Neonatal Med.
2019 Nov;26(4):233-239. 10.5385/nm.2019.26.4.233.
Povidone-Iodine Pleurodesis for Chylothorax in an Extremely Low Birth Weight Infant
- Affiliations
-
- 1Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Pediatrics, National Health Insurance Service Ilsan Hospital, Goyang, Korea. swyoon@nhimc.or.kr
- KMID: 2466645
- DOI: http://doi.org/10.5385/nm.2019.26.4.233
Abstract
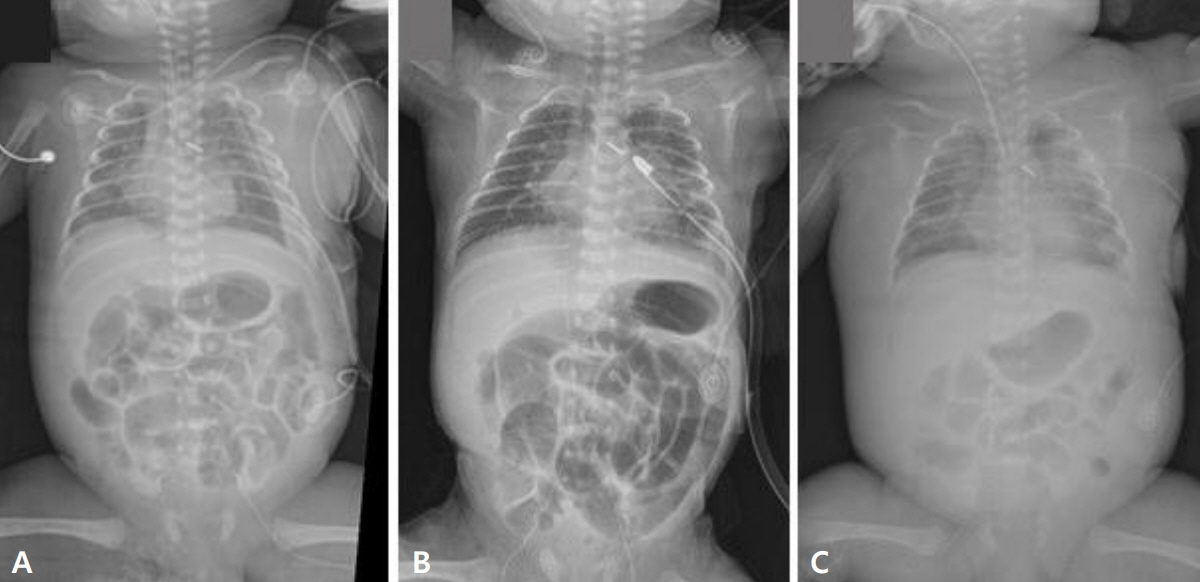
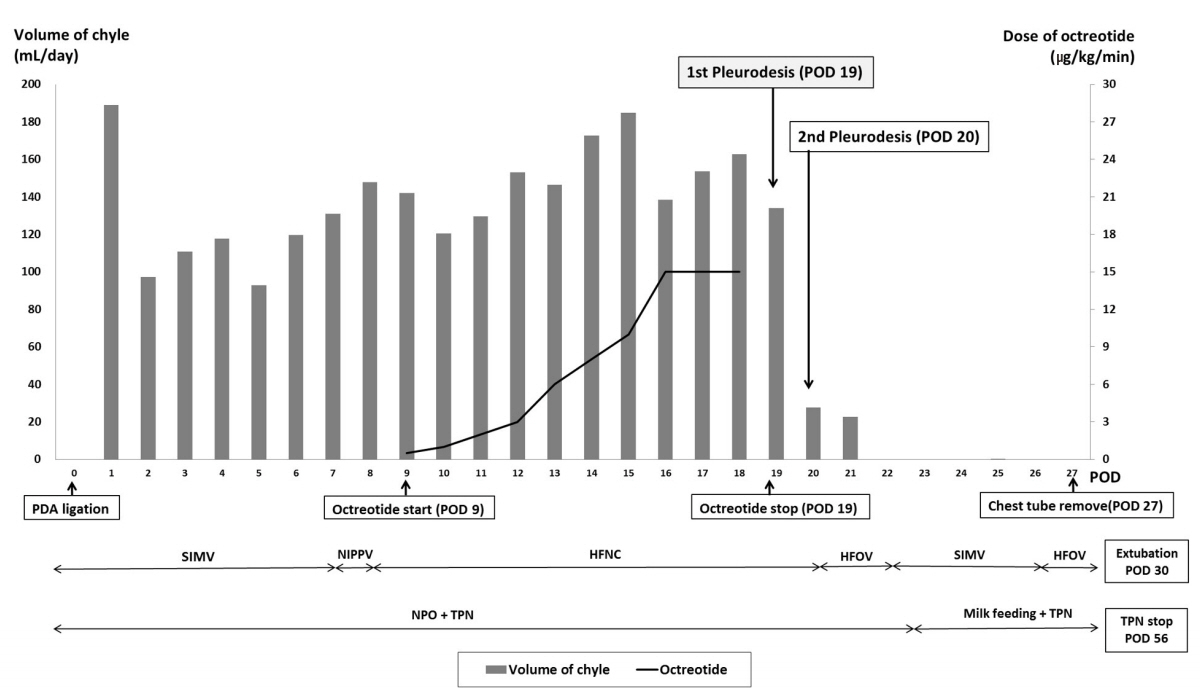
- Chylothorax, the accumulation of chyle in the pleural space, is a rare condition, but can lead to serious complications in neonates. Conservative therapy for chylothorax includes enteral feeding with medium-chain triglyceride-enriched diet or parenteral nutrition and administration of octreotide. Surgical management is considered in cases where there is no response to conservative therapy; however, the standardized approach to refractory neonatal chylothorax is still controversial. Chemical pleurodesis can be used when medical therapies for chylothorax fail, to avoid more invasive surgical procedures. We report an extremely preterm infant born at 26 weeks of gestation with refractory chylothorax after patent ductus arteriosus ligation. The infant was successfully treated with pleurodesis using 4% povidone-iodine, without long-term side effects.
