Side-to-side portal vein reconstruction for infant-to-infant deceased donor whole liver transplantation: Report of 2 cases with video
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2505342
- DOI: http://doi.org/10.14701/ahbps.2020.24.3.301
Abstract
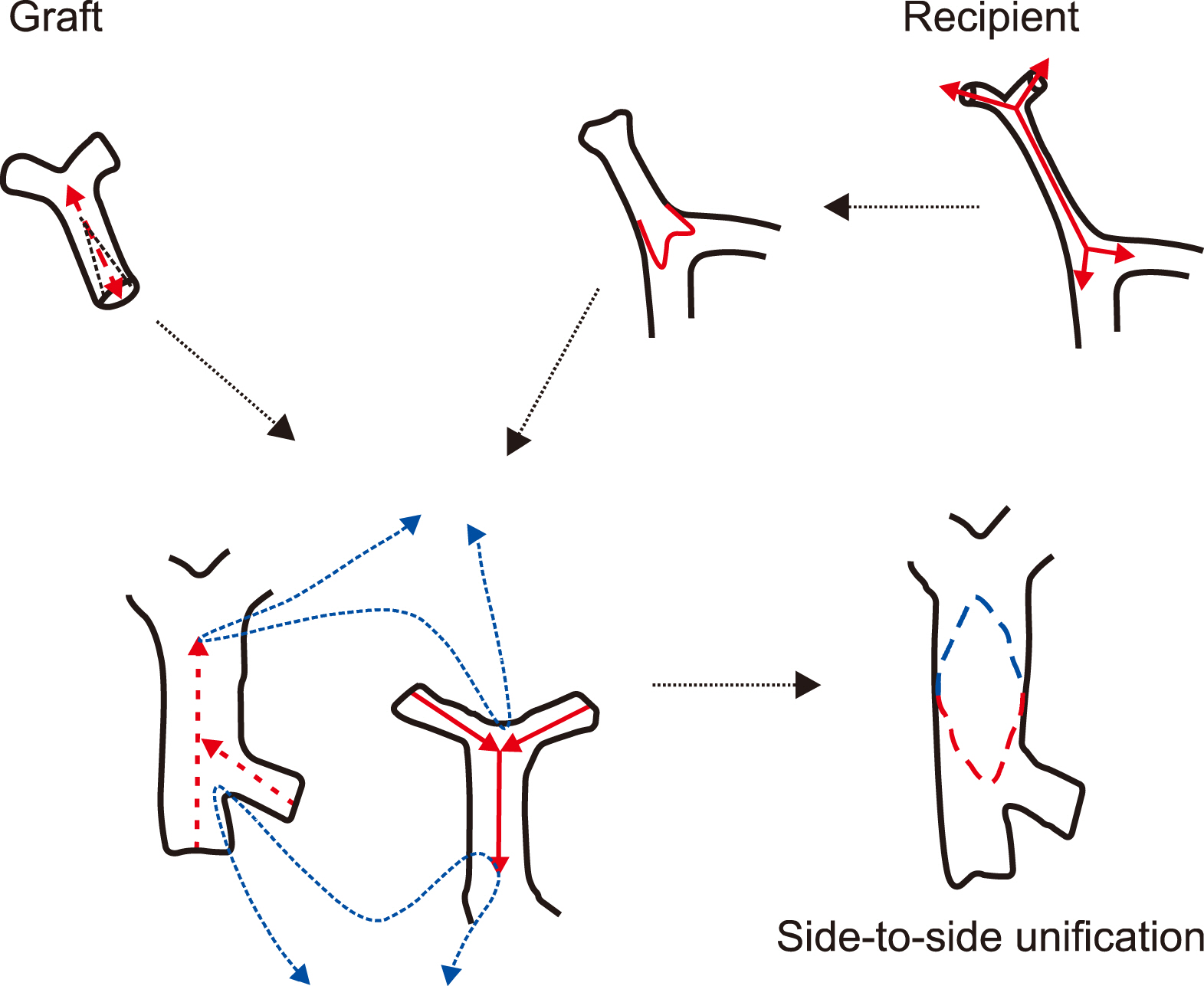
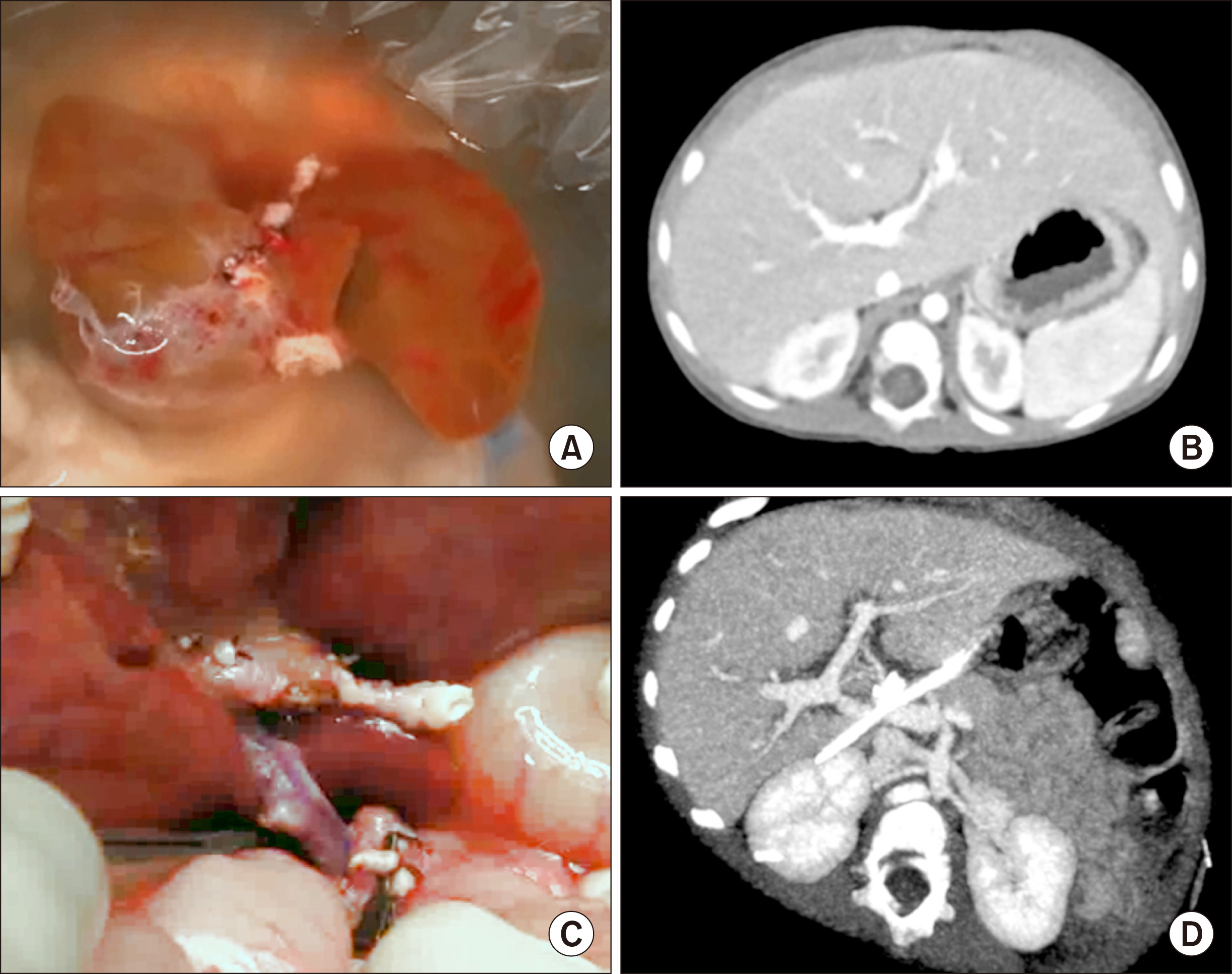
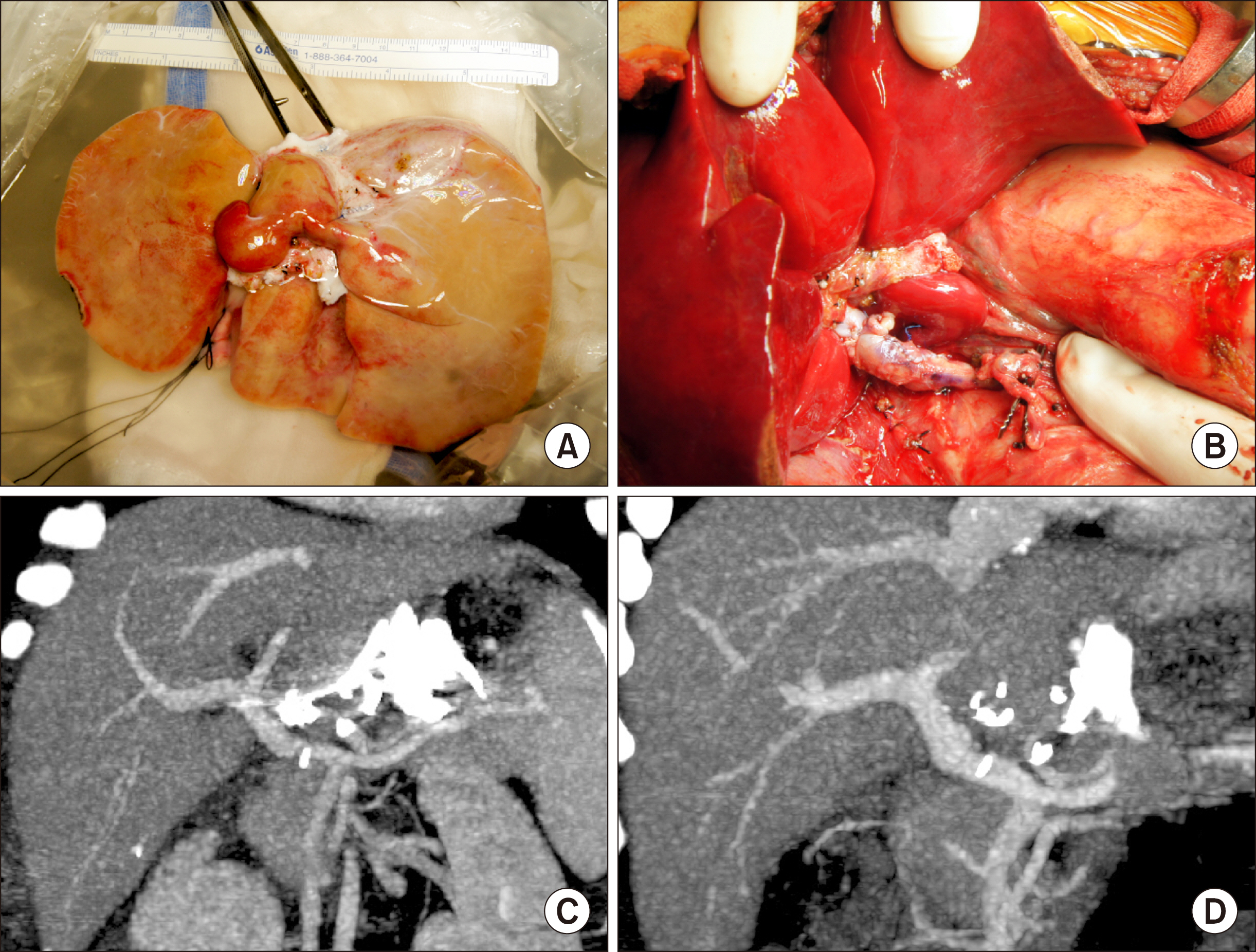
- Infant-to-infant whole liver transplantation (I2I-WLT) has been rarely performed in Korea. Unlike living donor liver transplantation or split liver transplantation, the donor graft portal vein (PV) in I2I-WLT is very small in diameter, so risk of PV complications increases significantly. We present two cases of I2I-WLT with application of side-to-side unification venoplasty for secure PV reconstruction. The first case recipient was a 10-month-old female baby who weighed 6.0 kg. She was diagnosed with progressive familial intrahepatic cholestasis. The deceased donor was a 12-month-old boy. The graft weight was 245 g, so the graft-recipient weight ratio (GRWR) was 4.1%. PV was reconstructed using side-to-side unification venoplasty. The function of graft liver recovered uneventfully and there was no evidence of PV complications. She is currently doing well for 4 years. The second case recipient was a 10-month-old female baby who weighed 8.8 kg. She had also undergone Kasai operation for biliary atresia. GRWR was 6.0%. Because the graft liver was much larger than the native liver, we designed the length of the extrahepatic PV more redundant than the precedent cases to avoid extrinsic compression by the large-sized caudate lobe. The PV was reconstructed using side-to-side unification venoplasty. The function of the graft liver recovered uneventfully. There was no evidence of PV complications. She is currently doing well for 2 years. As the PV size in infant donors and recipients is very small,PV reconstruction in I2I-WLT requires specialized surgical techniques of side-to-side unification venoplasty. Three supplementary video clips are provided.
