Yonsei Med J.
2016 Jan;57(1):81-87. 10.3349/ymj.2016.57.1.81.
The Beneficial Effect of Renin-Angiotensin-Aldosterone System Blockade in Marfan Syndrome Patients after Aortic Root Replacement
- Affiliations
-
- 1Cardiology Division, Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University Health System, Seoul, Korea. cdhlyj@yuhs.ac
- 2Department of Cardiovascular Surgery, Severance Cardiovascular Hospital, Yonsei University Health System, Seoul, Korea.
- 3Department of Radiology, Research Institute of Radiological Science, Yonsei University Health System, Seoul, Korea.
- 4Department of Anesthesiology and Pain Medicine, Severance Cardiovascular Hospital, Yonsei University Health System, Seoul, Korea.
- KMID: 2466355
- DOI: http://doi.org/10.3349/ymj.2016.57.1.81
Abstract
- PURPOSE
In this study, we evaluated the long term beneficial effect of Renin-Angiotensin-Aldosterone System (RAAS) blockade therapy in treatment of Marfan aortopathy.
MATERIALS AND METHODS
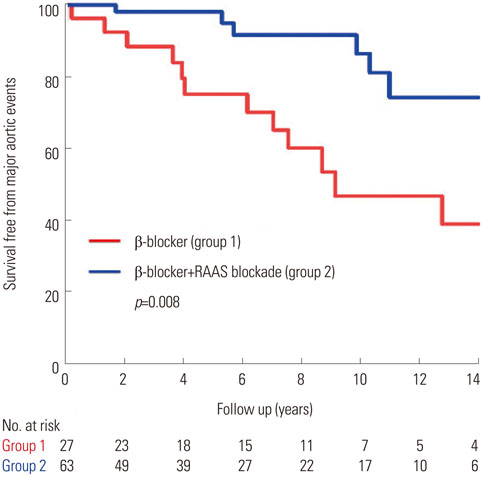
We reviewed Marfan syndrome (MFS) patients who underwent aortic root replacement (ARR) between January 1996 and January 2011. All patients were prescribed beta-blockers indefinitely. We compared major aortic events including mortality, aortic dissection, and reoperation in patients without RAAS blockade (group 1, n=27) to those with (group 2, n=63). The aortic growth rate was calculated by dividing the diameter change on CT scans taken immediately post-operatively and the latest scan available.
RESULTS
There were no differences in clinical parameters except for age which was higher in patients with RAAS blockade. In group 1, 2 (7%) deaths, 5 (19%) aortic dissections, and 7 (26%) reoperations occurred. In group 2, 3 (5%) deaths, 2 (3%) aortic dissections, and 3 (5%) reoperations occurred. A Kaplan-Meier plot demonstrated improved survival free from major aortic events in group 2. On multivariate Cox, RAAS blockade was an independent negative predictor of major aortic events (hazard ratio 0.38, 95% confidence interval 0.30-0.43, p=0.002). Mean diameter change in descending thoracic and supra-renal abdominal aorta was significantly higher in patients without RAAS blockade (p<0.05).
CONCLUSION
In MFS patients who underwent ARR, the addition of RAAS blockade to beta-blocker was associated with reduction of aortic dilatation and clinical events.
MeSH Terms
-
Adrenergic beta-Antagonists/pharmacology
Aged
Aneurysm, Dissecting/complications/mortality/surgery
*Angiotensin Receptor Antagonists
Angiotensin-Converting Enzyme Inhibitors/*therapeutic use
Aorta/pathology/*surgery
Aortic Aneurysm/complications/mortality/surgery
Aortic Valve
Female
Humans
Male
Marfan Syndrome/mortality/*surgery
Middle Aged
Renin-Angiotensin System/*drug effects
Adrenergic beta-Antagonists
Angiotensin Receptor Antagonists
Angiotensin-Converting Enzyme Inhibitors
Figure
Reference
-
1. Cañadas V, Vilacosta I, Bruna I, Fuster V. Marfan syndrome. Part 1: pathophysiology and diagnosis. Nat Rev Cardiol. 2010; 7:256–265.
