Arch Hand Microsurg.
2019 Dec;24(4):351-357. 10.12790/ahm.2019.24.4.351.
A Case of SAPHO Syndrome with Hyperostosis of the Ulna
- Affiliations
-
- 1Department of Orthopedic Surgery, Pusan National University Yangsan Hospital, Yangsan, Korea. shkwak2013@gmail.com
- 2Department of Orthopedic Surgery, Pusan National University Hospital, Busan, Korea.
- 3Department of Dermatology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 4Department of Radiology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2464471
- DOI: http://doi.org/10.12790/ahm.2019.24.4.351
Abstract
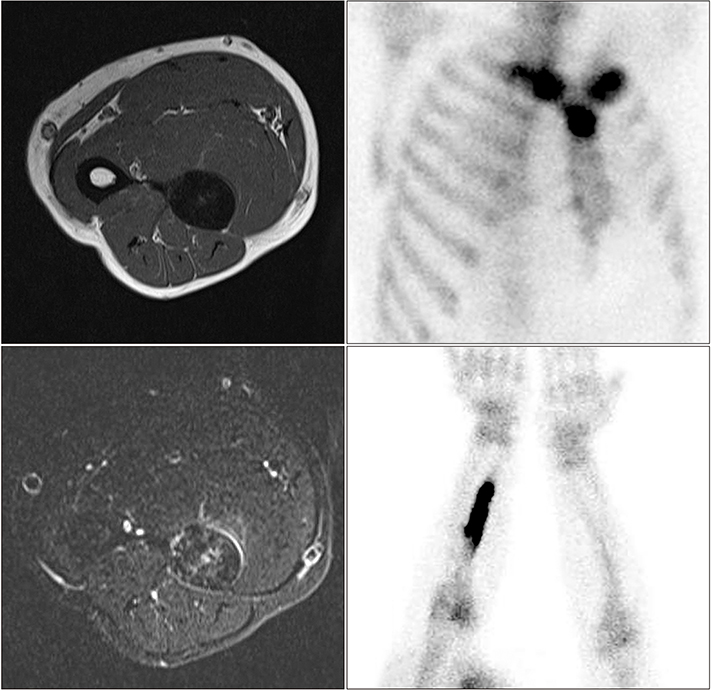
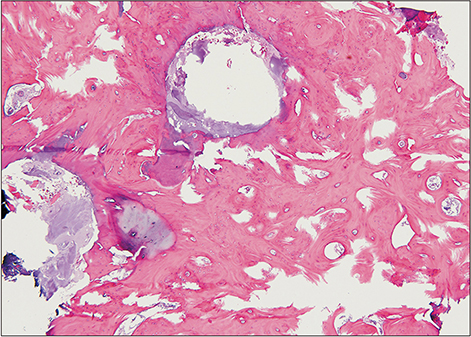
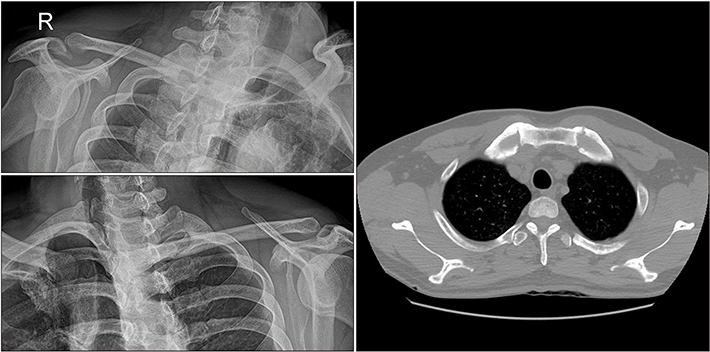
- SAPHO syndrome is a rare disease comprising of synovitis, acne, pustulosis, hyperostosis, and osteitis and osteoarticular manifestations usually involve anterior chest wall, spine, or pelvis. Among these features, hyperostosis of long bone was rarely reported on the upper extremity. The present case is about a 49-year-old male with painful hyperostosis of his ulna, diagnosed with SAPHO syndrome. The diagnostic process and the progress after two years are described.
Keyword
MeSH Terms
Figure
Reference
-
1. Takigawa T, Tanaka M, Nakanishi K, et al. SAPHO syndrome associated spondylitis. Eur Spine J. 2008; 17:1391–1397.
Article2. Rukavina I. SAPHO syndrome: a review. J Child Orthop. 2015; 9:19–27.
Article3. Zemann W, Pau M, Feichtinger M, Ferra-Matschy B, Kaercher H. SAPHO syndrome with affection of the mandible: diagnosis, treatment, and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 111:190–195.
Article4. Okuno H, Watanuki M, Kuwahara Y, et al. Clinical features and radiological findings of 67 patients with SAPHO syndrome. Mod Rheumatol. 2018; 28:703–708.
Article5. Reith JD, Bauer TW, Schils JP. Osseous manifestations of SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome. Am J Surg Pathol. 1996; 20:1368–1377.
Article6. Benhamou CL, Chamot AM, Kahn MF. Synovitis-acnepustulosis hyperostosis-osteomyelitis syndrome (SAPHO). A new syndrome among the spondyloarthropathies? Clin Exp Rheumatol. 1988; 6:109–112.7. Ferguson PJ, Sandu M. Current understanding of the pathogenesis and management of chronic recurrent multifocal osteomyelitis. Curr Rheumatol Rep. 2012; 14:130–141.
Article8. Firinu D, Garcia-Larsen V, Manconi PE, Del Giacco SR. SAPHO syndrome: current developments and approaches to clinical treatment. Curr Rheumatol Rep. 2016; 18:35.
Article9. Hayem G, Bouchaud-Chabot A, Benali K, et al. SAPHO syndrome: a long-term follow-up study of 120 cases. Semin Arthritis Rheum. 1999; 29:159–171.
Article10. Golla A, Jansson A, Ramser J, et al. Chronic recurrent multifocal osteomyelitis (CRMO): evidence for a susceptibility gene located on chromosome 18q21.3-18q22. Eur J Hum Genet. 2002; 10:217–221.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Refractory SAPHO Syndrome Treated with Etanercept
- A Case of SAPHO Syndrome
- A Case of Palmoplantar Pustulosis Present in the Daughter of a SAPHO Syndrome Patient
- SAPHO (Synovitis, Acne, Pustulosis, Hyperostosis, Osteitis) Syndrome occurred on the Clavicle: A Case Report
- Two Cases of SAPHO Syndrome