J Clin Neurol.
2020 Jan;16(1):124-130. 10.3988/jcn.2020.16.1.124.
Comparison of Neuropathic Pain in Neuromyelitis Optica Spectrum Disorder and Multiple Sclerosis
- Affiliations
-
- 1Department of Neurology, National Cancer Center, Goyang, Korea. hojinkim@ncc.re.kr
- 2Department of Neurology, Kosin University College of Medicine, Busan, Korea.
- 3Department of Neurology, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4Department of Neurology, Yeungnam University College of Medicine, Daegu, Korea.
- 5Department of Neurology, Konkuk University School of Medicine, Seoul, Korea.
- 6Department of Neurology, Ewha Womans University School of Medicine, Ewha Medical Research Institute, Seoul, Korea.
- KMID: 2467794
- DOI: http://doi.org/10.3988/jcn.2020.16.1.124
Abstract
- BACKGROUND AND PURPOSE
To compare the characteristics of neuropathic pain in neuromyelitis optica spectrum disorder (NMOSD) and multiple sclerosis (MS).
METHODS
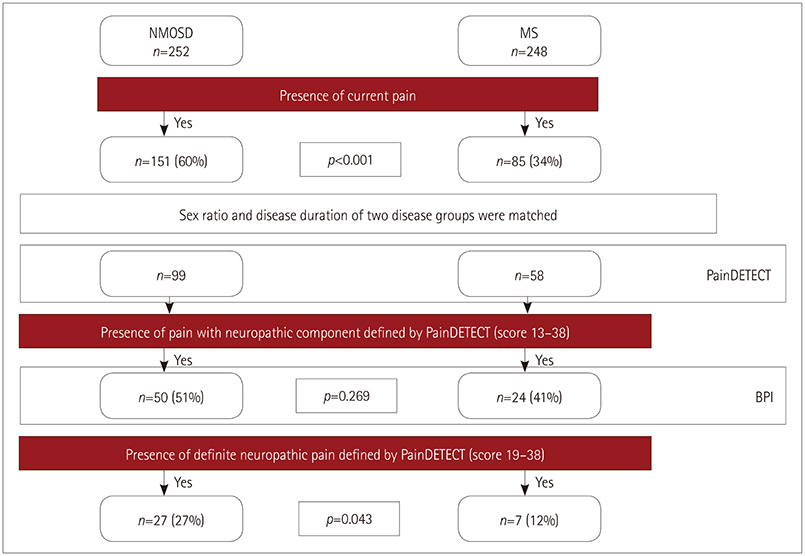
From 2016 to 2018, 500 patients with NMOSD and MS from 6 referral hospitals in Korea underwent pain investigation. After the patients with current pain were matched for sex ratio and disease duration as confounding factors, PainDETECT questionnaires were assessed in 99 NMOSD and 58 MS patients to investigate neuropathic pain. The short form of the Brief Pain Inventory from 74 patients with neuropathic pain component was also analysed.
RESULTS
According to the PainDETECT questionnaire, mechanical allodynia (p=0.014) and thermal hyperalgesia (p=0.011) were more severe in NMOSD patients than in MS patients. Strong involvements (score >3) of the pain in domains of tingling/prickling sensation (p=0.024), mechanical allodynia (p=0.027), sudden pain attacks (p=0.018), and thermal hyperalgesia (p=0.002) were significantly more frequent in NMOSD compared to MS patients. Among the patients experiencing pain with a neuropathic component, total pain-related interference (p=0.045) scores were significantly higher in NMOSD patients than in MS patients. In daily life, pain interfered with normal work (p=0.045) and relationships with other people (p=0.039) more often in NMOSD patients than in MS patients. Although pain medication was prescribed more frequently in NMOSD patients, the percentage of patients experiencing medication-related pain relief was lower in those patients.
CONCLUSIONS
The severity of neuropathic pain and the pain-related interference in daily life were greater in NMOSD patients than in MS patients. Individualized analgesic management should be considered based on a comprehensive understanding of neuropathic pain in these patients.
MeSH Terms
Figure
Cited by 1 articles
-
Investigation of serum biomarkers for neuropathic pain in neuromyelitis optica spectrum disorder: a preliminary study
Jae-Won Hyun, Yeseul Kim, Ho Jin Kim
Ann Clin Neurophysiol. 2021;23(1):46-52. doi: 10.14253/acn.2021.23.1.46.
Reference
-
1. International Association for the Study of Pain (IASP). IASP taxonomy. Pain terms. Neuropathic pain [Internet]. Washington, DC: IASP;2017. 12. 14. cited 2019 Apr 1. Available from: www.iasp-pain.org/terminology.2. Bradl M, Kanamori Y, Nakashima I, Misu T, Fujihara K, Lassmann H, et al. Pain in neuromyelitis optica--prevalence, pathogenesis and therapy. Nat Rev Neurol. 2014; 10:529–536.
