Korean J Adult Nurs.
2019 Dec;31(6):628-637. 10.7475/kjan.2019.31.6.628.
Factors Influencing Pre-Diabetes in Middle-aged Women based on the KNHANES
- Affiliations
-
- 1Assistant Professor, College of Nursing, Kyungdong University, Wonju, Korea.
- 2Assistant Professor, Department of Nursing, Dongguk University, Gyeongju, Korea. jrshim@dongguk.ac.kr
- KMID: 2466229
- DOI: http://doi.org/10.7475/kjan.2019.31.6.628
Abstract
- PURPOSE
This study was conducted to identify the predictive factors for pre-diabetes in middle-aged Korean women based on the Korean National Health and Nutrition Examination Survey (KNHANES).
METHODS
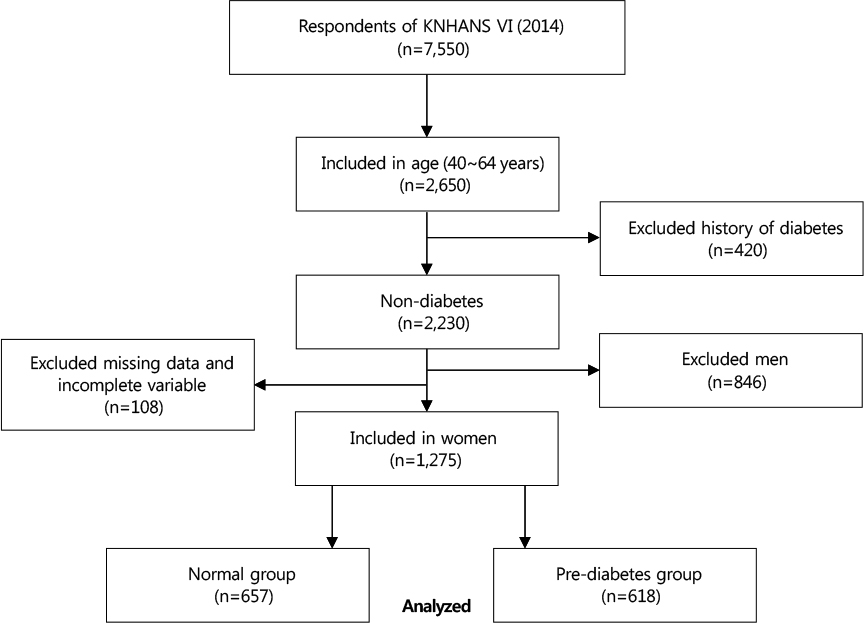
In this cross-sectional study, data were extracted from the second year of the 6th KNHANES (2013~2015), conducted at 129 sites from January to December 2014. The 1,275 subjects were middle-aged women between 40 and 64 years of age characterized as "pre-diabetic" (n=618) or "normal" (n=657) according to the American Diabetes Association (ADA) standard. Multivariate binary logistic regression was used to determine factors influencing pre-diabetes in middle-aged women.
RESULTS
The significant factors for pre-diabetes were a Waist-to-Height Ratio (WHtR) > 0.53 (Odds Ratio [OR]=1.71, 95% Confidence Interval [CI]=1.27~2.29), increasing prevalence of hypercholesterolemia (OR=2.02, 95% CI=1.42~2.86), and low level of High-Density Lipoprotein (HDL) cholesterol (OR=1.89, 95% CI=1.18~3.02). In addition, as age increased after 50 years, the proportion of WHtR > 0.53 decreased in the normal group, but increased with age in the pre-diabetes group.
CONCLUSION
Education to raise awareness about diabetes including pre-diabetes is needed for effective management of hyperlipidemia and central obesity to ensure a healthy middle age.
MeSH Terms
Figure
Reference
-
1. American Diabetes Association. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care. 2018; 41(Suppl 1):S13–S27. DOI: 10.2337/dc18-S002.2. Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012; 379(9833):2279–2290. DOI: 10.1016/S0140-6736(12)60283-9.
Article3. Huang Y, Cai X, Mai W, Li M, Hu Y. Association between prediabetes and risk of cardiovascular disease and all causes mortality: systematic review and meta-analysis. BMJ. 2016; 355:i5953. DOI: 10.1136/bmj.i5953.4. DeJesus RS, Breitkopf CR, Rutten LJ, Jacobson DJ, Wilson PM, Sauver JS. Incidence rate of prediabetes progression to diabetes: modeling an optimum target group for intervention. Population Health Management. 2017; 20(3):216–223. DOI: 10.1089/pop.2016.0067.
