Investig Magn Reson Imaging.
2019 Dec;23(4):316-327. 10.13104/imri.2019.23.4.316.
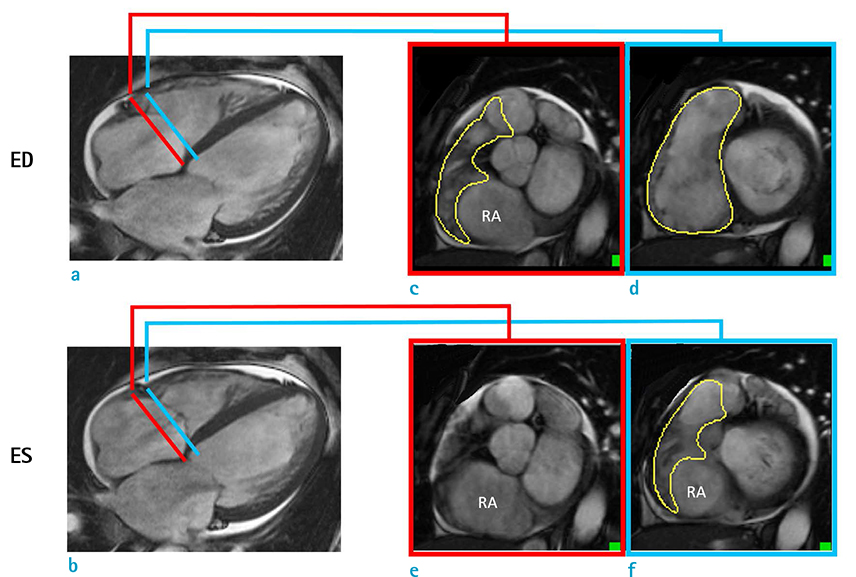
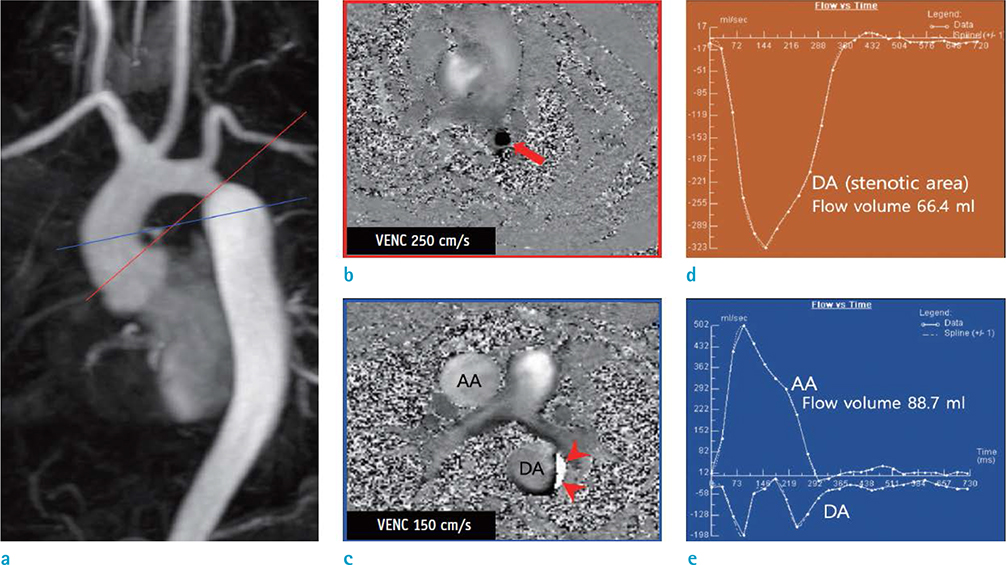
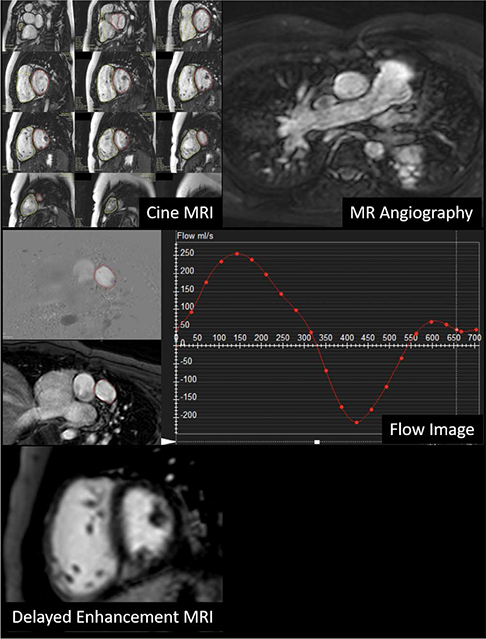
Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging (KOSCI) - Part 2: Interpretation of Cine, Flow, and Angiography Data
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Hospital Bucheon, Bucheon, Korea.
