J Dent Anesth Pain Med.
2019 Dec;19(6):369-378. 10.17245/jdapm.2019.19.6.369.
Comparative evaluation of the effectiveness of a mobile app (Little Lovely Dentist) and the tell-show-do technique in the management of dental anxiety and fear: a randomized controlled trial
- Affiliations
-
- 1Department of Pediatric and Preventive Dentistry, Narayana Dental College and Hospital, Nellore, Andhra Pradesh, India. sujathasushant@gmail.com
- KMID: 2466652
- DOI: http://doi.org/10.17245/jdapm.2019.19.6.369
Abstract
- BACKGROUND
Behavior guidance is a technique used to subdue inappropriate behavior by establishing communication that meets the needs of a child. This study aimed to measure the effectiveness of a mobile app (Little Lovely Dentist) compared to the tell-show-do (TSD) technique in managing anxious children during their first dental visit.
METHODS
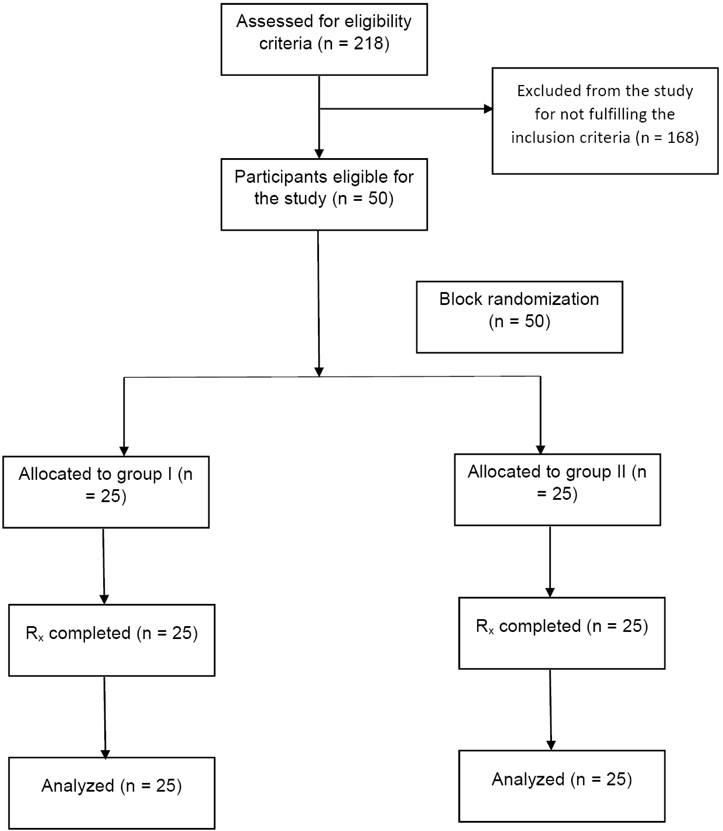
Fifty children (30 boys and 20 girls) without any past dental experience, aged from 7 to 11 years, were randomly allocated into either the dental app group or the TSD group. The pre- and post-operative anxiety of children who underwent prophylactic cleaning was assessed both physiologically and subjectively using a heart rate measurement and the RMS pictorial scale, respectively.
RESULTS
The intragroup comparison of heart rate and RMS scores for children allocated to the dental app group was statistically significant (P value ≤ 0.001). However, a significant reduction only occurred in the RMS scores, but not the heart rate measurements, in the TSD group. Conversely, there was an increase in heart rates in the TSD group.
CONCLUSION
Educating the child prior to a dental procedure using a smartphone application such as Little Lovely Dentist can significantly alleviate the anticipatory anxiety and engage children in dental treatment during their first visit.
Figure
Reference
-
1. Shetty RM, Khandelwal M, Rath S. RMS Pictorial Scale (RMS-PS): An innovative scale for the assessment of child's dental anxiety. J Indian Soc Pedod Prev Dent. 2015; 33:48–52.
Article2. Rantavuori K, Zerman N, Ferro R, Lahti S. Relationship between children's first dental visit and their dental anxiety in the Veneto Region of Italy. Acta Odontol Scand. 2002; 60:297–300.