Article2. Shin MS, Park HY, Lim Y, Shin GJ, Jang Y, Jang BC, et al. Identification of Molecular Defects in Korean Patients with Marfan Syndrome. Korean Circ J. 2003; 33:1018–1027.
Article3. Jondeau G, Michel JB, Boileau C. The translational science of Marfan syndrome. Heart. 2011; 97:1206–1214.
Article4. Sawaki D, Suzuki T. Targeting transforming growth factor-β signaling in aortopathies in Marfan syndrome. Circ J. 2013; 77:898–899.
Article5. Finkbohner R, Johnston D, Crawford ES, Coselli J, Milewicz DM. Marfan syndrome. Long-term survival and complications after aortic aneurysm repair. Circulation. 1995; 91:728–733.6. Judge DP, Dietz HC. Marfan's syndrome. Lancet. 2005; 366:1965–1976.
Article7. Loeys BL, Dietz HC, Braverman AC, Callewaert BL, De Backer J, Devereux RB, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet. 2010; 47:476–485.
Article8. Pyeritz RE. Marfan syndrome: current and future clinical and genetic management of cardiovascular manifestations. Semin Thorac Cardiovasc Surg. 1993; 5:11–16.9. Gott VL, Greene PS, Alejo DE, Cameron DE, Naftel DC, Miller DC, et al. Replacement of the aortic root in patients with Marfan's syndrome. N Engl J Med. 1999; 340:1307–1313.
Article10. Shores J, Berger KR, Murphy EA, Pyeritz RE. Progression of aortic dilatation and the benefit of long-term beta-adrenergic blockade in Marfan's syndrome. N Engl J Med. 1994; 330:1335–1341.
Article11. Volguina IV, Miller DC, LeMaire SA, Palmero LC, Wang XL, Connolly HM, et al. Valve-sparing and valve-replacing techniques for aortic root replacement in patients with Marfan syndrome: analysis of early outcome. J Thorac Cardiovasc Surg. 2009; 137:1124–1132.
Article12. Karck M, Kallenbach K, Hagl C, Rhein C, Leyh R, Haverich A. Aortic root surgery in Marfan syndrome: Comparison of aortic valve-sparing reimplantation versus composite grafting. J Thorac Cardiovasc Surg. 2004; 127:391–398.
Article13. de Oliveira NC, David TE, Ivanov J, Armstrong S, Eriksson MJ, Rakowski H, et al. Results of surgery for aortic root aneurysm in patients with Marfan syndrome. J Thorac Cardiovasc Surg. 2003; 125:789–796.
Article14. Habashi JP, Judge DP, Holm TM, Cohn RD, Loeys BL, Cooper TK, et al. Losartan, an AT1 antagonist, prevents aortic aneurysm in a mouse model of Marfan syndrome. Science. 2006; 312:117–121.
Article15. Brooke BS, Habashi JP, Judge DP, Patel N, Loeys B, Dietz HC 3rd. Angiotensin II blockade and aortic-root dilation in Marfan's syndrome. N Engl J Med. 2008; 358:2787–2795.
Article16. Yetman AT, Bornemeier RA, McCrindle BW. Usefulness of enalapril versus propranolol or atenolol for prevention of aortic dilation in patients with the Marfan syndrome. Am J Cardiol. 2005; 95:1125–1127.
Article17. Groenink M, den Hartog AW, Franken R, Radonic T, de Waard V, Timmermans J, et al. Losartan reduces aortic dilatation rate in adults with Marfan syndrome: a randomized controlled trial. Eur Heart J. 2013; 34:3491–3500.
Article18. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971; 285:1441–1446.
Article19. Geisbuesch S, Schray D, Bischoff MS, Lin HM, Di Luozzo G, Griepp RB. Frequency of reoperations in patients with Marfan syndrome. Ann Thorac Surg. 2012; 93:1496–1501.
