Yonsei Med J.
2016 Jan;57(1):269-271. 10.3349/ymj.2016.57.1.269.
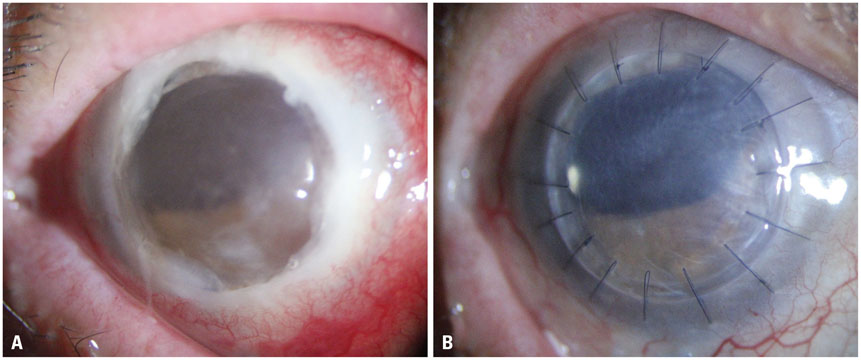
Tectonic Lamellar Keratoplasty Using Cryopreserved Cornea in a Large Descemetocele
- Affiliations
-
- 1Department of Ophthalmology, The Institute of Vision Research, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. tikim@yuhs.ac
- 2Corneal Dystrophy Research Institute, Severance Biomedical Science Institute, and Brain Korea 21 PLUS Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2466381
- DOI: http://doi.org/10.3349/ymj.2016.57.1.269
Abstract
- We describe herein a case of an impending corneal perforation with a large descemetocele in a patient with previous penetrating keratoplasty (PKP) that subsequently was treated with an emergent lamellar keratoplasty using frozen preserved cornea. A 76-year-old male patient, who had a PKP, presented with a completely whitish and edematous graft accompanied by large epithelial defects. Although antibiotics and antiviral agents were tried for three days, the corneal stroma abruptly melted, except for the Descemet's membrane and endothelium. Cryopreserved corneal tissue that was kept at -80degrees C was thawed and sutured on top of the remaining Descemet's membrane and endothelium. Pathological and microbiological tests were conducted using the remaining donor and recipient corneal tissues. After tectonic corneal transplantation on top of a large descemetocele, a healthy graft and relatively clear interfaces between graft-host junctions were maintained without serious adverse reactions throughout 6 month follow-up period. Microbiological evaluations of donor tissue at the time of thawing and tissue preparation were done, and the results were all negative. Tissue that was taken intraoperatively from the recipient cornea also showed negative microbiological results. In conclusion, tectonic lamellar keratoplasty, using cryopreserved corneal tissue, only onto the remaining Descemet's membrane and endothelium in an emergent condition, was a safe and effective treatment.
MeSH Terms
Figure
Reference
-
1. Krachmer JH, Mannis MJ, Holland EJ. Cornea. 2nd ed. Philadelphia: Elsevier Mosby;2005.2. Watson SL, Tuft SJ, Dart JK. Patterns of rejection after deep lamellar keratoplasty. Ophthalmology. 2006; 113:556–560.
Article3. Al-Torbak A, Malak M, Teichmann KD, Wagoner MD. Presumed stromal graft rejection after deep anterior lamellar keratoplasty. Cornea. 2005; 24:241–243.
Article4. Yao YF, Zhang YM, Zhou P, Zhang B, Qiu WY, Tseng SC. Therapeutic penetrating keratoplasty in severe fungal keratitis using cryopreserved donor corneas. Br J Ophthalmol. 2003; 87:543–547.
Article5. Chen W, Lin Y, Zhang X, Wang L, Liu M, Liu J, et al. Comparison of fresh corneal tissue versus glycerin-cryopreserved corneal tissue in deep anterior lamellar keratoplasty. Invest Ophthalmol Vis Sci. 2010; 51:775–781.
Article6. Javadi MA, Feizi S, Javadi F, Kanavi MR, Ghasemi H, Karimdizani S, et al. Deep anterior lamellar keratoplasty using fresh versus cryopreserved corneas. Ophthalmology. 2014; 121:610–611.
Article7. Li J, Yu L, Deng Z, Wang L, Sun L, Ma H, et al. Deep anterior lamellar keratoplasty using acellular corneal tissue for prevention of allograft rejection in high-risk corneas. Am J Ophthalmol. 2011; 152:762–770.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tectonic Deep Anterior Lamellar Keratoplasty in Impending Corneal Perforation Using Cryopreserved Cornea
- Clinical Evaluation of Full-thickness Deep Lamellar Keratoplasty
- C-type Anterior Lamellar Keratoplasty Using Cryopreserved Leftover Cornea for Terrien's Marginal Degeneration
- A Case of Tectonic Lamellar Corneal Patch Graft Using Acellular Cornea in Corneal Ulcer Perforation
- A tectonic keratoprosthesis using expanded polytetrafluoroethylene as a supporting skirt in humans