J Rheum Dis.
2015 Apr;22(2):127-131. 10.4078/jrd.2015.22.2.127.
A Case of Palmoplantar Pustulosis Present in the Daughter of a SAPHO Syndrome Patient
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Kyung Hee University School of Medicine, Seoul, Korea. hsj718@paran.com
- KMID: 2222917
- DOI: http://doi.org/10.4078/jrd.2015.22.2.127
Abstract
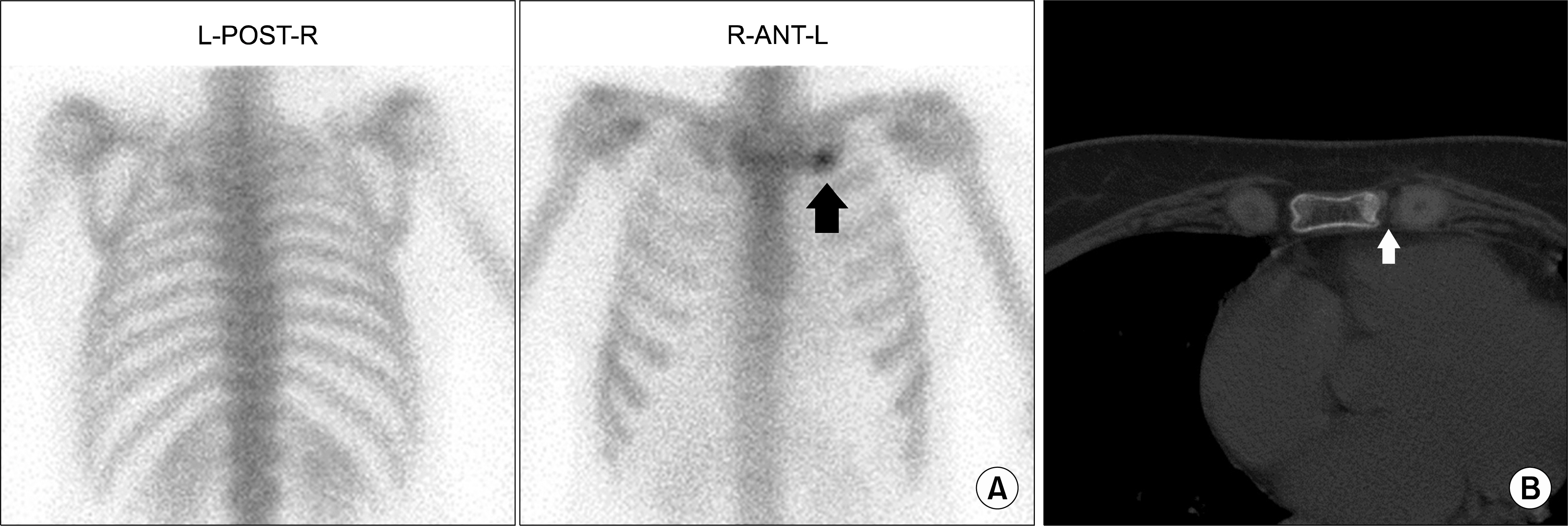
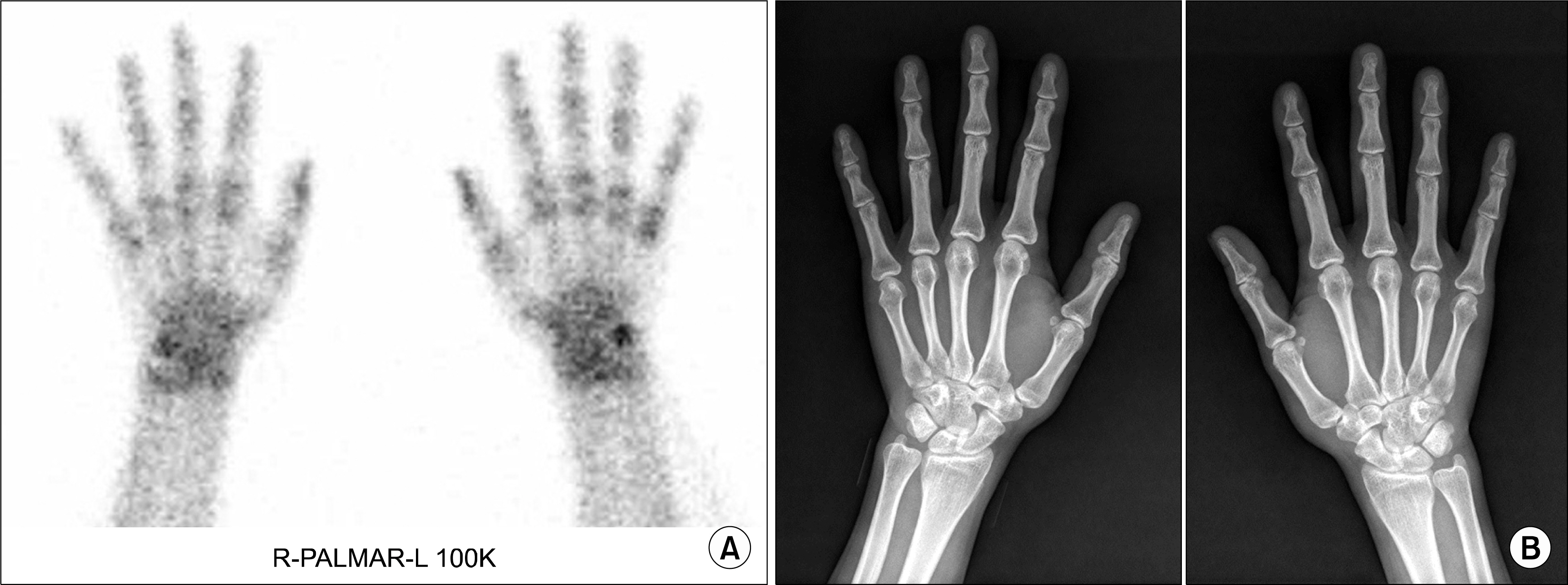
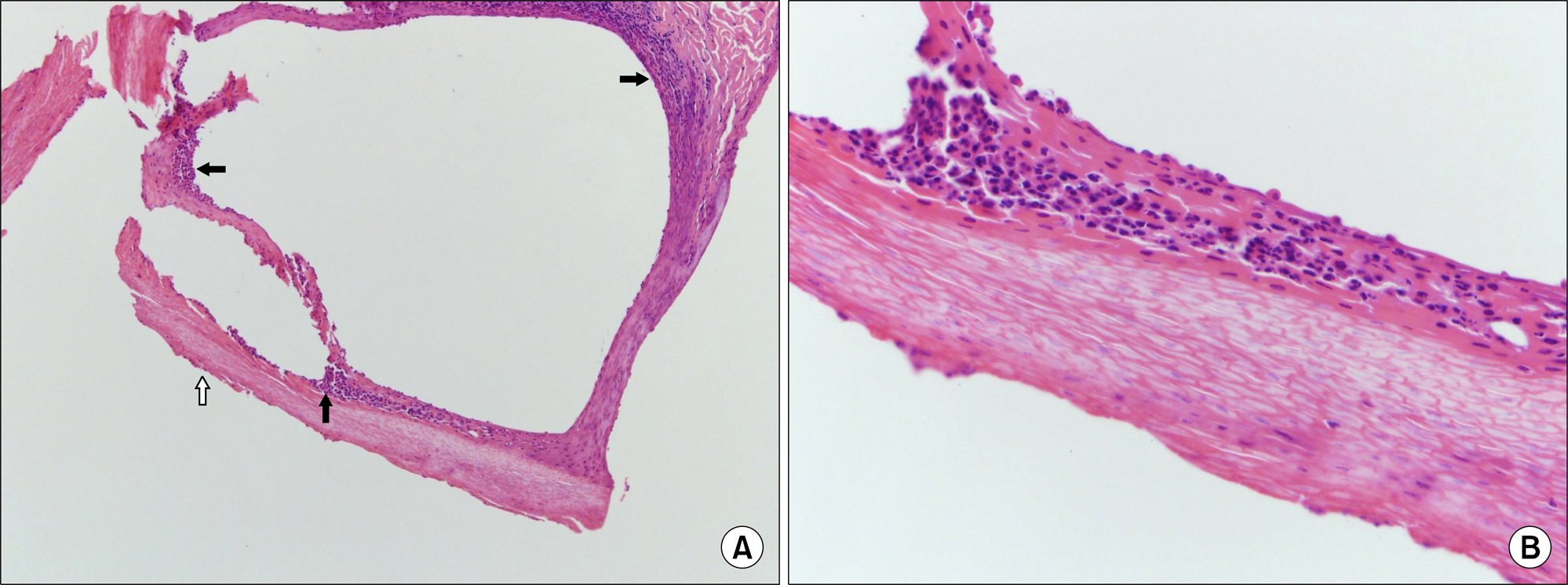
- SAPHO syndrome is a rare inflammatory, pseudoinfectious disease. Initially it was an acronym for Syndrome Acne Pustulosis Hyperostosis Osteitis, and the meaning of S was later changed to synovitis. It occurs predominantly in children and adults and is not common over 60 years. The most common clinical presentation is osteoarticular involvement at the anterior chest wall and skin manifestations may be evident, but it could occur years earlier or develop later. We report on two cases of mother and daughter. A 51-year-old female was diagnosed with SAPHO syndrome with costochondritis and palmoplantar pustulosis. Five years later, her 31-year-old daughter presented with similar skin manifestations of the hand and foot.
