J Korean Foot Ankle Soc.
2019 Dec;23(4):201-207. 10.14193/jkfas.2019.23.4.201.
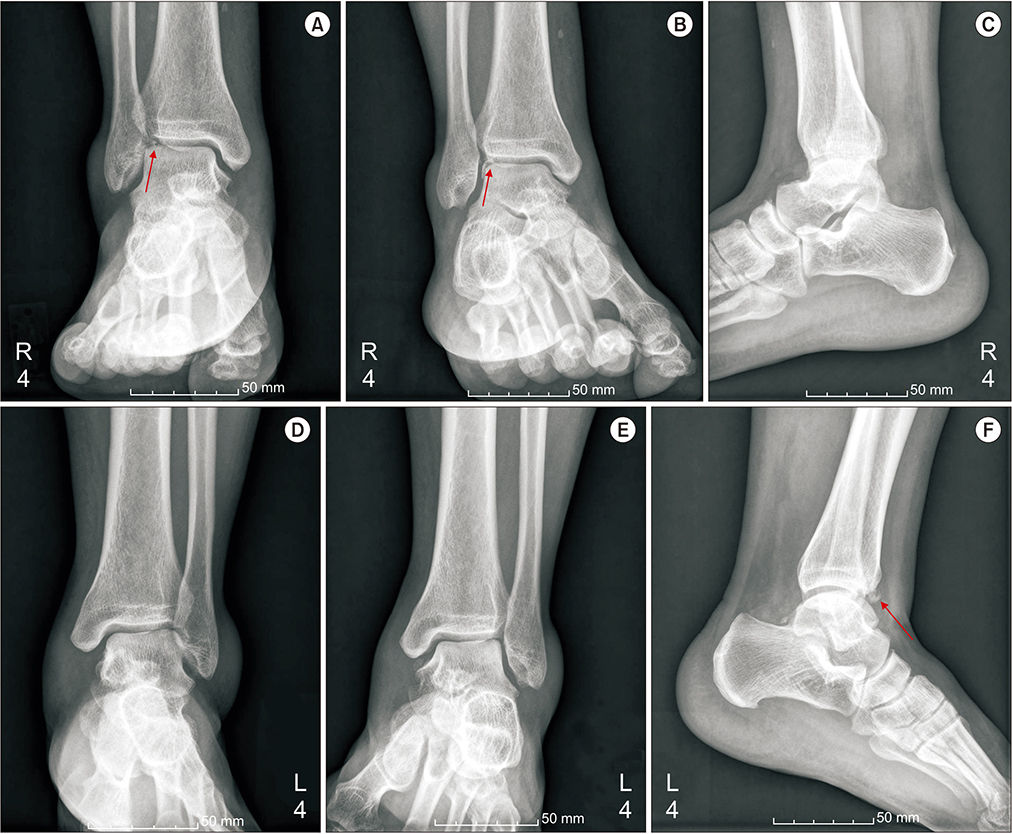
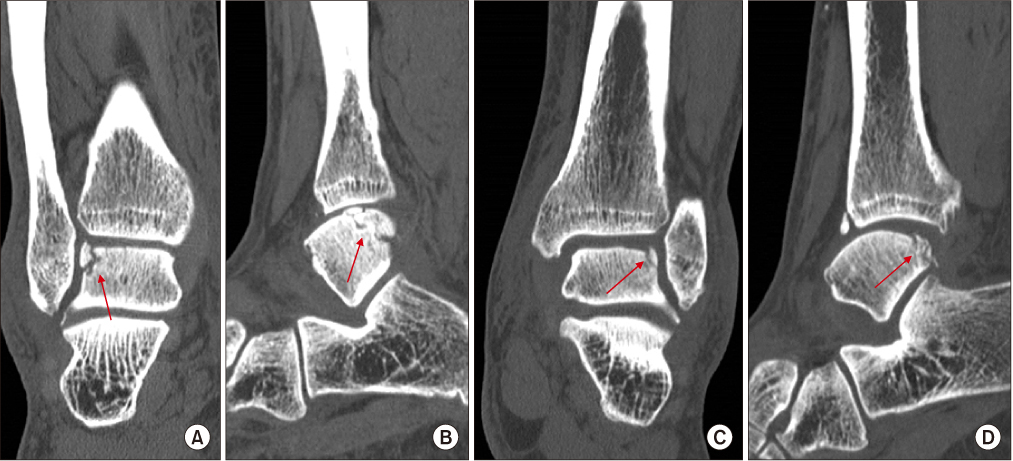
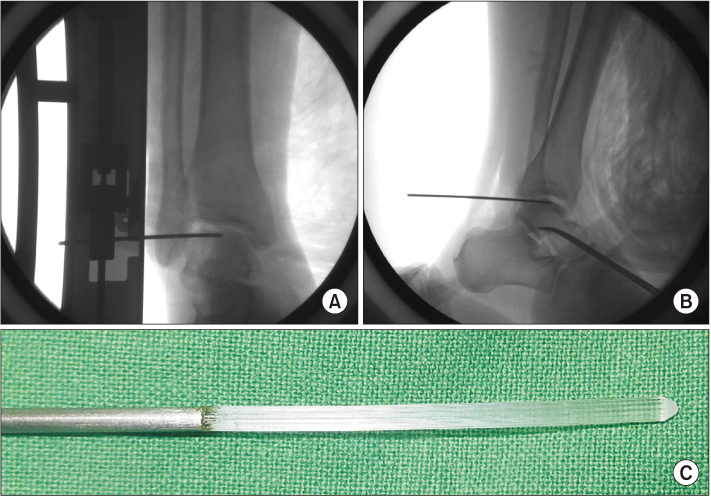
Bony Fragment Excision Followed by Multiple Drilling and Fragment Fixation Using Bio-absorbable Pins for Bilateral Osteochondral Fracture of the Lateral Talar Dome: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Inje University Ilsan Paik Hostpial, Goyang, Korea. osddr8151@paik.ac.kr
- KMID: 2465945
- DOI: http://doi.org/10.14193/jkfas.2019.23.4.201
Abstract
- An osteochondral fracture is considered to be an injury involving the cartilage and subchondral bone. Acute traumatic osteochondral fractures can be related to joint instability because abnormal joint motion causes shearing and rotatory stress. Acute osteochondral fractures are frequently missed or misdiagnosed as a pure soft tissue injury. Thus, surgeons' proactive attention is highly required as articular cartilage has limited potential for self-repair and these lesions may develop osteoarthritis. In order to minimize the progression of post-traumatic osteoarthritis, it is important to properly identify and treat osteochondral fractures. Yet, little is known about the operative management of acute osteochondral fractures of the talus. We report here on a case of a middle-aged male with acute osteochondral fractures of the bilateral lateral talar dome. We applied different operative methods on each side with regard to fragment size and stability. A favorable clinical outcome was obtained at 18 months follow-up.
MeSH Terms
Figure
Reference
-
1. Murawski CD, Kennedy JG. Operative treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 2013; 95:1045–1054. DOI: 10.2106/JBJS.L.00773.
Article2. Amendola A, Panarella L. Osteochondral lesions: medial versus lateral, persistent pain, cartilage restoration options and indications. Foot Ankle Clin. 2009; 14:215–227. DOI: 10.1016/j.fcl.2009.03.004.
Article3. Giannini S, Vannini F. Operative treatment of osteochondral lesions of the talar dome: current concepts review. Foot Ankle Int. 2004; 25:168–175. DOI: 10.1177/107110070402500311.