- 2Department of Radiology, Hanil General Hospital, Seoul, Korea.
- 3Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Seoul, Korea. donghyun.yang@gmail.com
- 4Department of Radiology, Eunpyeong St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. leebae@catholic.ac.kr
- 5Department of Radiology, Research Institute of Radiological Science, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 6Department of Radiology, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea.
- 7Department of Radiology, Seoul National University Hospital, Seoul, Korea.
- 8Department of Radiology, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea.
- 9Department of Radiology, Jeju National University Hospital, Jeju, Korea.
- 10Department of Radiology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
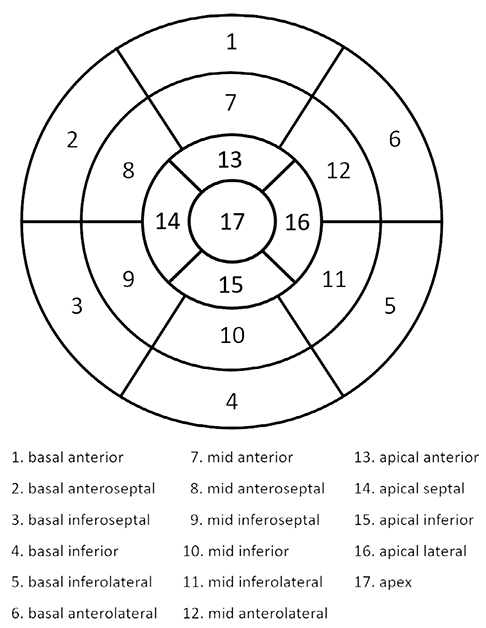
- 11Department of Radiology, Korea University Guro Hospital, Seoul, Korea.
- KMID: 2468049
- DOI: http://doi.org/10.13104/imri.2019.23.4.316
Abstract
- Cardiovascular magnetic resonance imaging (CMR) is expected to be increasingly used in Korea due to technology advances and the expanded national insurance coverage of these tests. For improved patient care, it is crucial not only that CMR images are properly acquired but that they are accurately interpreted by well-trained personnel. In response to the increased demand for CMR, the Korean Society of Cardiovascular Imaging (KOSCI) has issued interpretation guidelines in conjunction with the Korean Society of Radiology (KSR). KOSCI has also created a formal Committee on CMR Guidelines to write updated practices. The members of this Committee review previously published interpretation guidelines and discuss the patterns of CMR use in Korea.
