J Adv Prosthodont.
2019 Dec;11(6):341-349. 10.4047/jap.2019.11.6.341.
Effects of cementless fixation of implant prosthesis: A finite element study
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry, Pusan National University, Yangsan, Republic of Korea.
- 2School of Mechanical Engineering, Kyungpook National University, Daegu, Republic of Korea. gunwoo@knu.ac.kr
- 3Department of Prosthodontics, School of Dentistry, Kyung Hee University, Seoul, Republic of Korea.
- KMID: 2466249
- DOI: http://doi.org/10.4047/jap.2019.11.6.341
Abstract
- PURPOSE
A novel retentive type of implant prosthesis that does not require the use of cement or screw holes has been introduced; however, there are few reports examining the biomechanical aspects of this novel implant. This study aimed to evaluate the biomechanical features of cementless fixation (CLF) implant prostheses.
MATERIALS AND METHODS
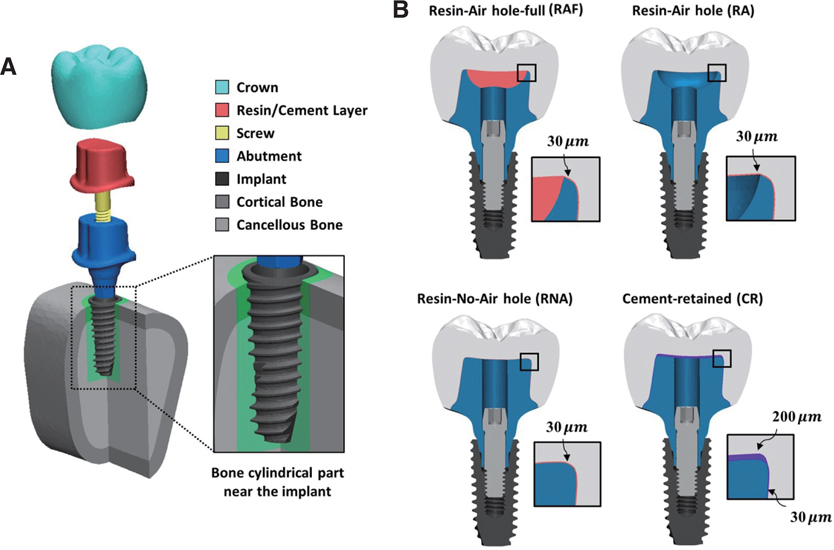