Article3. Roshan NM, Virupaxi SG, Bharath KP, Poornima P, Nagaveni NB, Neena IE. A comparative study of filmed modeling and tell-show-do technique on anxiety in children undergoing dental treatment. J Oral Health Comm Dent. 2018; 12:20–24.
Article4. Darrow CW. Physiological and clinical tests of autonomic function and autonomic balance. Physiol Rev. 1943; 23:1–36.
Article5. Milgrom P, Mancl L, King B, Weinstein P. Origins of childhood dental fear. Behav Res Ther. 1995; 33:313–319.
Article6. Locker D, Shapiro D, Liddell A. Negative dental experiences and their relationship to dental anxiety. Community Dent Health. 1996; 13:86–92.7. Alwin NP, Murray JJ, Britton PG. An assessment of dental anxiety in children. Br Dent J. 1991; 171:201–207.
Article8. Raadal M, Milgrom P, Weinstein P, et al. The prevalence of dental anxiety in children from low-income families and its relationship to personality traits. J Dent Res. 1995; 74:1439–1443.
Article9. Cuthbert MI, Melamed BG. A screening device: children at risk for dental fears and management problems. ASDC J Dent Child. 1982; 49:432–436.10. Herbertt RM, Innes JM. Familiarization and preparatory information in the reduction of anxiety in child dental patients. ASDC J Dent Child. 1979; 46:319–323.11. Oosterink FM, de Jongh A, Aartman IH. What are people afraid of during dental treatment? Anxiety-provoking capacity of 67 stimuli characteristic of the dental setting. Eur J Oral Sci. 2008; 116:44–51.
Article12. Klingberg G, Broberg AG. Dental fear/anxiety and dental behaviour management problems in children and adolescents: a review of prevalence and concomitant psychological factors. Int J Paediatr Dent. 2007; 17:391–406.
Article13. Li HC, Lopez V. Children's Emotional Manifestation Scale: development and testing. J Clin Nurs. 2005; 14:223–229.
Article14. American Academy of Pediatric Dentistry. Behavior guidance for the pediatric dental patient. Pediatr Dent. 2017; 39:246–259.15. Wright GZ, Stigers JI. Non-pharmacologic management of children's behaviors. In : Dean JA, Avery DR, McDonald RE, editors. Dentistry for the Child and Adolescence. 9th ed.St. Louis: CV Mosby Co.;2011. p. 30–31.16. Townsend JA. Behaviour guidance of the paediatric dental patient. In : Casa Massimo PS, Fields HW, McTigue DJ, Nowak AJ, editors. Paediatric Dentistry: Infancy through Adolescence. 5th ed. Philadelphia: Elsevier Saunders;2013. p. 358.17. Addleston HK. Child patient training. Fortnightly Rev Chicago Dental Soc. 1959; 38:27–29.18. Fields HW Jr, Machen JB, Murphy MG. Acceptability of various management techniques relative to types of dental treatment. Ped Dent. 1984; 6:199–203.19. Cianetti S, Lombardo G, Lupatelli E, Pagano S, Abraha I, Montedori A, et al. Dental fear/anxiety among children and adolescents. A systematic review. Eur J Paediatr Dent. 2017; 18:121–130.20. Panchal V, Gurunathan D, Shanmugaavel AK. Smartphone application as an aid in determination of caries risk and prevention: A pilot study. Eur J Dent. 2017; 11:469–474.
Article21. Nuvvula S, Alahari S, Kamatham R, Challa RR. Effect of audiovisual distraction with 3D video glasses on dental anxiety of children experiencing administration of local analgesia: a randomised clinical trial. Eur Arch Paediatr Dent. 2015; 16:43–50.
Article22. Nunna M, Dasaraju RK, Kamatham R, Mallineni SK, Nuvvula S. Comparative evaluation of virtual reality distraction and counter-stimulation on dental anxiety and pain perception in children. J Dent Anesth Pain Med. 2019; 19:277–288.
Article23. Milgrom P, Weinstein P, Kleinknecht R, Getz T. Treating fearful dental patients: a clinical handbook. New York: Appleton;1985.24. Chellappah NK, Vignehsa H, Milgrom P, Lam LG. Prevalence of dental anxiety and fear in children in Singapore. Community Dent Oral Epidemiol. 1990; 18:269–271.
