Korean J Radiol.
2016 Dec;17(6):874-881. 10.3348/kjr.2016.17.6.874.
Predictors for Better Blood-Flow Restoration of Long-Segmental Below-the-Knee Chronic Total Occlusions after Endovascular Therapy in Diabetic Patients
- Affiliations
-
- 1Department of Radiology, Chonnam National University Medical School, Gwangju 501757, Korea.
- 2Department of Radiology, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai 200233, China. zhaojungongradio@hotmail.com
- 3Department of Endocrinology, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai 200233, China.
- KMID: 2466284
- DOI: http://doi.org/10.3348/kjr.2016.17.6.874
Abstract
OBJECTIVE
To prospectively investigate predictors for good restoration of blood flow of below-the-knee (BTK) chronic total occlusions (CTOs) after endovascular therapy in diabetes mellitus (DM) patients.
MATERIALS AND METHODS
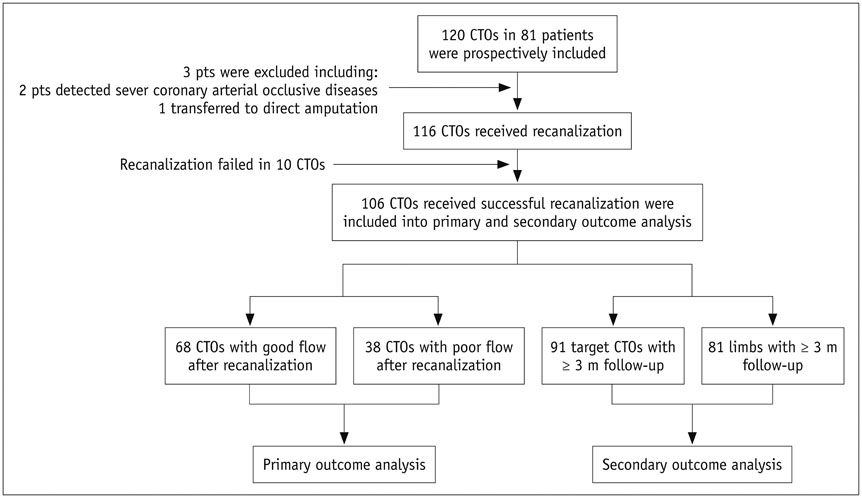
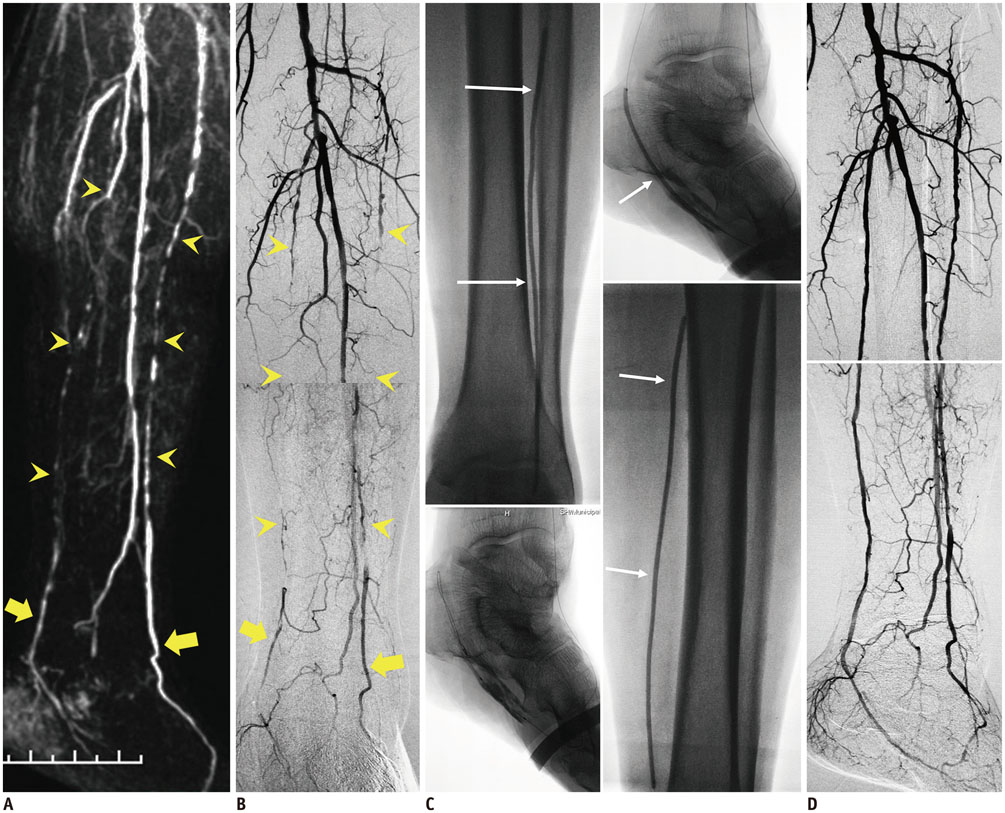
A total of 120 long-segmental (≥ 5 cm) BTK, CTOs in 81 patients who underwent recanalization were included in this study. After angioplasty, blood-flow restoration was assessed using modified thrombolysis in myocardial ischemia grades and classified as good flow (grade 3) and poor flow (grade 1/2). One hundred and six CTOs with successful recanalization were divided into a good flow group (GFG; n = 68) and poor flow group (PFG; n = 38). Multivariate logistic regression analyses were undertaken to determine independent predictors of blood-flow restoration. Receiver operating characteristic curves were constructed to determine the best cutoff value. The prevalence of target-lesion restenosis during follow-up was compared between two groups.