Figure
Reference
-
1. Yoon YE, Hong YJ, Kim HK, et al. 2014 Korean guidelines for appropriate utilization of cardiovascular magnetic resonance imaging: a joint report of the Korean Society of Cardiology and the Korean Society of Radiology. Korean Circ J. 2014; 44:359–385.2. Kim YJ, Yong HS, Kim SM, et al. Korean guidelines for the appropriate use of cardiac CT. Korean J Radiol. 2015; 16:251–285.3. ASCI Practice Guideline Working Group. Beck KS, Kim JA, et al. 2017 multimodality appropriate use criteria for noninvasive cardiac imaging: expert consensus of the Asian Society of Cardiovascular Imaging. Korean J Radiol. 2017; 18:871–880.4. Goo HW. Comparison between three-dimensional navigator-gated whole-heart MRI and two-dimensional cine MRI in quantifying ventricular volumes. Korean J Radiol. 2018; 19:704–714.5. Cui C, Yin G, Lu M, et al. Retrospective electrocardiographygated real-time cardiac cine MRI at 3T: comparison with conventional segmented cine MRI. Korean J Radiol. 2019; 20:114–125.6. Goo HW. Semiautomatic three-dimensional threshold-based cardiac computed tomography ventricular volumetry in repaired tetralogy of Fallot: comparison with cardiac magnetic resonance imaging. Korean J Radiol. 2019; 20:102–113.7. Lee JW, Jeong YJ, Lee G, et al. Predictive value of cardiac magnetic resonance imaging-derived myocardial strain for poor outcomes in patients with acute myocarditis. Korean J Radiol. 2017; 18:643–654.8. Pizzino F, Recupero A, Pugliatti P, Maffei S, Di Bella G. Re: multi-parameter CMR approach in acute myocarditis to improve diagnosis and prognostic stratification. Korean J Radiol. 2018; 19:366–367.9. Lee HG, Shim J, Choi JI, Kim YH, Oh YW, Hwang SH. Use of cardiac computed tomography and magnetic resonance imaging in case management of atrial fibrillation with catheter ablation. Korean J Radiol. 2019; 20:695–708.10. Min JY, Ko SM, Song IY, Yi JG, Hwang HK, Shin JK. Comparison of the diagnostic accuracies of 1.5T and 3T stress myocardial perfusion cardiovascular magnetic resonance for detecting significant coronary artery disease. Korean J Radiol. 2018; 19:1007–1102.11. Lim J, Park EA, Song YS, Lee W. Single-dose gadoterate meglumine for 3T late gadolinium enhancement MRI for the assessment of chronic myocardial infarction: intra-individual comparison with conventional double-dose 1.5T MRI. Korean J Radiol. 2018; 19:372–338.12. Wang L, Chen Y, Zhang B, et al. Self-gated late gadolinium enhancement at 7T to image rats with reperfused acute myocardial infarction. Korean J Radiol. 2018; 19:247–255.13. Chen Y, Zheng X, Jin H, et al. Role of myocardial extracellular volume fraction measured with magnetic resonance imaging in the prediction of left ventricular functional outcome after revascularization of chronic total occlusion of coronary arteries. Korean J Radiol. 2019; 20:83–93.14. Karimi S, Pourmehdi M, Naderi M. Re: prediction of the left ventricular functional outcome by myocardial extracellular volume fraction measured using magnetic resonance imaging: methodological issue. Korean J Radiol. 2019; 20:1001–1002.15. Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002; 105:539–554.16. Hundley WG, Bluemke D, Bogaert JG, et al. Society for Cardiovascular Magnetic Resonance guidelines for reporting cardiovascular magnetic resonance examinations. J Cardiovasc Magn Reson. 2009; 11:5.17. Schulz-Menger J, Bluemke DA, Bremerich J, et al. Standardized image interpretation and post processing in cardiovascular magnetic resonance: Society for Cardiovascular Magnetic Resonance (SCMR) board of trustees task force on standardized post processing. J Cardiovasc Magn Reson. 2013; 15:35.18. Maceira AM, Prasad SK, Khan M, Pennell DJ. Normalized left ventricular systolic and diastolic function by steady state free precession cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2006; 8:417–426.19. Hudsmith LE, Petersen SE, Francis JM, Robson MD, Neubauer S. Normal human left and right ventricular and left atrial dimensions using steady state free precession magnetic resonance imaging. J Cardiovasc Magn Reson. 