Article3. Solaro C, Trabucco E, Messmer Uccelli M. Pain and multiple sclerosis: pathophysiology and treatment. Curr Neurol Neurosci Rep. 2013; 13:320.
Article4. Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, et al. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet. 2004; 364:2106–2112.
Article5. Wingerchuk DM, Lennon VA, Lucchinetti CF, Pittock SJ, Weinshenker BG. The spectrum of neuromyelitis optica. Lancet Neurol. 2007; 6:805–815.
Article6. Kanamori Y, Nakashima I, Takai Y, Nishiyama S, Kuroda H, Takahashi T, et al. Pain in neuromyelitis optica and its effect on quality of life: a cross-sectional study. Neurology. 2011; 77:652–658.
Article7. Qian P, Lancia S, Alvarez E, Klawiter EC, Cross AH, Naismith RT. Association of neuromyelitis optica with severe and intractable pain. Arch Neurol. 2012; 69:1482–1487.
Article8. Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015; 85:177–189.
Article9. Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011; 69:292–302.
Article10. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL 3rd. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009; 10:447–485.
Article11. Freynhagen R, Baron R, Gockel U, Tölle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006; 22:1911–1920.
Article12. Sung JK, Choi JH, Jeong J, Kim WJ, Lee DJ, Lee SC, et al. Korean version of the painDETECT questionnaire: a study for cultural adaptation and validation. Pain Pract. 2017; 17:494–504.
Article13. Kim Y, Kim G, Kong BS, Lee JE, Oh YM, Hyun JW, et al. Large scale in-house cell based assay for the evaluation of serostatus in patients with neuromyelitis optica spectrum disorder based on new diagnostic criteria. J Clin Neurol. 2017; 13:175–180.
Article14. Yun YH, Mendoza TR, Heo DS, Yoo T, Heo BY, Park HA, et al. Development of a cancer pain assessment tool in Korea: a validation study of a Korean version of the brief pain inventory. Oncology. 2004; 66:439–444.
Article15. Nees TA, Finnerup NB, Blesch A, Weidner N. Neuropathic pain after spinal cord injury: the impact of sensorimotor activity. Pain. 2017; 158:371–376.
Article16. Zhao S, Mutch K, Elsone L, Nurmikko T, Jacob A. Neuropathic pain in neuromyelitis optica affects activities of daily living and quality of life. Mult Scler. 2014; 20:1658–1661.
Article17. Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983; 33:1444–1452.
Article18. Hahn HM, Yum TH, Shin YW, Kim KH, Yoon DJ, Chung KJ. A standardization study of beck depression inventory in Korea. J Korean Neuropsychiatr Assoc. 1986; 25:487–500.19. Lee JH, Jeong HS, Lim SM, Cho HB, Ma JY, Ko E, et al. Reliability and validity of the fatigue severity scale among university student in South Korea. Korean J Biol Psychiatry. 2013; 20:6–11.20. Freynhagen R, Tölle TR, Gockel U, Baron R. The painDETECT project - far more than a screening tool on neuropathic pain. Curr Med Res Opin. 2016; 32:1033–1057.
Article21. Heitmann H, Biberacher V, Tiemann L, Buck D, Loleit V, Selter RC, et al. Prevalence of neuropathic pain in early multiple sclerosis. Mult Scler. 2016; 22:1224–1230.
Article22. Olechowski CJ, Truong JJ, Kerr BJ. Neuropathic pain behaviours in a chronic-relapsing model of experimental autoimmune encephalomyelitis (EAE). Pain. 2009; 141:156–164.
Article23. Hyun JW, Kim SH, Jeong IH, Lee SH, Kim HJ. Bright spotty lesions on the spinal cord: an additional MRI indicator of neuromyelitis optica spectrum disorder? J Neurol Neurosurg Psychiatry. 2015; 86:1280–1282.
Article24. Nakamura M, Miyazawa I, Fujihara K, Nakashima I, Misu T, Watanabe S, et al. Preferential spinal central gray matter involvement in neuromyelitis optica. An MRI study. J Neurol. 2008; 255:163–170.
Article25. Gruber-Schoffnegger D, Drdla-Schutting R, Hönigsperger C, Wunderbaldinger G, Gassner M, Sandkühler J. Induction of thermal hyperalgesia and synaptic long-term potentiation in the spinal cord lamina I by TNF-α and IL-1β is mediated by glial cells. J Neurosci. 2013; 33:6540–6551.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differential Diagnosis between Multiple Sclerosis and Neuromyelitis Optica Spectrum Disorder
- Postpartum Relapse of Neuromyelitis Optica Spectrum Disorder after a Long Period of Spontaneous Remission
- Investigation of serum biomarkers for neuropathic pain in neuromyelitis optica spectrum disorder: a preliminary study
- Central Hyperthemia Treated with Bromocriptine in a Patient with Aquaporin 4 Antibody Positive Neuromyelitis Optica Spectrum Disorder
- Monoclonal Antibody Therapies for Multiple Sclerosis and Neuromyelitis Optica Spectrum Disorder