Article5. Luo B, Zhang J, Hu Z, Gao F, Zhou Q, Song S, et al. Diabetes-related behaviours among elderly people with pre-diabetes in rural communities of Hunan, China: a cross-sectional study. BMJ open. 2018; 8(1):e015747.6. Kim KE, Hwang SY. Impact of physical activity, central obesity and depression on the quality of life according to the presence of cardiovascular risk among menopausal middle-aged women: Secondary data analysis. Korean Journal of Adult Nursing. 2017; 29(4):382–392.
Article7. Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocrine Reviews. 2016; 37(3):278–316. DOI: 10.1210/er.2015-1137.
Article8. Hamilton MT, Hamilton DG, Zderic TW. Sedentary behavior as a mediator of type 2 diabetes. Medicine and Sport Science. 2014; 60:11–26. DOI: 10.1159/000357332.
Article9. Bhowmik B, Siddiquee T, Mujumder A, Afsana F, Ahmed T, Mdala I, et al. Serum lipid profile and its association with diabetes and prediabetes in a rural Bangladeshi population. International Journal of Environmental Research and Public Health. 2018; 15(9):1944. DOI: 10.3390/ijerph15091944.
Article10. Okwechime IO, Roberson S, Odoi A. Prevalence and predictors of pre-diabetes and diabetes amongadults 18 years or older in Florida: a multinomial logistic modeling approach. Plos One. 2015; 10(12):e0145781. DOI: 10.1371/journal.pone.0145781.11. Hilawe EH, Chiang C, Yatsuya H, Wang C, Ikerdeu E, Honjo K, et al. Prevalence and predictors of prediabetes and diabetes among adults in Palau: population-based national STEPS survey. Nagoya Journal of Medical Science. 2016; 78(4):475–483. DOI: 10.18999/nagjms.78.4.475.12. Song HJ, Lee EK, Kwon JW. Gender differences in the impact of obesity on health-related quality of life. Asia Pacific Journal of Public Health. 2016; 28(2):146–156. DOI: 10.1177/1010539515626267.
Article13. Worrall-Carter L, Ski C, Scruth E, Campbell M, Page K. Systematic review of cardiovascular disease in women: assessing the risk. Nursing & Health Sciences. 2011; 13(4):529–535. DOI: 10.1111/j.1442-2018.2011.00645.x.
Article14. Dosi R, Bhatt N, Shah P, Patell R. Cardiovascular disease and menopause. Journal of Clinical and Diagnostic Research. 2014; 8(2):62–64. DOI: 10.7860/jcdr/2014/6457.4009.15. Shin HM, Jee SH, Kim JH, Kim MR. The influence on cardiovascular mortality of the metabolic syndrome in Korean postmenopausal women. The Journal of Korean Society of Menopause. 2012; 18(1):6–14. DOI: 10.6118/jksm.2012.18.1.6.
Article16. Lin X, Zhang X, Guo J, Roberts CK, McKenzie S, Wu WC, et al. Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials. Journal of American Heart Association. 2015; 4(7):e002014.
Article17. Díaz-Redondo A, Giráldez-García C, Carrillo L, Serrano R, García-Soidán FJ, Artola S, et al. Modifiable risk factors associated with pre-diabetes in men and women: a cross- sectional analysis of the cohort study in primary health care on the evolution of patients with pre-diabetes (PREDAPS-Study). BMC Family Practice. 2015; 16:5.
Article18. Reports of the 6th National Health and Nutrition Survey in 2014. [Internet]. Osong: Centers for Disease Control and Prevention 2014;2015. cited 2015 Octber 06. Available from: https://www.cdc.go.kr/board.es?mid=a20501000000&bid=0015&act=view&list_no=65846.19. Swindell N, Mackintosh K, McNarry M, Stephens JW, Sluik D, Fogelholm M, et al. Objectively measured physical activity and sedentary time are associated with cardiometabolic risk factors in adults with pre-diabetes: The PREVIEW Study. Diabetes Care. 2018; 41(3):562–569. DOI: 10.2337/dc17-1057.
Article20. Borel AL, Coumes S, Reche F, Ruckly S, Pépin JL, Tamisier R, et al. Waist, neck circumferences, waist-to-hip ratio: which is the best cardiometabolic risk marker in women with severe obesity? The SOON cohort. Plos One. 2018; 13(11):e0206617. DOI: 10.1371/journal.pone.0206617.
Article21. Kim JM, Back MK, Ju SH, Shin MY, Kim MJ, Park YH, et al. Validation of waist-to-height ratio for predicting metabolic syndrome in patients with pre-diabetes. The Korean Journal of Obesity. 2015; 24(1):36–43. DOI: 10.7570/kjo.2015.24.1.36.
