J Cerebrovasc Endovasc Neurosurg.
2019 Jun;21(2):77-85. 10.7461/jcen.2019.21.2.77.
Long-term Prognosis of Patients Who Contraindicated for Intravenous Thrombolysis in Acute Ischemic Stroke
- Affiliations
-
- 1Department of Public Health, Graduate school of Korea University, Seoul, South Korea.
- 2Department of Neurosurgery, College of Medicine, Soonchunhyang University, Cheonnan Hospital, South Korea. metatron1324@hotmail.com
- KMID: 2465200
- DOI: http://doi.org/10.7461/jcen.2019.21.2.77
Abstract
- BACKGROUND
As intravenous thrombolysis (IVT) has very restricted inclusion criteria, eligible patients of IVT constitute a very small proportion and studies about their mortality are rare. The long-term mortality in a patients with contraindication of ineligible patients of IVT still under the debate. So, we investigated the proportion of patients with contraindication of IVT and the short and long-term mortality of them in AIS on emergency department comparing with the long-term effect of IVT in patients with moderate-to-severe stroke.
METHODS
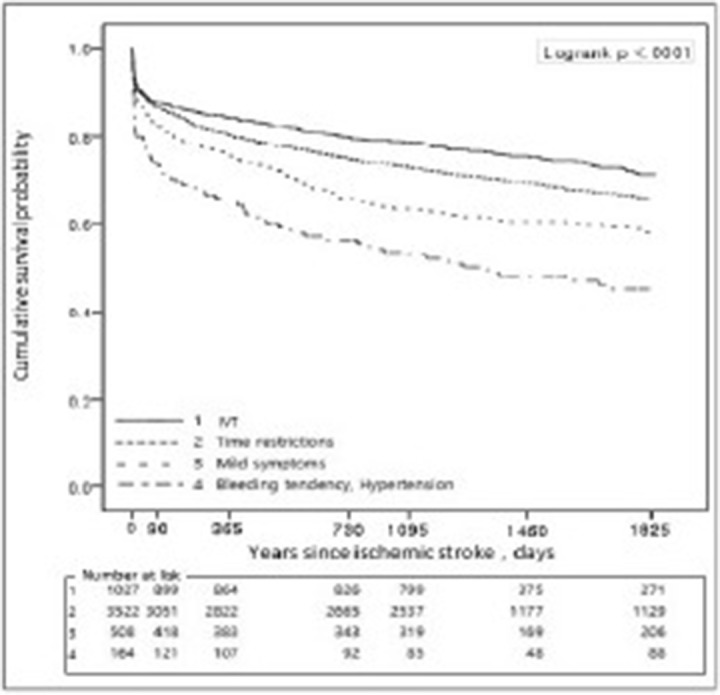
Using acute stroke assessment indication registry & Health Insurance Review and Assessment Service database, a total of 5,407 patients with NIHSS≥5 were selected from a total of 169 acute stroke care hospital nationwide during October-December 2011 and March-June 2013. We divided AIS patients into two groups: 1) IVT group who received IVT within 4.5 hours, and 2) non-IVT group who did not receive the IVT because of contraindications. And we divided the subgroups according to the reason of contraindication of IVT. The 5-year survival rate of each group was assessed using Kaplan-Meyer survival analysis.
RESULTS
Of the 5,407 patients, a total of 1,027 (19%) patients who received IVT using r-tPA within 4.5 h after onset. Compared with the IVT group, hazard ratios of non-IVT group were 1.33 at 3 months, 1.53 at 1 year and 1.47 at 5 years (p<.001). A total of 4,380 patients did not receive IVT because of the following contraindications to IVT. 1) Time restriction: 3,378 (77.1 %) patients were admitted after 4.5 h following stroke onset, and 144 (3.3%) patients failed to determine the stroke onset time. 2) Mild symptoms:137 (3.1%) patients had rapid improvement or mild stroke on emergency room, 3) Bleeding diathesis or non-adjustable hypertension: 53 (1.2%) patients showed a bleeding tendency or severe hypertension. Compared with the IVT group, the subgroups of non-IVT group showed consistently high mortality during short and long term follow up. Mild symptom and bleeding diathesis or non-adjustable hypertension subgroup in the non-IVT group consistently showed the higher mortality than time restriction subgroup during the short and long-term follow-up (log-rank p<.001). Patients who had rapid improvement or mild stroke on emergency department had the higher mortality than time restriction group in short and long term follow up.
CONCLUSION
The AIS patients with rapid improvement or mild stroke on emergency room had higher mortality than ineligible patients of IVT due to time restriction during the short and long-term follow-up. A further management and special support on emergency department is needed for these patients with initially mild stroke and rapid improvement in AIS to reduce the poor outcome.
