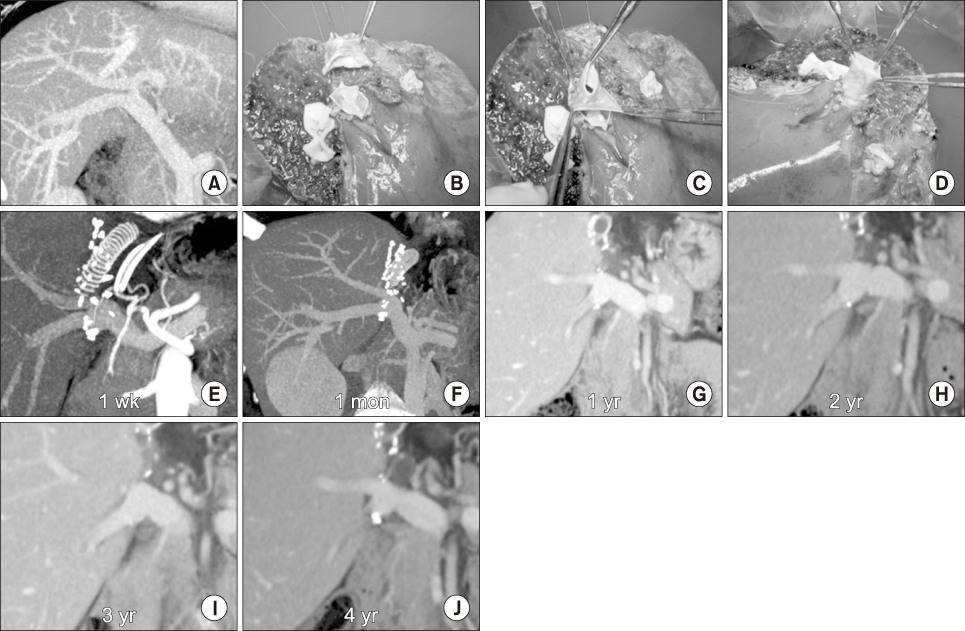
The mean age of recipients was 51.7±4.9 years. The model for end-stage liver disease score was 15.3±6.4. The graft-recipient weight ratio was 1.12±0.21. Recipient PYGs were harvested in all cases. All living donors were blood relatives or relatives through marriage with type III PV anomalies. The number of right liver graft PV orifices was two in 19 cases and three in two cases. For the central intervening vein patch, a PV segment was used in six cases, and an autologous greater saphenous vein patch was used in the remaining 15 cases. The 21 patient cohort displayed a 100% 4-year patient survival rate. None of them underwent any PV interventions including interventional stenting. Serial follow-up computed tomography scans revealed that the reconstructed PV showed early reshaping with a stable streamlined configuration for over 3 years.
CONCLUSIONS
PV reconstruction using the CUV technique appears to be significantly more effective in preventing PV complications. We believe that CUV is a useful technique to reconstruct right liver grafts with multiple PV orifices.
MeSH Terms
Figure
Reference
-
1. Hwang S, Lee SG, Lee YJ, Sung KB, Park KM, Kim KH, et al. Lessons learned from 1,000 living donor liver transplantations in a single center: how to make living donations safe. Liver Transpl. 2006; 12:920–927.
Article2. Marcos A, Orloff M, Mieles L, Olzinski A, Sitzmann J. Reconstruction of double hepatic arterial and portal venous branches for right-lobe living donor liver transplantation. Liver Transpl. 2001; 7:673–679.
Article3. Thayer WP, Claridge JA, Pelletier SJ, Oh CK, Sanfey HA, Sawyer RG, et al. Portal vein reconstruction in right lobe living-donor liver transplantation. J Am Coll Surg. 2002; 194:96–98.
Article4. Lee SG, Hwang S, Kim KH, Ahn CS, Park KM, Lee YJ, et al. Approach to anatomic variations of the graft portal vein in right lobe living-donor liver transplantation. Transplantation. 2003; 75(3 Suppl):S28–S32.
Article5. Hwang S, Lee SG, Ahn CS, Kim KH, Moon DB, Ha TY, et al. Technique and outcome of autologous portal Y-graft interposition for anomalous right portal veins in living donor liver transplantation. Liver Transpl. 2009; 15:427–434.
Article6. Lee HJ, Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, et al. Long-term outcomes of portal Y-graft interposition for anomalous right portal veins in living donor liver transplantation. Transplant Proc. 2012; 44:454–456.
Article7. Ha TY, Hwang S, Moon DB, Ahn CS, Kim KH, Song GW, et al. Conjoined unification venoplasty for graft double portal vein branches as a modification of autologous Y-graft interposition. Liver Transpl. 2015; 21:707–710.
Article8. Hwang S, Ha TY, Song GW, Jung DH, Moon DB, Ahn CS, et al. Conjoined unification venoplasty for double portal vein branches of right liver graft: 1-year experience at a high-volume living donor liver transplantation center. J Gastrointest Surg. 2016; 20:199–205.
Article9. Kwon JH, Hwang S, Song GW, Moon DB, Park GC, Kim SH, et al. Conjoined unification venoplasty for triple portal vein branches of right liver graft: a case report and technical refinement. Korean J Hepatobiliary Pancreat Surg. 2016; 20:61–65.
Article10. Moon DB, Lee SG, Ahn C, Hwang S, Kim KH, Ha T, et al. Application of intraoperative cine-portogram to detect spontaneous portosystemic collaterals missed by intraoperative doppler exam in adult living donor liver transplantation. Liver Transpl. 2007; 13:1279–1284.
Article11. Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, Song GW, et al. Standardization of modified right lobe grafts to minimize vascular outflow complications for adult living donor liver transplantation. Transplant Proc. 2012; 44:457–459.
Article12. Hwang S, Ha TY, Ahn CS, Moon DB, Kim KH, Song GW, et al. Standardized surgical techniques for adult living donor liver transplantation using a modified right lobe graft: a video presentation from bench to reperfusion. Korean J Hepatobiliary Pancreat Surg. 2016; 20:97–101.
Article13. Hwang S, Lee SG, Ahn CS, Moon DB, Kim KH, Ha TY, et al. Outflow vein reconstruction of extended right lobe graft using quilt venoplasty technique. Liver Transpl. 2006; 12:156–158.
Article14. Hwang S, Ha TY, Ahn CS, Moon DB, Song GW, Kim KH, et al. Hemodynamics-compliant reconstruction of the right hepatic vein for adult living donor liver transplantation with a right liver graft. Liver Transpl. 2012; 18:858–866.
Article15. Sugawara Y, Makuuchi M, Tamura S, Matsui Y, Kaneko J, Hasegawa K, et al. Portal vein reconstruction in adult living donor liver transplantation using cryopreserved vein grafts. Liver Transpl. 2006; 12:1233–1236.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Conjoined unification venoplasty for triple portal vein branches of right liver graft: a case report and technical refinement
- Standardized surgical techniques for adult living donor liver transplantation using a modified right lobe graft: a video presentation from bench to reperfusion
- Graft outflow vein unification venoplasty with superficial left hepatic vein branch in pediatric living donor liver transplantation using a left lateral section graft
- Clinical applicability of autologous great saphenous vein for living donor liver transplantation
- Side-to-side portal vein reconstruction for infant-to-infant deceased donor whole liver transplantation: Report of 2 cases with video