Ann Dermatol.
2020 Feb;32(1):53-56. 10.5021/ad.2020.32.1.53.
Necrobiotic Xanthogranuloma Coexists with Diffuse Normolipidemic Plane Xanthoma and Multiple Myeloma
- Affiliations
-
- 1Department of Dermatology, Yeungnam University College of Medicine, Daegu, Korea. dhshin@med.yu.ac.kr
- 2Department of Pathology, Yeungnam University College of Medicine, Daegu, Korea.
- KMID: 2467201
- DOI: http://doi.org/10.5021/ad.2020.32.1.53
Abstract
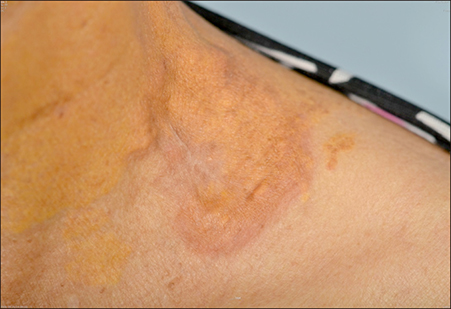
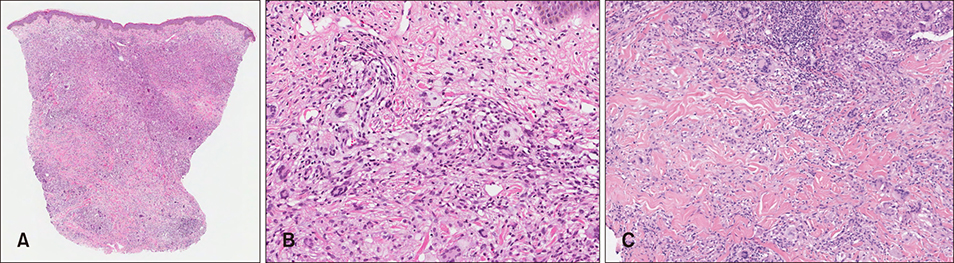
- Necrobiotic xanthogranuloma (NXG), is a rare multisystem disease that manifests as cutaneous inflammatory lesions, and is commonly associated with lymphoproliferative disease. Diffuse normolipemic plane xanthoma (NX), is also a rare, acquired disease that is often associated with systemic diseases such as lymphoproliferative disease. Both of these diseases have been reported to be associated with monoclonal gammopathy (MG). However, there are few cases in which these diseases co-exist. A 78-year-old female, who had a known case of NX on the neck and axillary area, presented with an asymptomatic erythematous plaque on her left supraclavicular area. Histopathological examination showed lymphoid aggregates, necrobiotic areas, and granulomatous inflammation in the dermis. Numerous foreignbody and Touton type giant cells were noticed. Serum protein immunoelectrophoresis showed an IgG kappa type MG. Lipid profile of the patient was normal. Bone marrow examination showed plasma cell myeloma. Based on these histologic and laboratory results, we diagnosed this lesion as NXG coexisting with NX and multiple myeloma. She was started on treatment with bortezomib and melphalan for multiple myeloma, and high-dose systemic corticosteroid and triamcinolone intralesional injection for the skin lesion. After 3 months of treatment, the NXG skin lesion and MG improved.
MeSH Terms
Figure
Reference
-
1. Yoon SY, Park HJ, Lee JY, Cho BK. Necrobiotic xanthogranuloma with multiple myeloma and no periorbital involvement. Ann Dermatol. 2007; 19:22–24.
Article2. Altman J, Winkelmann RK. Diffuse normolipemic plane xanthoma. Generalized xanthelasma. Arch Dermatol. 1962; 85:633–640.3. Rosmaninho A, Fernandes I, Guimas A, Amorim I, Selores M. Diffuse plane xanthomatosis associated with monoclonal gammopathy. An Bras Dermatol. 2011; 86:4 Suppl 1. S50–S52.
Article4. Szalat R, Arnulf B, Karlin L, Rybojad M, Asli B, Malphettes M, et al. Pathogenesis and treatment of xanthomatosis associated with monoclonal gammopathy. Blood. 2011; 118:3777–3784.
Article5. Parker F. Normocholesterolemic xanthomatosis. Arch Dermatol. 1986; 122:1253–1257.
Article6. Misselwitz B, Goede JS, Pestalozzi BC, Schanz U, Seebach JD. Hyperlipidemic myeloma: review of 53 cases. Ann Hematol. 2010; 89:569–577.
Article7. Mehregan DA, Winkelmann RK. Necrobiotic xanthogranuloma. Arch Dermatol. 1992; 128:94–100.
Article8. Spicknall KE, Mehregan DA. Necrobiotic xanthogranuloma. Int J Dermatol. 2009; 48:1–10.
Article9. Kourou K, Suga Y, Muramatsu S, Yaguchi H, Ogawa H. A case of diffuse plane normolipemic xanthomatosis associated with pancytopenia and monoclonal gammopathy. J Dermatol. 2006; 33:64–67.
Article10. Jeziorska M, Hassan A, Mackness MI, Woolley DE, Tullo AB, Lucas GS, et al. Clinical, biochemical, and immunohistochemical features of necrobiotic xanthogranulomatosis. J Clin Pathol. 2003; 56:64–68.
Article11. Matsuura F, Yamashita S, Hirano K, Ishigami M, Hiraoka H, Tamura R, et al. Activation of monocytes in vivo causes intracellular accumulation of lipoprotein-derived lipids and marked hypocholesterolemia--a possible pathogenesis of necrobiotic xanthogranuloma. Atherosclerosis. 1999; 142:355–365.
Article12. Szalat R, Pirault J, Fermand JP, Carrié A, Saint-Charles F, Olivier M, et al. Physiopathology of necrobiotic xanthogranuloma with monoclonal gammopathy. J Intern Med. 2014; 276:269–284.
Article13. Wruhs M, Feldmann R, Sawetz I, Breier F, Steiner A. Necrobiotic xanthogranuloma in a patient with multiple myeloma. Case Rep Dermatol. 2016; 8:350–353.
Article14. Xu G, Yang M, Qian W. Long-term disease control in a refractory multiple myeloma patient treated with bortezomib mono-therapy: a case report and review of literature. Int J Clin Exp Med. 2015; 8:19629–19631.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Generalized Plane Xanthoma Associated with Monoclonal Gammopathy of Unknown Significance
- Two Cases of Diffuse Plane Xanthoma
- Diffuse Normolipemic Plane Xanthoma with Multiple Myeloma
- Necrobiotic Xanthogranuloma with Multiple Myeloma and No Periorbital Involvement
- A Case of Diffuse Normolipemic Plane Xanthoma Associated with Multiple Myeloma