Keyword
MeSH Terms
Figure
Reference
-
1. Matsuo S, Takahashi G, Konishi A, Sai S. Management of refractory chylothorax after pediatric cardiovascular surgery. Pediatr Cardiol. 2013; 34:1094–9.2. Tutor JD. Chylothorax in infants and children. Pediatrics. 2014; 133:722–33.3. Bialkowski A, Poets CF, Franz AR; Erhebungseinheit fur seltene padiatrische Erkrankungen in Deutschland Study Group. Congenital chylothorax: a prospective nationwide epidemiological study in Germany. Arch Dis Child Fetal Neonatal Ed. 2015; 100:F169–72.4. Roehr CC, Jung A, Proquitte H, Blankenstein O, Hammer H, Lakhoo K, et al. Somatostatin or octreotide as treatment options for chylothorax in young children: a systematic review. Intensive Care Med. 2006; 32:650–7.5. Das A, Shah PS. Octreotide for the treatment of chylothorax in neonates. Cochrane Database Syst Rev. 2010; 9:CD006388.6. Murki S, Faheemuddin M, Gaddam P. Congenital chylothorax: successful management with chemical pleurodesis. Indian J Pediatr. 2010; 77:332–4.7. Cho HJ, Na KJ, Kim DW, Choi YE, Ma JS, Jeong IS. Chemical pleurodesis using a Viscum album extract in infants with congenital chylothorax. Eur J Pediatr. 2014; 173:823–6.8. Utture A, Kodur V, Mondkar J. Chemical pleurodesis with oxytetracycline in congenital chylothorax. Indian Pediatr. 2016; 53:1105–6.9. Kim JE, Lee C, Park KI, Park MS, Namgung R, Park IK. Successful pleurodesis with OK-432 in preterm infants with persistent pleural effusion. Korean J Pediatr. 2012; 55:177–80.10. Brissaud O, Desfrere L, Mohsen R, Fayon M, Demarquez JL. Congenital idiopathic chylothorax in neonates: chemical pleurodesis with povidone-iodine (Betadine). Arch Dis Child Fetal Neonatal Ed. 2003; 88:F531–3.11. Wagenfeld L, Zeitz O, Richard G. Visual loss after povidoneiodine pleurodesis. N Engl J Med. 2007; 357:1264–5.12. Agarwal R, Aggarwal AN, Gupta D. Efficacy and safety of iodopovidone pleurodesis through tube thoracostomy. Respirology. 2006; 11:105–8.13. Mitanchez D, Walter-Nicolet E, Salomon R, Bavoux F, Hubert P. Congenital chylothorax: what is the best strategy? Arch Dis Child Fetal Neonatal Ed. 2006; 91:F153–4.14. Le Nue R, Molinaro F, Gomes-Ferreira C, Scheib-Brolly C, Escande B, Kuhn P, et al. Surgical management of congenital chylothorax in children. Eur J Pediatr Surg. 2010; 20:307–11.15. Arayici S, Simsek GK, Oncel MY, Yilmaz Y, Canpolat FE, Dilmen U. Povidone-iodine for persistent air leak in an extremely low birth weight infant. J Pediatr Surg. 2013; 48:E21–3.16. Hmami F, Oulmaati A, Bouchikhi C, Banani A, Bouharrou A. Congenital chylothorax: rapid and complete response to polyvidone iodine. Arch Pediatr. 2014; 21:1002–5.17. Scottoni F, Fusaro F, Conforti A, Morini F, Bagolan P. Pleurodesis with povidone-iodine for refractory chylothorax in newborns: personal experience and literature review. J Pediatr Surg. 2015; 50:1722–5.18. Resch B, Freidl T, Reiterer F. Povidone-iodine pleurodesis for congenital chylothorax of the newborn. Arch Dis Child Fetal Neonatal Ed. 2016; 101:F87–8.19. Kasdallah N, Kbaier H, Ben Salem H, Blibech S, Bouziri A, Douagi M. Povidone iodine pleurodesis for refractory congenital chylothorax: a review of literature. Tunis Med. 2016; 94:834.20. Borcyk K, Kamil A, Hagerty K, Deer M, Tomich P, Anderson Berry AL. Successful management of extremely high-output refractory congenital chylothorax with chemical pleurodesis using 4% povidone-iodine and propranolol: a case report. Clin Case Rep. 2018; 6:702–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Treatment of Intractable Chylo thorax with Povidone-Iodine Pleurodesis in Extremely Preterm Infant
- Two Cases of Allergic Contact Dermatitis due to Povidone-iodine
- Chemical Pleurodesis Using a Viscum album Extract in an Infant with Postoperative Chylothorax: A Case Report
- Effect of 1% Povidone-iodine for Ophthalmia Neonatorum Prophylaxis
- Primary Irritant Dermatitis to Povidone-Iodine after Caudal Anesthesia: A Case Report