Keyword
MeSH Terms
Figure
Reference
-
1. Albers GW, Bates VE, Clark WM, Bell R, Verro P, Hamilton SA. Intravenous tissue-type plasminogen activator for treatment of acute stroke: the Standard Treatment with Alteplase to Reverse Stroke (STARS) study. JAMA. 2000; 3. 01. 283(9):1145–1150. PMID: 10703776.2. Breuer L, Blinzler C, Huttner HB, Kiphuth IC, Schwab S, Kohrmann M. Off-label thrombolysis for acute ischemic stroke: rate, clinical outcome and safety are influenced by the definition of ‘minor stroke’. Cerebrovasc Dis. 2011; 8. 32(2):177–185. PMID: 21849777.
Article3. Brunner F, Tomandl B, Schroter A, Mellinghoff C, Haldenwanger A, Hildebrandt H, et al. Hemorrhagic complications after systemic thrombolysis in acute stroke patients with abnormal baseline coagulation. Eur J Neurol. 2011; 12. 18(12):1407–1411. PMID: 21672089.
Article4. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with Alteplase 3 to 4.5 Hours after Acute Ischemic Stroke. N Engl J Med. 2008; 9. 359(13):1317–1329. PMID: 18815396.
Article5. Katzan IL, Furlan AJ, Lloyd LE, Frank JI, Harper DL, Hinchey JA, et al. Use of tissue-type plasminogen activator for acute ischemic stroke: the Cleveland area experience. JAMA. 2000; 3. 283(9):1151–1158. PMID: 10703777.6. Kim JT, Park MS, Chang J, Lee JS, Choi K-H, Cho KH. Proximal Arterial Occlusion in Acute Ischemic Stroke with Low NIHSS Scores Should Not Be Considered as Mild Stroke. PLOS ONE. 2013; 8. 8(8):e70996. PMID: 23976971.
Article7. Lopez-Yunez AM, Bruno A, Williams LS, Yilmaz E, Zurrú C, Biller J. Protocol violations in community-based rTPA stroke treatment are associated with symptomatic intracerebral hemorrhage. Stroke. 2001; 1. 32(1):12–16. PMID: 11136907.
Article8. Mazya M, Egido JA, Ford GA, Lees KR, Mikulik R, Toni D, et al. Predicting the risk of symptomatic intracerebral hemorrhage in ischemic stroke treated with intravenous alteplase: safe Implementation of Treatments in Stroke (SITS) symptomatic intracerebral hemorrhage risk score. Stroke. 2012; 6. 43(6):1524–1531. PMID: 22442178.9. Meretoja A, Putaala J, Tatlisumak T, Atula S, Artto V, Curtze S, et al. Off-label thrombolysis is not associated with poor outcome in patients with stroke. Stroke. 2010; 7. 41(7):1450–1458. PMID: 20538701.
Article10. Nedeltchev K, Schwegler B, Haefeli T, Brekenfeld C, Gralla J, Fischer U, et al. Outcome of stroke with mild or rapidly improving symptoms. Stroke. 2007; 9. 38(9):2531–2535. PMID: 17673713.
Article11. Rajajee V, Kidwell C, Starkman S, Ovbiagele B, Alger JR, Villablanca P, et al. Early MRI and outcomes of untreated patients with mild or improving ischemic stroke. Neurology. 2006; 9. 26. 67(6):980–984. PMID: 17000964.
Article12. Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E, Delgado P, Montaner J, et al. Tandem internal carotid artery/middle cerebral artery occlusion: an independent predictor of poor outcome after systemic thrombolysis. Stroke. 2006; 9. 37(9):2301–2305. PMID: 16888266.13. Smith EE, Abdullah AR, Petkovska I, Rosenthal E, Koroshetz WJ, Schwamm LH. Poor outcomes in patients who do not receive intravenous tissue plasminogen activator because of mild or improving ischemic stroke. Stroke. 2005; 11. 36(11):2497–2499. PMID: 16210552.
Article14. Tanne D, Kasner SE, Demchuk AM, Koren-Morag N, Hanson S, Grond M, et al. Markers of increased risk of intracerebral hemorrhage after intravenous recombinant tissue plasminogen activator therapy for acute ischemic stroke in clinical practice: the Multicenter rt-PA Stroke Survey. Circulation. 2002; 4. 09. 105(14):1679–1685. PMID: 11940547.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Treatment of Acute Ischemic Stroke: Thrombolysis
- Interventional Recanalization Treatment of Acute Ischemic Stroke
- Thrombolytic Treatment of Acute Stroke
- Antiplatelet Therapy for Secondary Stroke Prevention in Patients with Ischemic Stroke or Transient Ischemic Attack