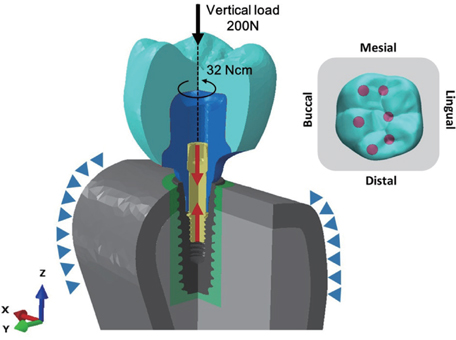
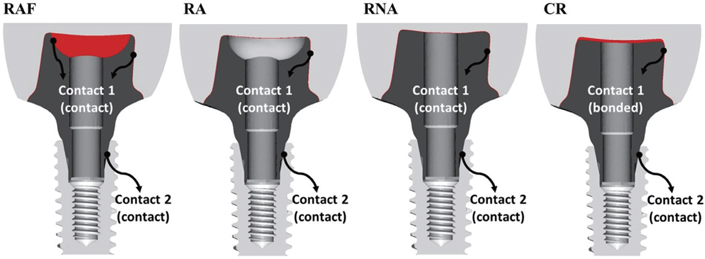
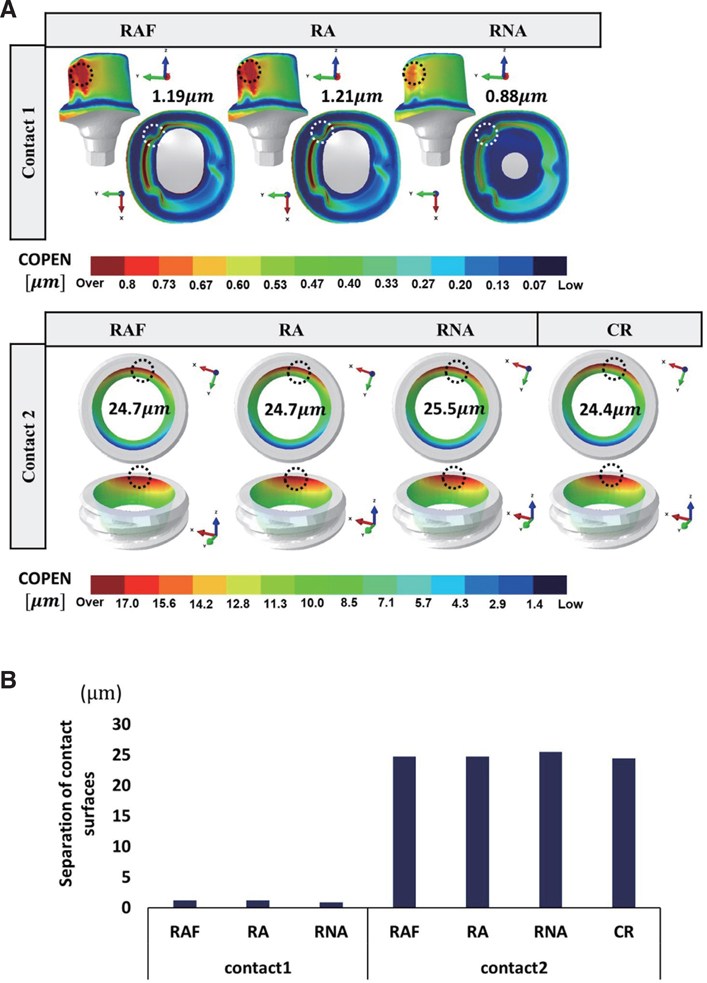
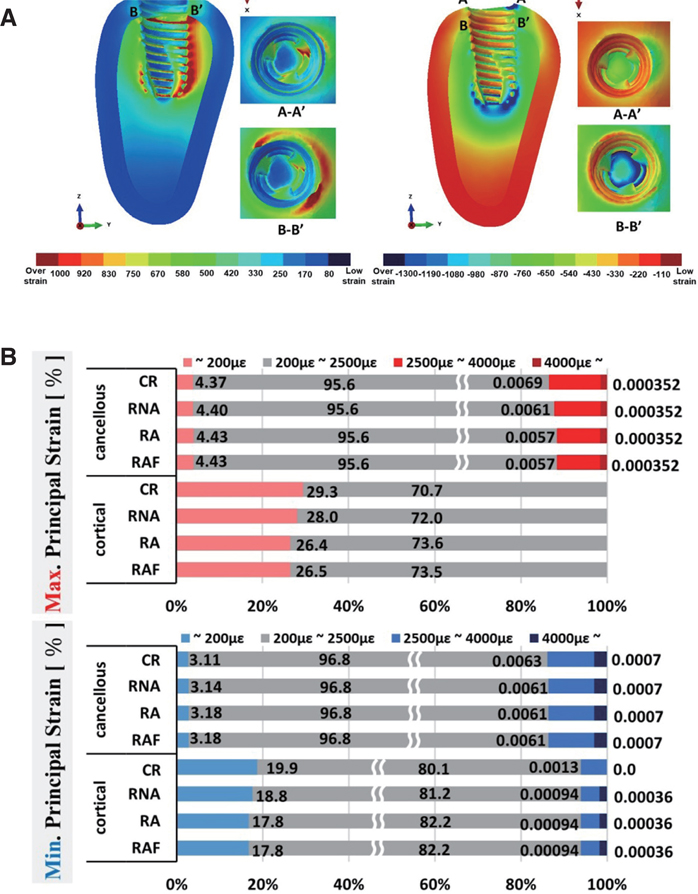
The test groups of three variations of CLF implant prostheses and a control group of conventional cement-retained (CR) prosthesis were designed three-dimensionally for finite element analysis. The test groups were divided according to the abutment shape and the relining strategy on the inner surface of the implant crown as follows; resin-air hole-full (RAF), resin-air hole (RA), and resin-no air hole (RNA). The von Mises stress and principal stress were used to evaluate the stress values and distributions of the implant components. Contact open values were calculated to analyze the gap formation of the contact surfaces at the abutment-resin and abutment-implant interfaces. The micro-strain values were evaluated for the surrounding bone.