RESULTS
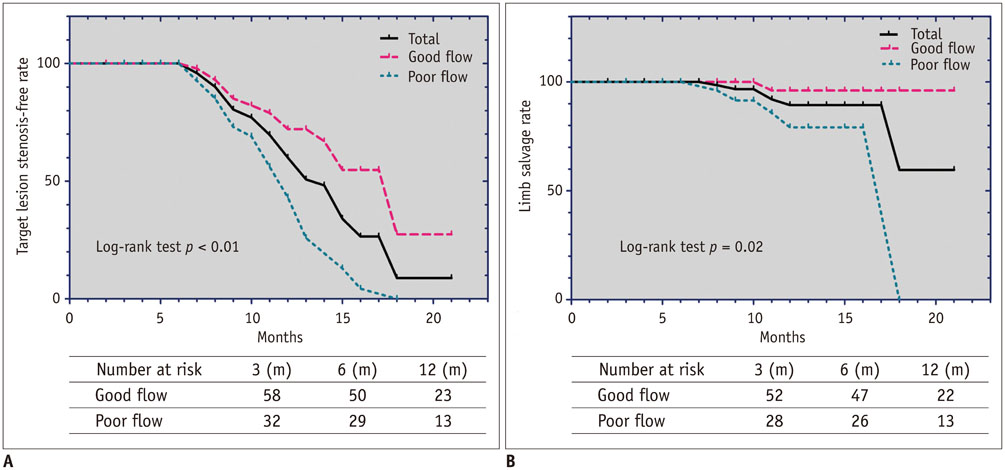
Univariate analyses suggested that CTOs in GFG were characterized by lighter limb ischemia (p = 0.03), shorter course of ischemic symptoms (p < 0.01) and lesion length (p = 0.04), more frequent use of intraluminal angioplasty (p = 0.03), and higher runoff score (p < 0.01) than those in PFG. Multivariate regression analyses suggested that distal runoffs (p = 0.001; odds ratio [OR], 10.32; 95% confidence interval [CI]: 4.082-26.071) and lesion length (p < 0.001; OR, 1.26; 95% CI: 1.091-1.449) were independent predictors for good flow restoration. Kaplan-Meier analyses at 12 months showed a higher prevalence of non-restenosis in GFG (p < 0.01).
CONCLUSION
Distal runoffs and lesion length are independent predictors for good flow restoration for long-segmental BTK, CTOs in DM patients who receive endovascular therapy.
Keyword
MeSH Terms
-
Aged
Area Under Curve
Arterial Occlusive Diseases/complications/diagnostic imaging/physiopathology/*therapy
Blood Flow Velocity/*physiology
Chronic Disease
Diabetes Mellitus, Type 2/*complications
Female
Femoral Artery/diagnostic imaging
Humans
Kaplan-Meier Estimate
Knee Joint/*blood supply
Limb Salvage
Logistic Models
Magnetic Resonance Angiography
Male
Middle Aged
Odds Ratio
Predictive Value of Tests
ROC Curve
Regional Blood Flow/physiology
Retrospective Studies
Treatment Outcome
Figure
Reference
-
1. Liistro F, Porto I, Angioli P, Grotti S, Ricci L, Ducci K, et al. Drug-eluting balloon in peripheral intervention for below the knee angioplasty evaluation (DEBATE-BTK): a randomized trial in diabetic patients with critical limb ischemia. Circulation. 2013; 128:615–621.2. Baumann F, Engelberger RP, Willenberg T, Do DD, Kalka C, Baumgartner I, et al. Infrapopliteal lesion morphology in patients with critical limb ischemia: implications for the development of anti-restenosis technologies. J Endovasc Ther. 2013; 20:149–156.3. Thukkani AK, Kinlay S. Endovascular intervention for peripheral artery disease. Circ Res. 2015; 116:1599–1613.4. Cassese S, Ndrepepa G, Liistro F, Fanelli F, Kufner S, Ott I, et al. Drug-coatedballoons for revascularization of infrapopliteal arteries: a meta-analysis of randomized trials. JACC Cardiovasc Interv. 2016; 9:1072–1080.5. Faglia E, Mantero M, Caminiti M, Caravaggi C, De Giglio R, Pritelli C, et al. Extensive use of peripheral angioplasty, particularly infrapopliteal, in the treatment of ischaemic diabetic foot ulcers: clinical results of a multicentric study of 221 consecutive diabetic subjects. J Intern Med. 2002; 252:225–232.6. Sidhu R, Pigott J, Pigott M, Comerota A. Subintimal angioplasty for advanced lower extremity ischemia due to TASC II C and D lesions of the superficial femoral artery. Vasc Endovascular Surg. 2010; 44:633–637.7. Hendricks NJ, Sabri SS. Subintimal arterial flossing with antegrade-retrograde intervention (SAFARI) and rertograde access for critical limb ischemia. Tech Vasc Interv Radiol. 2014; 17:203–210.8. Kim YH, Bae JI, Jeon YS, Kim CW, Jae HJ, Park KB, et al. Korean guidelines for interventional recanalization of lower extremity arteries. Korean J Radiol. 