Article4. Rungprai C, Tennant JN, Gentry RD, Phisitkul P. Management of osteochondral lesions of the talar dome. Open Orthop J. 2017; 11:743–761. DOI: 10.2174/1874325001711010743.
Article5. Choi JY, Kim JH, Ko HT, Suh JS. Single oblique posterolateral approach for open reduction and internal fixation of posterior malleolar fractures with an associated lateral malleolar fracture. J Foot Ankle Surg. 2015; 54:559–564. DOI: 10.1053/j.jfas.2014.09.043.
Article6. Hermanson E, Ferkel RD. Bilateral osteochondral lesions of the talus. Foot Ankle Int. 2009; 30:723–727. DOI: 10.3113/FAI.2009.0723.
Article7. Verhagen RA, Struijs PA, Bossuyt PM, van Dijk CN. Systematic review of treatment strategies for osteochondral defects of the talar dome. Foot Ankle Clin. 2003; 8:233–242. DOI: 10.1016/s1083-7515(02)00064-5.
Article8. Hannon CP, Smyth NA, Murawski CD, Savage-Elliott I, Deyer TW, Calder JD, et al. Osteochondral lesions of the talus: aspects of current management. Bone Joint J. 2014; 96:164–171. DOI: 10.1302/0301-620X.96B2.31637.9. Pedersen ME, DaCambra MP, Jibri Z, Dhillon S, Jen H, Jomha NM. Acute osteochondral fractures in the lower extremities - approach to identification and treatment. Open Orthop J. 2015; 9:463–474. DOI: 10.2174/1874325001509010463.
Article10. Di Cave E, Versari P, Sciarretta F, Luzon D, Marcellini L. Biphasic bioresorbable scaffold (TruFit Plug®) for the treatment of osteochondral lesions of talus: 6- to 8-year follow-up. Foot (Edinb). 2017; 33:48–52. DOI: 10.1016/j.foot.2017.05.005.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Results of the Multiple Drilling for Osteochondral Lesion of the Medial Talar Dome
- Sbuchondral Curettage & Bone Peg Fixation in Osteochondral Fracture of The Talus
- Capitellar Osteochondral Impacted Fracture of the Humerus in an Adult Female: A Case Report
- Arthroscopic Fragment Excision of Pipkin Type I Displaced Femoral Head Fracture: A Case Report
- Avulsion Fracture of the Talar Attachment of the Anterior Talofibular Ligament in Pediatric Patient: A Case Report