RESULTS
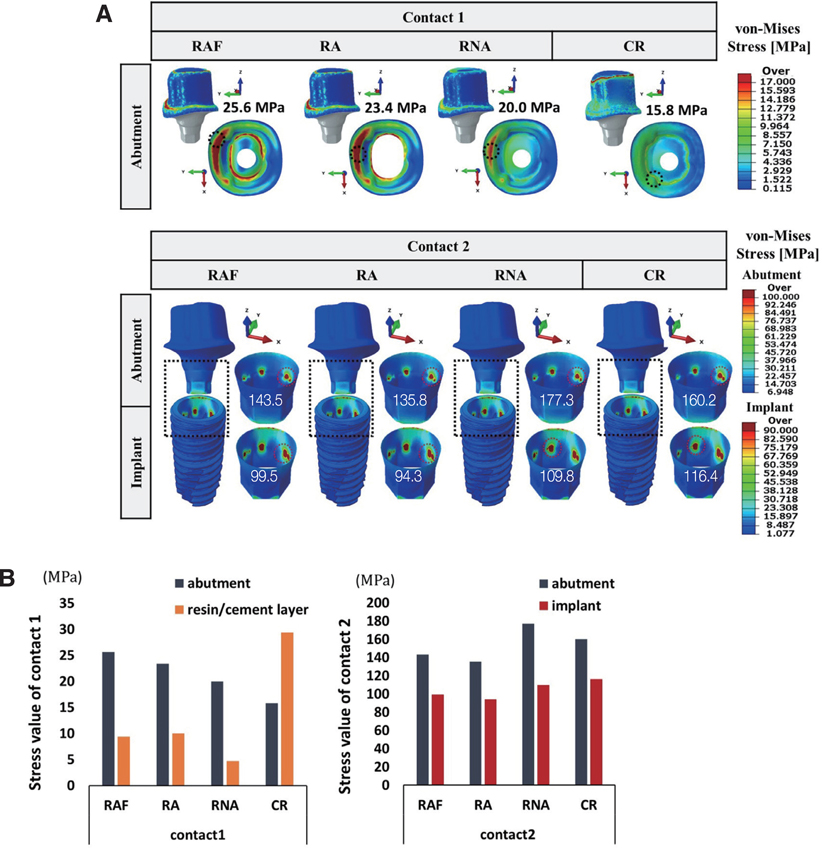
Values reflecting the maximum stress on the abutment were as follows (in MPa): RAF, 25.6; RA, 23.4; RNA, 20.0; and CR, 15.8. The value of gap formation was measured from 0.88 to 1.19 µm at the abutmentresin interface and 24.4 to 24.7 µm at the abutment-implant interface. The strain distribution was similar in all cases.
CONCLUSION
CLF had no disadvantages in terms of the biomechanical features compared with conventional CR implant prosthesis and could be successfully applied for implant prosthesis.