2015; 16:696–722.9. Conrad MF, Kang J, Cambria RP, Brewster DC, Watkins MT, Kwolek CJ, et al. Infrapopliteal balloon angioplasty for the treatment of chronic occlusive disease. J Vasc Surg. 2009; 50:799–805.e4.10. Saqib NU, Domenick N, Cho JS, Marone L, Leers S, Makaroun MS, et al. Predictors and outcomes of restenosis following tibial artery endovascular interventions for critical limb ischemia. J Vasc Surg. 2013; 57:692–699.11. Sacks D, Marinelli DL, Martin LG, Spies JB. Society of Interventional Radiology Technology Assessment Committee. Reporting standards for clinical evaluation of new peripheral arterial revascularization devices. J Vasc Interv Radiol. 2003; 14(9 Pt 2):S395–S404.12. Iida O, Soga Y, Hirano K, Kawasaki D, Suzuki K, Miyashita Y, et al. Long-term results of direct and indirect endovascular revascularization based on the angiosome concept in patients with critical limb ischemia presenting with isolated below-the-knee lesions. J Vasc Surg. 2012; 55:363–370.e5.13. Schlager O, Francesconi M, Haumer M, Dick P, Sabeti S, Amighi J, et al. Duplex sonography versus angiography for assessment of femoropopliteal arterial disease in a "real-world" setting. J Endovasc Ther. 2007; 14:452–459.14. Hiramori S, Soga Y, Tomoi Y, Tosaka A. Impact of runoff grade after endovascular therapy for femoropopliteal lesions. J Vasc Surg. 2014; 59:720–727.15. Kiguchi MM, Marone LK, Chaer RA, Winger DG, Shi ZY, Celis RI, et al. Patterns of femoropopliteal recurrence after routine and selective stenting endoluminal therapy. J Vasc Surg. 2013; 57:37–43.16. Conrad MF, Crawford RS, Hackney LA, Paruchuri V, Abularrage CJ, Patel VI, et al. Endovascular management of patients with critical limb ischemia. J Vasc Surg. 2011; 53:1020–1025.17. Zhu YQ, Zhao JG, Li MH, Liu F, Wang JB, Cheng YS, et al. Retrograde transdorsal-to-plantar or transplantar-to-dorsal intraluminal re-entry following unsuccessful subintimal angioplasty for below-the-ankle arterial occlusion. J Endovasc Ther. 2010; 17:712–721.18. Palena LM, Manzi M. Extreme below-the-knee interventions: retrograde transmetatarsal or transplantar arch access for foot salvage in challenging cases of critical limb ischemia. J Endovasc Ther. 2012; 19:805–811.19. Rana MA, Gloviczki P. Endovascular interventions for infrapopliteal arterial disease: an update. Semin Vasc Surg. 2012; 25:29–34.20. Malcolm PN, King DH, Crabbe RW, Taylor PR, Reidy JF. Arteriovenous fistula at the site of balloon dilatation complicating femoropopliteal angioplasty. Cardiovasc Intervent Radiol. 1997; 20:54–56.21. Ferraresi R, Centola M, Ferlini M, Da Ros R, Caravaggi C, Assaloni R, et al. Long-term outcomes after angioplasty of isolated, below-the-knee arteries in diabetic patients with critical limb ischaemia. Eur J Vasc Endovasc Surg. 2009; 37:336–342.22. Park SW, Kim JS, Yun IJ, Hwang JJ, Lee SA, Chee HK, et al. Clinical outcomes of endovascular treatments for critical limb ischemia with chronic total occlusive lesions limited to below-the-knee arteries. Acta Radiol. 2013; 54:785–789.23. Spillerova K, Biancari F, Leppäniemi A, Albäck A, Söderström M, Venermo M. Differential impact of bypass surgery and angioplasty on angiosome-targeted infrapopliteal revascularization. Eur J Vasc Endovasc Surg. 2015; 49:412–419.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Treatment for Chronic Total Occlusions of Peripheral Arteries
- Macular Blood Flows in Diabetic Patients
- The Outback(R) LTDtrade mark Catheter: The Novel Re-Entry Technique in Recanalization of Chronic Inflow Occlusion of the Superficial Femoral Arteries in 3 Cases
- Drug-eluting Stent Implantation for a Below-the-knee Chronic Total Occlusion Lesion: A Case Report
- Current Role of Endovascular Therapy in Leg Arteries