Article25. Davila JM, Menendez J. Relaxing effects of music in dentistry for mentally handicapped patients. Spec Care Dentist. 1986; 6:18–21.
Article26. Wright GZ, Alpern GD. Variables influencing children's co-operative behaviour at first dental visit. ASDC J Dent Child. 1971; 38:124–128.27. Aartman IH, Hoogstraten J, Schuurs AH. Self-report measurements of dental anxiety and fear in children: a critical assessment. ASDC J Dent Child. 1998; 65:252–258.28. Ayer WA Jr, Domoto PK, Gale EN, Joy ED Jr, Melamed BG. Overcoming dental fear: strategies for its prevention and management. J Am Dent Assoc. 1983; 107:18–27.
Article29. Wright GZ, Strakey PE, Gardner DE. Managing Children's behavior in the dental office. St. Louis: Mosby;1983.30. Feigal R. Pediatric behavior management through nonpharmacologic methods. Gen Dent. 1995; 43:327–332.31. Rosenberg HM. Behavior modification for the child dental patient. ASDC J Dent Child. 1974; 41:111–114.32. McKnight-Hanes C, Myers DR, Dushku JC, Davis HC. The use of behaviour management techniques by dentists across practitioner type, age, and geographic region. Pediatr Dent. 1993; 15:267–271.33. Vellody A, Sarda K, Pratap R, Thota H. Mobile Social Media, Proceedings of Mobile India, 6th International conference on COMmunication and NETwork. Jan 7–10; 2014. Last accessed on 08-11-2019. from URL: https://www.comsnets.org/archive/2014/doc/MI%202014_Session%204_Ashvin%20Vellody.pdf.34. Children's use of mobile phones-An international comparison Published in 2010 by the GSM Association and the Mobile Society Research Institute within NTT DOCOMO Inc, Japan, 2011.35. Vardeh D, Edwards RR, Jamison RN, Eccleston C. There's an app for that: mobile technology - Is a new advantage in managing chronic pain. Pain Clin Updates. 2013; 21:1–8.36. Khatoon B, Hill KB, Walmsley AD. Instant message in dental education. J Dent Educ. 2015; 79:1471–1478.37. Alklayb SA, Assery MK, Alqahtani A, Alanazi M, Pani SC. Comparison of the effectiveness of a mobile phone-based education program in educating mothers as oral health providers in two regions of Saudi Arabia. J Int Soc Prev Community Dent. 2017; 7:110–115.38. Myers DR, Kramer WS, Sullivan RE. A study of the heart action of the child dental patient. ASDC J Dent Child. 1972; 99–106.39. Pinkham JR. Fear of dentistry: a discussion of its usefulness to certain child dental patients. ASDC J Dent Child. 1983; 50:111–113.40. Simpson WJ, Ruzicka RL, Thomas NR. Physiologic responses of children to initial dental experience. ASDC J Dent Child. 1974; 41:465–470.41. Patil VH, Vaid K, Gokhale NS, Shah P, Mundada M, Hugar SM. Evaluation of effectiveness of dental apps in management of child behaviour: A pilot study. Int J Pedod Rehabil. 2017; 2:14–18.
Article42. Shah HA, Nanjunda Swamy KV, Kulkarni S, Choubey S. Evaluation of dental anxiety and hemodynamic changes (Sympatho-Adrenal Response) during various dental procedures using smartphone applications v/s traditional behaviour management techniques in pediatric patients. Int J Appl Res. 2017; 3:429–433.43. Lee JH, Jung HK, Lee GG, Kim HY, Park SG, Woo SC. Effect of behavioral intervention using smartphone application for preoperative anxiety in pediatric patients. Korean J Anesthesiol. 2013; 65:508–518.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the effectiveness of tell-show-do and ask-tell-ask in the management of dental fear and anxiety: a double-blinded randomized control trial
- Comparative evaluation of the effectiveness of two innovative methods in the management of anxiety in a dental office: a randomized controlled trial
- What is the gold standard of the dental anxiety scale?
- Effectiveness of a mobile app-based individualized non-pharmacological intervention on behavioral and psychological symptoms of dementia in community-dwelling older adults: Study protocol for a randomized control trial
- Effects of Mobile Phone-Based App Learning Compared to Computer-Based Web Learning on Nursing Students: Pilot Randomized Controlled Trial