Kosin Med J.
2019 Dec;34(2):95-105. 10.7180/kmj.2019.34.2.95.
Cribriform Pattern at the Surgical Margin is Highly Predictive of Biochemical Recurrence in Patients Undergoing Radical Prostatectomy
- Affiliations
-
- 1Department of Urology, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea. hongkooha@naver.com
- 2Department of Urology, Inje University Busan Paik Hospital, Busan, Korea.
- 3Department of Pathology, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea.
- 4Biomedical Research Institute, Pusan National University Hospital, Busan, Korea.
- KMID: 2467970
- DOI: http://doi.org/10.7180/kmj.2019.34.2.95
Abstract
OBJECTIVES
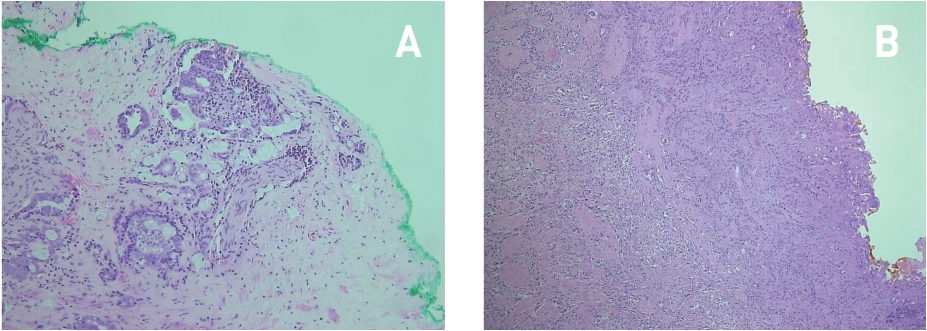
We investigated the relationship between cribriform patterns and biochemical recurrence in patients with positive surgical margins after radical prostatectomy.
METHODS
This study was based on radical prostatectomy specimens obtained from 817 patients (165 with margin-positive status) collected at a single center between 2010 and 2016. We retrospectively analyzed and compared body mass index, preoperative prostate-specific antigen, Gleason score, operative methods, postoperative Gleason score, pathological T-stage, tumor percentage involvement, lymphatic and perineural invasion, prostate-specific antigen nadir, location and length of the positive margin, cribriform pattern status, and Gleason grade at the surgical margin in terms of their association with biochemical recurrence. Risk factors for biochemical recurrence were also investigated.
RESULTS
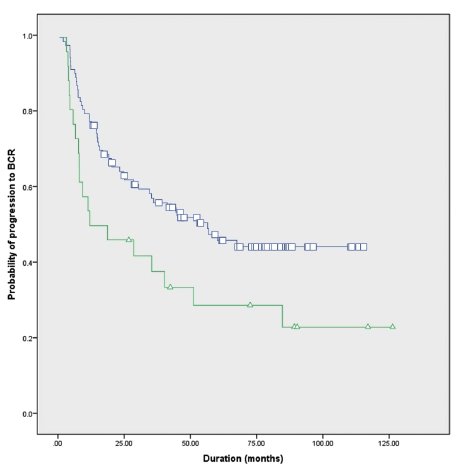
21% (31/146) of surgical margin-positive patients had a cribriform pattern. Nadir prostate-specific antigen, perineural invasion and biochemical recurrence rates were significantly higher in cribriform pattern present group than absent group (P = 0.031, 0.043 and 0.045, respectively). According to the Cox regression model, postoperative Gleason score, tumor percentage involvement, location and length of the positive margin, and the presence of a cribriform pattern at the surgical margin were significant predictive factors of biochemical recurrence (P = 0.022, < 0.001, 0.015, 0.001, and 0.022, respectively). Moreover, the biochemical recurrence risk was approximately 3-fold higher in patients with a cribriform pattern at the surgical margin than in those without (HR: 3.41, 95% CI 1.20-9.70, P = 0.022).
CONCLUSIONS
A cribriform pattern at the surgical margin is a significant predictor of biochemical recurrence in patients who undergo radical prostatectomy.
MeSH Terms
Figure
Reference
-
1. Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA, et al. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of grading patterns and proposal for a new grading system. Am J Surg Pathol. 2016; 40:244–252.
