Blood Res.
2019 Dec;54(4):282-284. 10.5045/br.2019.54.4.282.
EBV reactivation mimicking a lymphoproliferative disorder associated with ruxolitinib therapy for myelofibrosis
- Affiliations
-
- 1Division of Allo-BMT, Princess Margaret Centre, Toronto, ON, Canada.
- 2Division of Leukemia, Princess Margaret Centre, Toronto, ON, Canada. vikas.gupta@uhn.ca
- KMID: 2466594
- DOI: http://doi.org/10.5045/br.2019.54.4.282
Abstract
- No abstract available.
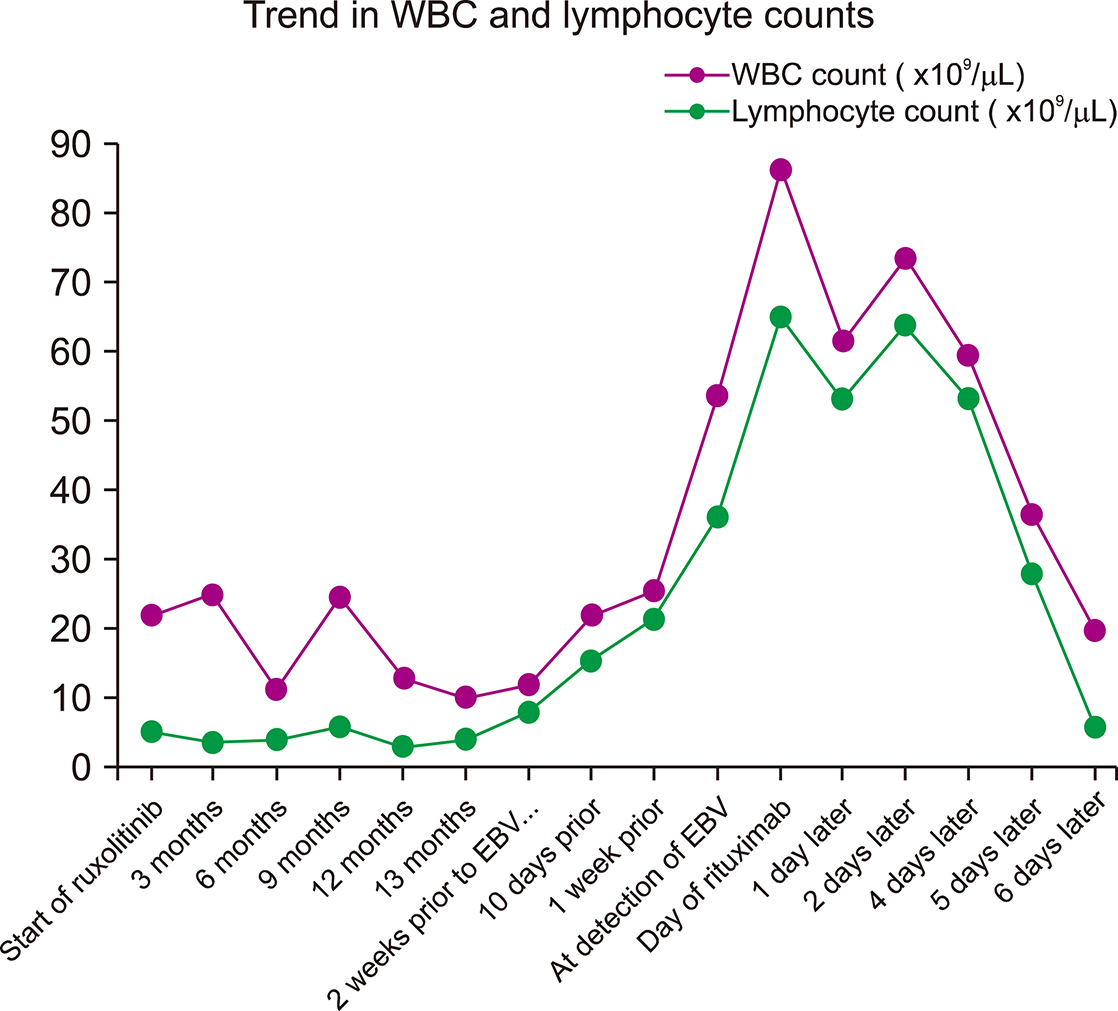
Figure
Reference
-
1. Verstovsek S, Mesa RA, Gotlib J, et al. Long-term treatment with ruxolitinib for patients with myelofibrosis: 5-year update from the randomized, double-blind, placebo-controlled, phase 3 COMFORT-I trial. J Hematol Oncol. 2017; 10:55.