Article20. Gott VL, Cameron DE, Alejo DE, Greene PS, Shake JG, Caparrelli DJ, et al. Aortic root replacement in 271 Marfan patients: a 24-year experience. Ann Thorac Surg. 2002; 73:438–443.21. Nienaber CA, Von Kodolitsch Y. Therapeutic management of patients with Marfan syndrome: focus on cardiovascular involvement. Cardiol Rev. 1999; 7:332–341.22. Ades L; CSANZ Cardiovascular Genetics Working Group. Guidelines for the diagnosis and management of Marfan syndrome. Heart Lung Circ. 2007; 16:28–30.
Article23. Habashi JP, Doyle JJ, Holm TM, Aziz H, Schoenhoff F, Bedja D, et al. Angiotensin II type 2 receptor signaling attenuates aortic aneurysm in mice through ERK antagonism. Science. 2011; 332:361–365.
Article24. Nagashima H, Sakomura Y, Aoka Y, Uto K, Kameyama Ki, Ogawa M, et al. Angiotensin II type 2 receptor mediates vascular smooth muscle cell apoptosis in cystic medial degeneration associated with Marfan's syndrome. Circulation. 2001; 104:I282–I287.
Article25. Moltzer E, te Riet L, Swagemakers SM, van Heijningen PM, Vermeij M, van Veghel R, et al. Impaired vascular contractility and aortic wall degeneration in fibulin-4 deficient mice: effect of angiotensin II type 1 (AT1) receptor blockade. PLoS One. 2011; 6:e23411.
Article26. Iida Y, Xu B, Schultz GM, Chow V, White JJ, Sulaimon S, et al. Efficacy and mechanism of angiotensin II receptor blocker treatment in experimental abdominal aortic aneurysms. PLoS One. 2012; 7:e49642.
Article27. Adams JN, Brooks M, Redpath TW, Smith FW, Dean J, Gray J, et al. Aortic distensibility and stiffness index measured by magnetic resonance imaging in patients with Marfan's syndrome. Br Heart J. 1995; 73:265–269.
Article28. Segers P, De Backer J, Devos D, Rabben SI, Gillebert TC, Van Bortel LM, et al. Aortic reflection coefficients and their association with global indexes of wave reflection in healthy controls and patients with Marfan's syndrome. Am J Physiol Heart Circ Physiol. 2006; 290:H2385–H2392.
Article29. Nollen GJ, Groenink M, Tijssen JG, Van Der Wall EE, Mulder BJ. Aortic stiffness and diameter predict progressive aortic dilatation in patients with Marfan syndrome. Eur Heart J. 2004; 25:1146–1152.
Article30. Groenink M, de Roos A, Mulder BJ, Verbeeten B Jr, Timmermans J, Zwinderman AH, et al. Biophysical properties of the normal-sized aorta in patients with Marfan syndrome: evaluation with MR flow mapping. Radiology. 2001; 219:535–540.
Article31. Groenink M, Langerak SE, Vanbavel E, van der Wall EE, Mulder BJ, van der Wal AC, et al. The influence of aging and aortic stiffness on permanent dilation and breaking stress of the thoracic descending aorta. Cardiovasc Res. 1999; 43:471–480.
Article32. Dhakam Z, McEniery CM, Yasmin , Cockcroft JR, Brown MJ, Wilkinson IB. Atenolol and eprosartan: differential effects on central blood pressure and aortic pulse wave velocity. Am J Hypertens. 2006; 19:214–219.
Article33. Mackenzie IS, McEniery CM, Dhakam Z, Brown MJ, Cockcroft JR, Wilkinson IB. Comparison of the effects of antihypertensive agents on central blood pressure and arterial stiffness in isolated systolic hypertension. Hypertension. 2009; 54:409–413.
Article34. Takami T, Shigemasa M. Efficacy of various antihypertensive agents as evaluated by indices of vascular stiffness in elderly hypertensive patients. Hypertens Res. 2003; 26:609–614.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Renin-Angiotensin-Aldosterone System Blockade and Renal Protection in Diabetic Nephropathy
- A Case of Infantile Marfan Syndrome
- Aortic Root Replacement with Valve Preservation in a Patient with Annuloaortic Ectasia
- New drugs for treatment of hypertension
- A Case of Marfan Syndrome in Pregnancy with Aortic Root Dilatation