Figure
Cited by 4 articles
-
Korea-nationwide incidence of pediatric deceased donors and single-institutional status of liver transplantation using pediatric donor liver grafts
Jung-Man Namgung, Shin Hwang, Chul-Soo Ahn, Ki-Hun Kim, Deok-Bog Moon, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park, Dea-Yeon Kim, Kyung Mo Kim, Seak Hee Oh, Sung-Gyu Lee
Korean J Transplant. 2020;34(3):178-184. doi: 10.4285/kjt.2020.34.3.178.Portal vein reconstruction using side-to-side unification technique for infant-to-infant deceased donor whole liver transplantation
Jung-Man Namgoong, Shin Hwang, Chul-Soo Ahn, Kyoung-Mo Kim, Seok-Hee Oh, Dae-Yeon Kim, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park
Ann Hepatobiliary Pancreat Surg. 2020;24(4):445-453. doi: 10.14701/ahbps.2020.24.4.445.Whole liver deceased donor liver transplantation for pediatric recipients: single-center experience for 20 years
Jung-Man Namgoong, Shin Hwang, Dae-Yeon Kim, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park, Kyung Mo Kim, Seak Hee Oh
Korean J Transplant. 2020;34(4):249-256. doi: 10.4285/kjt.20.0036.Liver transplantation in pediatric patients with progressive familial intrahepatic cholestasis: Single center experience of seven cases
Jung-Man Namgoong, Shin Hwang, Hyunhee Kwon, Suhyeon Ha, Kyung Mo Kim, Seak Hee Oh, Seung-Mo Hong
Ann Hepatobiliary Pancreat Surg. 2022;26(1):69-75. doi: 10.14701/ahbps.21-114.
Reference
-
1. Hwang S, Kim DY, Ahn CS, Moon DB, Kim KM, Park GC, et al. 2013; Computational simulation-based vessel interposition reconstruction technique for portal vein hypoplasia in pediatric liver transplantation. Transplant Proc. 45:255–258. DOI: 10.1016/j.transproceed.2012.05.090. PMID: 23375311.
Article2. Mitchell A, John PR, Mayer DA, Mirza DF, Buckels JA. , De Ville De Goyet J. 2002; Improved technique of portal vein reconstruction in pediatric liver transplant recipients with portal vein hypoplasia. Transplantation. 73:1244–1247. DOI: 10.1097/00007890-200204270-00009. PMID: 11981415.
Article3. Takahashi Y, Nishimoto Y, Matsuura T, Hayashida M, Tajiri T, Soejima Y, et al. 2009; Surgical complications after living donor liver transplantation in patients with biliary atresia: a relatively high incidence of portal vein complications. Pediatr Surg Int. 25:745–751. DOI: 10.1007/s00383-009-2430-y. PMID: 19655151.
Article4. Ueda M, Egawa H, Ogawa K, Uryuhara K, Fujimoto Y, Kasahara M, et al. 2005; Portal vein complications in the long-term course after pediatric living donor liver transplantation. Transplant Proc. 37:1138–1140. DOI: 10.1016/j.transproceed.2005.01.044. PMID: 15848648.
Article5. Kasahara M, Umeshita K, Sakamoto S, Fukuda A, Furukawa H, Uemoto S. 2017; Liver transplantation for biliary atresia: a systematic review. Pediatr Surg Int. 33:1289–1295. DOI: 10.1007/s00383-017-4173-5. PMID: 28983725.
Article6. Gu LH, Fang H, Li FH, Zhang SJ, Han LZ, Li QG. 2015; Preoperative hepatic hemodynamics in the prediction of early portal vein thrombosis after liver transplantation in pediatric patients with biliary atresia. Hepatobiliary Pancreat Dis Int. 14:380–385. DOI: 10.1016/S1499-3872(15)60377-0. PMID: 26256082.
Article7. Yeh YT, Chen CY, Tseng HS, Wang HK, Tsai HL, Lin NC, et al. 2017; Enlarging vascular stents after pediatric liver transplantation. J Pediatr Surg. 52:1934–1939. DOI: 10.1016/j.jpedsurg.2017.08.060. PMID: 28927979.
Article8. Ko GY, Sung KB, Lee S, Yoon HK, Kim KR, Kim KM, et al. 2007; Stent placement for the treatment of portal vein stenosis or occlusion in pediatric liver transplant recipients. J Vasc Interv Radiol. 18:1215–1221. DOI: 10.1016/j.jvir.2007.06.029. PMID: 17911510.
Article9. Yabuta M, Shibata T, Shibata T, Shinozuka K, Isoda H, Okamoto S, et al. 2014; Long-term outcome of percutaneous transhepatic balloon angioplasty for portal vein stenosis after pediatric living donor liver transplantation: a single institute's experience. J Vasc Interv Radiol. 25:1406–1412. DOI: 10.1016/j.jvir.2014.03.034. PMID: 24854391.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tailored standardization of portal vein reconstruction for pediatric liver transplantation at Asan Medical Center
- End-to-side jump graft from superior mesenteric vein for portal vein reconstruction in pediatric liver transplantation: a case report
- Portal vein reconstruction using side-to-side unification technique for infant-to-infant deceased donor whole liver transplantation
- Portal flow augmentation using meso-reno-portal anastomosis during liver transplantation with severe portal vein thrombosis
- Portal vein fenestration: a case report of an unusual portal vein developmental anomaly