Article22. Sigmundová D, Sigmund E, Hamrík Z, Kalman M, Pavelka J, Frömel K. Sedentary behaviour and physical activity of randomised sample of Czech adults aged 20–64 years: IPAQ and GPAQ studies between 2002 and 2011. Central European Journal of Public Health. 2015; 23 Suppl:S91–S96. DOI: 10.21101/cejph.a4142.
Article23. Lin CH, Chiang SL, Yates P, Lee MS, Hung YJ, Tzeng WC, et al. Moderate physical activity level as a protective factor against metabolic syndrome in middle-aged and older women. Journal of Clinical Nursing. 2015; 24(9-10):1234–1245. DOI: 10.1111/jocn.12683.
Article24. Ligthart S, van Herpt TT, Leening MJ, Kavousi M, Hofman A, Stricker BH, et al. Lifetime risk of developing impaired glucose metabolism and eventual progression from pre-diabetes to type 2 diabetes: a prospective cohort study. Lancet Diabetes & Endocrinology. 2016; 4(1):44–51. DOI: 10.1016/s2213-8587(15)00362-9.
Article25. American Diabetes Association. Standards of medical care in diabetes-2015 abridged for primary care providers. Clinical Diabetes. 2015; 33(2):97–111. DOI: 10.2337/diaclin.33.2.97.26. Farni K, Shoham DA, Cao G, Luke AH, Layden J, Cooper RS, et al. Physical activity and pre-diabetes-an unacknowledged mid-life crisis: findings from NHANES 2003-2006. Peer J. 2014; 2:e499. DOI: 10.7717/peerj.499.
Article27. Mayega RW, Guwatudde D, Makumbi F, Nakwagala FN, Peterson S, Tomson G, et al. Diabetes and pre-diabetes among persons aged 35 to 60 years in eastern Uganda: prevalence and associated factors. Plos One. 2013; 8(8):e72554. DOI: 10.1371/journal.pone.0072554.
Article28. Shifren JL, Gass ML. NAMS Recommendations for Clinical Care of Midlife Women Working Group. The North American Menopause Society recommendations for clinical care of midlife women. Menopause. 2014; 21(10):1038–1062. DOI: 10.1097/gme.0000000000000319.
Article29. Joo JK, Son JB, Jung JE, Kim SC, Lee KS. Differences of prevalence and components of metabolic syndrome according to menopausal status. The Journal of Korean Society of Menopause. 2012; 18(3):155–162. DOI: 10.6118/jksm.2012.18.3.155.
Article30. Harada PH, Demler OV, Dugani SB, Akinkuolie AO, Moorthy MV, Ridker P M, et al. Lipoprotein insulin resistance score and risk of incident diabetes during extended follow-up of 20 years: the women's health study. Journal of Clinical Lipidology. 2017; 11(5):1257–1267. DOI: 10.1016/j.jacl.2017.06.008.31. Flores-Guerrero JL, Connelly MA, Shalaurova I, Gruppen EG, Kieneker LM, Dullaart RP, et al. Lipoprotein insulin resistance index, a high-throughput measure of insulin resistance, is associated with incident type II diabetes mellitus in the prevention of renal and vascular end-stage disease study. Journal of Clinical Lipidology. 2019; 13(1):129–137. DOI: 10.1016/j.jacl.2018.11.009.
Article32. Mayo Clinic. Pre-diabetes [Internet]. United States: Mayo Clinic;2017. cited 2017 August 02. Available from: https://www.mayoclinic.org/diseases-conditions/prediabetes/symptoms-causes/syc-20355278.33. Ravnskov U, de Lorgeril M, Diamond DM, Hama R, Hamazaki T, Hammarskjöld B, et al. LDL-C does not cause cardiovascular disease: a comprehensive review of the current literature. Expert Review of Clinical Pharmacology. 2018; 11(10):959–970. DOI: 10.1080/17512433.2018.1519391.
Article34. Jeon J, Cho ER, Jung KJ, Jee SH. Fasting blood glucose levels trajectory and risk of cardiovascular disease in Korean population: National Health Insurance Service-National Sample Cohort (NHIS-NSC). Journal of Health Informatics Statistics. 2016; 41(4):403–410. DOI: 10.21032/jhis.2016.41.4.403.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of pre-obesity and above and its associated factors in adult women: an analysis of the 2020 Korea National Health and Nutrition Examination Survey
- Factors related to the Identification of Middle-Aged Women Who are Disadvantaged by Cardio-cerebrovascular Disease
- Trends of Diabetes and Prediabetes Prevalence among Korean Adolescents From 2007 to 2018
- Factors Influencing Glycemic Control by gender in Workers with Diabetes Mellitus
- The Influencing Factors on Health-Related Quality of Life in Childbearing Women Based on the Korea National Health and Nutrition Examination Survey (KNHANES) 2019 Data