Article2. Cervantes F, Vannucchi AM, Kiladjian JJ, et al. Three-year efficacy, safety, and survival findings from COMFORT-II, a phase 3 study comparing ruxolitinib with best available therapy for myelofibrosis. Blood. 2013; 122:4047–4053.
Article3. Caocci G, Murgia F, Podda L, Solinas A, Atzeni S, La Nasa G. Reactivation of hepatitis B virus infection following ruxolitinib treatment in a patient with myelofibrosis. Leukemia. 2014; 28:225–227.
Article4. Novartis Europharm Limited. Summary of product characteristics: Jaksvi, INN-ruxolitinib. Amsterdam, The Netherlands: European Medicines Agency;2017. Accesed October 31, 2018. at https://www.ema.europa.eu/en/documents/product-information/jakavi-epar-product-information_en.pdf.5. Pálmason R, Lindén O, Richter J. Case-report: EBV driven lymphoproliferative disorder associated with ruxolitinib. BMC Hematol. 2015; 15:10.
Article6. Kusano Y, Terui Y, Ueda K, Hatake K. Epstein-Barr virus gastric ulcer associated with ruxolitinib. Ann Hematol. 2016; 95:1741–1742.
Article7. O'Shea JJ, Holland SM, Staudt LM. JAKs and STATs in immunity, immunodeficiency, and cancer. N Engl J Med. 2013; 368:161–170.8. Massa M, Rosti V, Campanelli R, Fois G, Barosi G. Rapid and long-lasting decrease of T-regulatory cells in patients with myelofibrosis treated with ruxolitinib. Leukemia. 2014; 28:449–451.
Article9. Heine A, Held SA, Daecke SN, et al. The JAK-inhibitor ruxolitinib impairs dendritic cell function in vitro and in vivo. Blood. 2013; 122:1192–1202.
Article10. Parampalli Yajnanarayana S, Stübig T, Cornez I, et al. JAK1/2 inhibition impairs T cell function in vitro and in patients with myeloproliferative neoplasms. Br J Haematol. 2015; 169:824–833.
Article11. Schönberg K, Rudolph J, Vonnahme M, et al. JAK inhibition impairs NK cell function in myeloproliferative neoplasms. Cancer Res. 2015; 75:2187–2199.
Article12. Lussana F, Cattaneo M, Rambaldi A, Squizzato A. Ruxolitinib-associated infections: a systematic review and meta-analysis. Am J Hematol. 2018; 93:339–347.
Article13. Dioverti MV, Abu Saleh OM, Tande AJ. Infectious complications in patients on treatment with ruxolitinib: case report and review of the literature. Infect Dis (Lond). 2018; 50:381–387.
Article14. Sylvine P, Thomas S, Pirayeh E;. Infections associated with ruxolitinib: study in the French Pharmacovigilance database. Ann Hematol. 2018; 97:913–914.
Article15. Heine A, Brossart P, Wolf D. Ruxolitinib is a potent immunosuppressive compound: is it time for anti-infective prophylaxis? Blood. 2013; 122:3843–3844.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epstein Barr virus-associated lymphoproliferative diseases: the virus as a therapeutic target
- Ruxolitinib changes the natural course of myelofibrosis and its transplant outcome
- Real-life ruxolitinib experience in intermediate-risk myelofibrosis
- EBV-Associated Lymphoproliferative Disorders
- A Case of Severe Chronic Active Epstein-Barr Virus Infection with T-cell lymphoproliferative Disorder