Figure
Reference
-
1. Muddugangadhar BC, Amarnath GS, Sonika R, Chheda PS, Garg A. Meta-analysis of failure and survival rate of implant-supported single crowns, fixed partial denture, and implant tooth-supported prostheses. J Int Oral Health. 2015; 7:11–17.2. Simonis P, Dufour T, Tenenbaum H. Long-term implant survival and success: a 10-16-year follow-up of non-submerged dental implants. Clin Oral Implants Res. 2010; 21:772–777.3. Staubli N, Walter C, Schmidt JC, Weiger R, Zitzmann NU. Excess cement and the risk of peri-implant disease - a systematic review. Clin Oral Implants Res. 2017; 28:1278–1290.4. Wittneben JG, Millen C, Brägger U. Clinical performance of screw- versus cement-retained fixed implant-supported reconstructions-a systematic review. Int J Oral Maxillofac Implants. 2014; 29:84–98.5. Wittneben JG, Joda T, Weber HP, Brägger U. Screw retained vs. cement retained implant-supported fixed dental prosthesis. Periodontol 2000. 2017; 73:141–151.6. Amorfini L, Storelli S, Mosca D, Scanferla M, Romeo E. Comparison of cemented vs screw-retained, customized computer-aided design/computer-assisted manufacture zirconia abutments for esthetically located single-tooth implants: A 10-year randomized prospective study. Int J Prosthodont. 2018; 31:359–366.7. Lemos CA, de Souza Batista VE, Almeida DA, Santiago Júnior JF, Verri FR, Pellizzer EP. Evaluation of cement-retained versus screw-retained implant-supported restorations for marginal bone loss: A systematic review and meta-analysis. J Prosthet Dent. 2016; 115:419–427.8. Lee JI, Lee Y, Kim NY, Kim YL, Cho HW. A photoelastic stress analysis of screw- and cement-retained implant prostheses with marginal gaps. Clin Implant Dent Relat Res. 2013; 15:735–749.9. Cicciu M, Bramanti E, Matacena G, Guglielmino E, Risitano G. FEM evaluation of cemented-retained versus screw-retained dental implant single-tooth crown prosthesis. Int J Clin Exp Med. 2014; 7:817–825.10. Tanimura R, Suzuki S. Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study. Int J Implant Dent. 2017; 3:19.11. Hebel KS, Gajjar RC. Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent. 1997; 77:28–35.12. Taylor RC, Ghoneim AS, McGlumphy EA. An esthetic technique to fill screw-retained fixed prostheses. J Oral Implantol. 2004; 30:384–385.13. Weininger B, McGlumphy E, Beck M. Esthetic evaluation of materials used to fill access holes of screw-retained implant crowns. J Oral Implantol. 2008; 34:145–149.14. Sancho-Puchades M, Crameri D, Özcan M, Sailer I, Jung RE, Hämmerle CHF, Thoma DS. The influence of the emergence profile on the amount of undetected cement excess after delivery of cement-retained implant reconstructions. Clin Oral Implants Res. 2017; 28:1515–1522.15. Gehrke P, Bleuel K, Fischer C, Sader R. Influence of margin location and luting material on the amount of undetected cement excess on CAD/CAM implant abutments and cement-retained zirconia crowns: an in-vitro study. BMC Oral Health. 2019; 19:111.16. Ma S, Fenton A. Screw- versus cement-retained implant prostheses: a systematic review of prosthodontic maintenance and complications. Int J Prosthodont. 2015; 28:127–145.17. Papakostas GI, McGrath P, Stewart J, Charles D, Chen Y, Mischoulon D, Dording C, Fava M. Psychic and somatic anxiety symptoms as predictors of response to fluoxetine in major depressive disorder. Psychiatry Res. 2008; 161:116–120.18. Vaillancourt H, Pilliar RM, McCammond D. Finite element analysis of crestal bone loss around porous-coated dental implants. J Appl Biomater. 