Ann Dermatol.
2020 Feb;32(1):64-68. 10.5021/ad.2020.32.1.64.
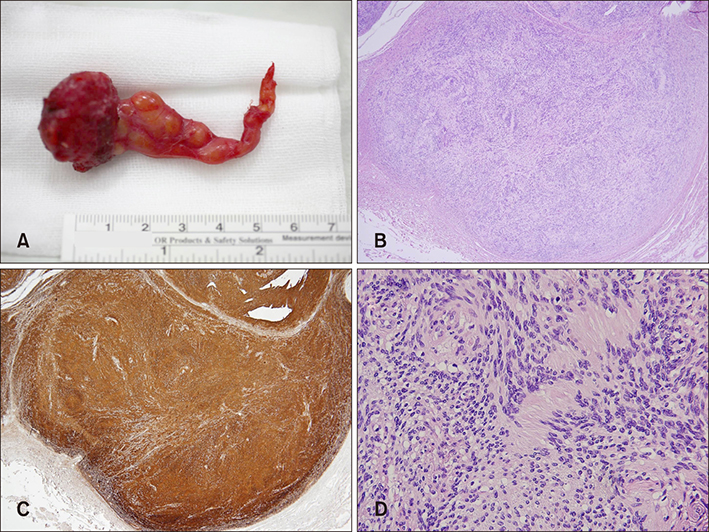
Schwannoma Presenting as a Scalp Mass: A Case Report with Magnetic Resonance Imaging Findings
- Affiliations
-
- 1Department of Dermatology, Seoul National University College of Medicine, Seoul, Korea. jehomun@gmail.com
- 2Institute of Human-Environment Interface Biology, Seoul National University, Seoul, Korea.
- KMID: 2467203
- DOI: http://doi.org/10.5021/ad.2020.32.1.64
Abstract
- A schwannoma can develop anywhere along the course of nerves. However, a schwannoma presenting as a scalp nodule is rare. Here, we present a rare case of schwannoma on the scalp with a review of magnetic resonance imaging (MRI) findings, which was initially misdiagnosed as an epidermal cyst or vascular malformation despite various radiologic examinations. Recognition of characteristic MRI features of schwannomas, such as low signal margin, target, entering-and-exiting-nerve, and fascicular signs, may result in an accurate diagnosis and proper management of tumors. In this report, we summarized differential characteristics of a schwannoma with an epidermal cyst and a lipoma.
MeSH Terms
Figure
Reference
-
1. Noh S, Do JE, Park JM, Jee H, Oh SH. Cutaneous schwannoma presented as a pedunculated protruding mass. Ann Dermatol. 2011; 23:Suppl 2. S264–S266.
Article2. Zhang H, Cai C, Wang S, Liu H, Ye Y, Chen X. Extracranial head and neck schwannomas: a clinical analysis of 33 patients. Laryngoscope. 2007; 117:278–281.
Article3. Colreavy MP, Lacy PD, Hughes J, Bouchier-Hayes D, Brennan P, O'Dwyer AJ, et al. Head and neck schwannomas--a 10 year review. J Laryngol Otol. 2000; 114:119–124.4. Asuquo ME, Nwagbara VI, Akpan SO, Otobo FO, Umeh J, Ebughe G, et al. Recurrent benign schwannoma of the scalp: Case report. Int J Surg Case Rep. 2013; 4:65–67.
Article5. Mohan Kh, Manjunath H. Cutaneous schwannoma masquerading as trichilemmal cyst over scalp in a young male. Indian J Dermatol. 2013; 58:407.
Article6. Kim YC, Park HJ, Cinn YW, Vandersteen DP. Benign glandular schwannoma. Br J Dermatol. 2001; 145:834–837.
Article7. Kang GC, Soo KC, Lim DT. Extracranial non-vestibular head and neck schwannomas: a ten-year experience. Ann Acad Med Singapore. 2007; 36:233–238.8. Yasumatsu R, Nakashima T, Miyazaki R, Segawa Y, Komune S. Diagnosis and management of extracranial head and neck schwannomas: a review of 27 cases. Int J Otolaryngol. 2013; 2013:973045.
Article9. Salunke AA, Chen Y, Tan JH, Chen X, Foo TL, Gartner LE, et al. Intramuscular schwannoma: clinical and magnetic resonance imaging features. Singapore Med J. 2015; 56:555–557.
Article10. Varma DG, Moulopoulos A, Sara AS, Leeds N, Kumar R, Kim EE, et al. MR imaging of extracranial nerve sheath tumors. J Comput Assist Tomogr. 1992; 16:448–453.
Article11. Petscavage-Thomas JM, Walker EA, Logie CI, Clarke LE, Duryea DM, Murphey MD. Soft-tissue myxomatous lesions: review of salient imaging features with pathologic comparison. Radiographics. 2014; 34:964–980.
Article12. Jee WH, Oh SN, McCauley T, Ryu KN, Suh JS, Lee JH, et al. Extraaxial neurofibromas versus neurilemmomas: discrimination with MRI. AJR Am J Roentgenol. 2004; 183:629–633.
Article13. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill;2012. p. 1333–1334. p. 1476–1477. p. 1489–1490.14. DiDomenico P, Middleton W. Sonographic evaluation of palpable superficial masses. Radiol Clin North Am. 2014; 52:1295–1305.
Article15. Kim HK, Kim SM, Lee SH, Racadio JM, Shin MJ. Subcutaneous epidermal inclusion cysts: ultrasound (US) and MR imaging findings. Skeletal Radiol. 2011; 40:1415–1419.
Article16. Wortsman X. Common applications of dermatologic sonography. J Ultrasound Med. 2012; 31:97–111.
Article17. Beaman FD, Kransdorf MJ, Andrews TR, Murphey MD, Arcara LK, Keeling JH. Superficial soft-tissue masses: analysis, diagnosis, and differential considerations. Radiographics. 2007; 27:509–523.
Article18. Skolnik AD, Loevner LA, Sampathu DM, Newman JG, Lee JY, Bagley LJ, et al. Cranial nerve schwannomas: diagnostic imaging approach. radiographics. 2016; 36:1463–1477.
Article19. Razek AA, Huang BY. Soft tissue tumors of the head and neck: imaging-based review of the WHO classification. Radiographics. 2011; 31:1923–1954.
Article20. De Schepper AM, Bloem JL. Soft tissue tumors: grading, staging, and tissue-specific diagnosis. Top Magn Reson Imaging. 2007; 18:431–444.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nipple Schwannoma: A Case Report and Literature Review on Nipple Mass
- Schwannoma of the Tongue Base with Imaging Features and Differential Diagnosis: a Rare Case Report and Literature Review
- Ancient Schwannoma at the Olfactory Groove Mimicking Meningioma: A Case Report
- A Case of Subcutaneous Schwannoma of the Scalp
- A case of Bell’s palsy with an incidental finding of facial nerve schwannoma: comparison of magnetic resonance imaging findings