2005; 7:775–782.20. Hamdan A, Kelle S, Schnackenburg B, Fleck E, Nagel E. Improved quantitative assessment of left ventricular volumes using TGrE approach after application of extracellular contrast agent at 3 Tesla. J Cardiovasc Magn Reson. 2007; 9:845–853.21. Thiele H, Paetsch I, Schnackenburg B, et al. Improved accuracy of quantitative assessment of left ventricular volume and ejection fraction by geometric models with steady-state free precession. J Cardiovasc Magn Reson. 2002; 4:327–339.22. Puntmann VO, Gebker R, Duckett S, et al. Left ventricular chamber dimensions and wall thickness by cardiovascular magnetic resonance: comparison with transthoracic echocardiography. Eur Heart J Cardiovasc Imaging. 2013; 14:240–246.23. Alfakih K, Plein S, Thiele H, Jones T, Ridgway JP, Sivananthan MU. Normal human left and right ventricular dimensions for MRI as assessed by turbo gradient echo and steady-state free precession imaging sequences. J Magn Reson Imaging. 2003; 17:323–329.24. Alfakih K, Plein S, Bloomer T, Jones T, Ridgway J, Sivananthan M. Comparison of right ventricular volume measurements between axial and short axis orientation using steady-state free precession magnetic resonance imaging. J Magn Reson Imaging. 2003; 18:25–32.25. Clarke CJ, Gurka MJ, Norton PT, Kramer CM, Hoyer AW. Assessment of the accuracy and reproducibility of RV volume measurements by CMR in congenital heart disease. JACC Cardiovasc Imaging. 2012; 5:28–37.26. Mohiaddin RH, Kilner PJ, Rees S, Longmore DB. Magnetic resonance volume flow and jet velocity mapping in aortic coarctation. J Am Coll Cardiol. 1993; 22:1515–1521.27. Mohiaddin RH, Pennell DJ. MR blood flow measurement. Clinical application in the heart and circulation. Cardiol Clin. 1998; 16:161–187.28. Rebergen SA, van der Wall EE, Doornbos J, de Roos A. Magnetic resonance measurement of velocity and flow: technique, validation, and cardiovascular applications. Am Heart J. 1993; 126:1439–1456.29. O'Brien KR, Cowan BR, Jain M, Stewart RA, Kerr AJ, Young AA. MRI phase contrast velocity and flow errors in turbulent stenotic jets. J Magn Reson Imaging. 2008; 28:210–218.30. Holland BJ, Printz BF, Lai WW. Baseline correction of phase-contrast images in congenital cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2010; 12:11.31. Chernobelsky A, Shubayev O, Comeau CR, Wolff SD. Baseline correction of phase contrast images improves quantification of blood flow in the great vessels. J Cardiovasc Magn Reson. 2007; 9:681–685.32. Holloway BJ, Rosewarne D, Jones RG. Imaging of thoracic aortic disease. Br J Radiol. 2011; 84 Spec No 3:S338–S354.33. Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/ AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. J Am Coll Cardiol. 2010; 55:e27–e129.34. Glockner JF. MR angiography interpretation: techniques and pitfalls. Magn Reson Imaging Clin N Am. 2005; 13:23–40.35. Kalb B, Sharma P, Tigges S, et al. MR imaging of pulmonary embolism: diagnostic accuracy of contrast-enhanced 3D MR pulmonary angiography, contrast-enhanced lowflip angle 3D GRE, and nonenhanced free-induction FISP sequences. Radiology. 2012; 263:271–278.36. Grosse-Wortmann L, Al-Otay A, Goo HW, et al. Anatomical and functional evaluation of pulmonary veins in children by magnetic resonance imaging. J Am Coll Cardiol. 2007; 49:993–1002.37. Sakuma H, Ichikawa Y, Chino S, Hirano T, Makino K, Takeda K. Detection of coronary artery stenosis with whole-heart coronary magnetic resonance angiography. J Am Coll Cardiol. 2006; 48:1946–1950.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging—Part 2: Interpretation of Cine, Flow, and Angiography Data
- Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging—Part 2: Interpretation of Cine, Flow, and Angiography Data
- Imaging Forum in Cardiovascular Disease of the Korean Society of Cardiovascular Imaging
- Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging (KOSCI) - Part 3: Perfusion, Delayed Enhancement, and T1- and T2 Mapping
- Comparison of Cine Magnetic Resonance Imaging with Doppler Echocardiography for the Quantative Evaluation of Tricuspid Regurgitation in Newborn