1995; 6:267–282.19. Bulaqi HA, Mousavi Mashhadi M, Safari H, Samandari MM, Geramipanah F. Effect of increased crown height on stress distribution in short dental implant components and their surrounding bone: A finite element analysis. J Prosthet Dent. 2015; 113:548–557.20. Niinomi M. Mechanical properties of biomedical titanium alloys. Mater Sci Eng. 1998; 243:231–236.21. Sertgöz A. Finite element analysis study of the effect of superstructure material on stress distribution in an implant-supported fixed prosthesis. Int J Prosthodont. 1997; 10:19–27.22. Tolidis K, Papadogiannis D, Papadogiannis Y, Gerasimou P. Dynamic and static mechanical analysis of resin luting cements. J Mech Behav Biomed Mater. 2012; 6:1–8.23. Lang LA, Kang B, Wang RF, Lang BR. Finite element analysis to determine implant preload. J Prosthet Dent. 2003; 90:539–546.24. Guda T, Ross TA, Lang LA, Millwater HR. Probabilistic analysis of preload in the abutment screw of a dental implant complex. J Prosthet Dent. 2008; 100:183–193.25. Wang RF, Kang B, Lang LA, Razzoog ME. The dynamic natures of implant loading. J Prosthet Dent. 2009; 101:359–371.26. Silva GC, Cornacchia TM, de Magalhães CS, Bueno AC, Moreira AN. Biomechanical evaluation of screw- and cement-retained implant-supported prostheses: a nonlinear finite element analysis. J Prosthet Dent. 2014; 112:1479–1488.27. Lee H, Park S, Noh G. Biomechanical analysis of 4 types of short dental implants in a resorbed mandible. J Prosthet Dent. 2019; 121:659–670.28. Roberts WE, Sarandeep H, Jeffery AR. Bone modeling: biomechanics, molecular mechanisms, and clinical perspectives. Semin Orthod. 2004; 10:123–161.29. Torcato LB, Pellizzer EP, Verri FR, Falcón-Antenucci RM, Santiago Júnior JF, de Faria Almeida DA. Influence of parafunctional loading and prosthetic connection on stress distribution: a 3D finite element analysis. J Prosthet Dent. 2015; 114:644–651.30. Santiago Junior JF, Verri FR, Almeida DA, de Souza Batista VE, Lemos CA, Pellizzer EP. Finite element analysis on influence of implant surface treatments, connection and bone types. Mater Sci Eng C Mater Biol Appl. 2016; 63:292–300.31. Ramos Verri F, Santiago Junior JF, de Faria Almeida DA, de Oliveira GB, de Souza Batista VE, Marques Honório H, Noritomi PY, Pellizzer EP. Biomechanical influence of crown-to-implant ratio on stress distribution over internal hexagon short implant: 3-D finite element analysis with statistical test. J Biomech. 2015; 48:138–145.32. Minatel L, Verri FR, Kudo GAH, de Faria Almeida DA, de Souza Batista VE, Lemos CAA, Pellizzer EP, Santiago JF Junior. Effect of different types of prosthetic platforms on stress-distribution in dental implant-supported prostheses. Mater Sci Eng C Mater Biol Appl. 2017; 71:35–42.33. He Y, Fok A, Aparicio C, Teng W. Contact analysis of gap formation at dental implant-abutment interface under oblique loading: A numerical-experimental study. Clin Implant Dent Relat Res. 2019; 21:741–752.34. Robinson D, Aguilar L, Gatti A, Abduo J, Lee PVS, Ackland D. Load response of the natural tooth and dental implant: A comparative biomechanics study. J Adv Prosthodont. 2019; 11:169–178.35. Mahnama A, Tafazzoli-Shadpour M, Geramipanah F, Mehdi Dehghan M. Verification of the mechanostat theory in mandible remodeling after tooth extraction: animal study and numerical modeling. J Mech Behav Biomed Mater. 2013; 20:354–362.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ANALYSIS OF THE FIT IN THE IMPLANT PROSTHESIS USING LASER DISPLACEMENT METER AND THREE-DIMENSIONAL FINITE ELEMENT METHOD
- A study on the various implant systems using the finite element stress analysis
- A finite element analysis on the 3-unit fixed prosthesis supported with a natural tooth and angle variable implant
- Three-dimensional finite element analysis of the splinted implant prosthesis in a reconstructed mandible
- Three-dimensional finite element analysis according to the insertion depth of an immediately loaded implant in the anterior maxilla