Article2. Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL. ISUP Grading Committee. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol. 2005; 29:1228–1242.
Article3. Iczkowski KA, Torkko KC, Kotnis GR, Wilson RS, Huang W, Wheeler TM, et al. Digital quantification of five high-grade prostate cancer patterns, including the cribriform pattern, and their association with adverse outcome. Am J Clin Pathol. 2011; 136:98–107.
Article4. Dong F, Yang P, Wang C, Wu S, Xiao Y, Mc-Dougal WS, et al. Architectural heterogeneity and cribriform pattern predict adverse clinical outcome for Gleason grade 4 prostatic adenocarcinoma. Am J Surg Pathol. 2013; 37:1855–1861.
Article5. Kweldam CF, Kümmerlin IP, Nieboer D, Verhoef EI, Steyerberg EW, Incrocci L, et al. Prostate cancer outcomes of men with biopsy Gleason score 6 and 7 without cribriform or intraductal carcinoma. Eur J Cancer. 2016; 66:26–33.
Article6. Kweldam CF, Wildhagen MF, Steyerberg EW, Bangma CH, van der Kwast TH, van Leenders GJ. Cribriform growth is highly predictive for postoperative metastasis and disease-specific death in Gleason score 7 prostate cancer. Mod Pathol. 2015; 28:457–464.
Article7. Kweldam CF, Kümmerlin IP, Nieboer D, Verhoef EI, Steyerberg EW, van der Kwast TH, et al. Disease-specific survival of patients with invasive cribriform and intraductal prostate cancer at diagnostic biopsy. Mod Pathol. 2016; 29:630–636.
Article8. Shen S, Lepor H, Yaffee R, Taneja SS. Ultrasensitive serum prostate specific antigen nadir accurately predicts the risk of early relapse after radical prostatectomy. J Urol. 2005; 173:777–780.
Article9. Song C, Kang T, Yoo S, Jeong IG, Ro JY, Hong JH, et al. Tumor volume, surgical margin, and the risk of biochemical recurrence in men with organ-confined prostate cancer. Urol Oncol. 2013; 31:168–174.
Article10. Hsu M, Chang SL, Ferrari M, Nolley R, Presti JC Jr, Brooks JD. Length of site-specific positive surgical margins as a risk factor for biochemical recurrence following radical prostatectomy. Int J Urol. 2011; 18:272–279.
Article11. Han M, Partin AW, Zahurak M, Piantadosi S, Epstein JI, Walsh PC. Biochemical (prostate specific antigen) recurrence probability following radical prostatectomy for clinically localized prostate cancer. J Urol. 2003; 169:517–523.
Article12. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998; 280:969–974.13. Kinoshita H, Shimizu Y, Mizowaki T, Takayama K, Norihisa Y, Kamoto T, et al. Risk factors predicting the outcome of salvage radiotherapy in patients with biochemical recurrence after radical prostatectomy. Int J Urol. 2013; 20:806–812.
Article14. McKenney JK. The present and future of prostate cancer histopathology. Curr Opin Urol. 2017; 27:464–468.
Article15. Truong M, Frye T, Messing E, Miyamoto H. Historical and contemporary perspectives on cribriform morphology in prostate cancer. Nat Rev Urol. 2018; 15:475–482.
Article16. Kweldam CF, van der Kwast, van Leenders GJ. On cribriform prostate cancer. Transl Androl Urol. 2018; 7:145–154.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Impact of Positive Surgical Margins on Biochemical Recurrence after Radical Retropubic Prostatectomy
- Molecular risk classifier score and biochemical recurrence risk are associated with cribriform pattern type in Gleason 3+4=7 prostate cancer
- Influences of Neoadjuvant Androgen Ablation before Radical Prostatectomy on Positive Surgical Margin and Biochemical Recurrence Rate
- The Inpact of Positive Surgical Margins and Their Preoperative Predicting Factors on Biochemical Failure after Radical Retropubic Prostatectomy
- Biochemical Recurrence-Free and Cancer-Specific Survival after Radical Prostatectomy at a Single Institution