MeSH Terms
Figure
Reference
-
1. Chamot AM, Benhamou CL, Kahn MF, Beraneck L, Kaplan G, Prost A. Acne-pustulosis-hyperostosis-osteitis syndrome. Results of a national survey. 85 cases. Rev Rhum Mal Osteoartic. 1987; 54:187–96.2. Kahn MF, Chamot AM. SAPHO syndrome. Rheum Dis Clin North Am. 1992; 18:225–46.
Article3. Nguyen MT, Borchers A, Selmi C, Naguwa SM, Cheema G, Gershwin ME. The SAPHO syndrome. Semin Arthritis Rheum. 2012; 42:254–65.
Article4. Yun HR, Jung SS, Koh HK, Yoo TS, Lee JK, Hong KP, et al. Two cases of SAPHO syndrome. J Korean Rheum Assoc. 1997; 4:162–7.5. Park JH, Suh HS, Seo KW, Jeong ID, Jung HC, Lee JS, et al. Two cases of SAPHO syndrome. Korean J Med. 2003; 65(Suppl 3):S782–7.6. Kim YJ, Bae SI, Choi SJ, Lee YH, Ji JD, Song GG. A case of refractory SAPHO syndrome treated with etanercept. J Rheum Dis. 2012; 19:51–4.
Article7. Depasquale R, Kumar N, Lalam RK, Tins BJ, Tyrrell PN, Singh J, et al. SAPHO: what radiologists should know. Clin Radiol. 2012; 67:195–206.
Article8. Sonozaki H, Mitsui H, Miyanaga Y, Okitsu K, Igarashi M, Hayashi Y, et al. Clinical features of 53 cases with pustulotic arthro-osteitis. Ann Rheum Dis. 1981; 40:547–53.
Article9. Benhamou CL, Chamot AM, Kahn MF. Synovitis-acne-pus-tulosis hyperostosis-osteomyelitis syndrome (SAPHO). A new syndrome among the spondyloarthropathies? Clin Exp Rheumatol. 1988; 6:109–12.10. Carneiro S, Sampaio-Barros PD. SAPHO syndrome. Rheum Dis Clin North Am. 2013; 39:401–18.
Article11. Dumolard A, Gaudin P, Juvin R, Bost M, Peoc'h M, Phelip X. SAPHO syndrome or psoriatic arthritis? A familial case study. Rheumatology (Oxford). 1999; 38:463–7.
Article12. Witt M, Meier J, Hammitzsch A, Proft F, Schulze-Koops H, Grunke M. Disease burden, disease manifestations and current treatment regimen of the SAPHO syndrome in Germany: results from a nationwide patient survey. Semin Arthritis Rheum. 2014; 43:745–50.
Article13. Assmann G, Wagner AD, Monika M, Pfoehler C, Pfreundschuh M, Tilgen W, et al. Single-nucleotide polymorphisms p53 G72C and Mdm2 T309G in patients with psoriasis, psoriatic arthritis, and SAPHO syndrome. Rheumatol Int. 2010; 30:1273–6.
Article14. Gudkov AV, Komarova EA. Dangerous habits of a security guard: the two faces of p53 as a drug target. Hum Mol Genet. 2007; (16 Spec No 1):R67–72.
Article15. Ichikawa J, Sato E, Haro H, Ando T, Maekawa S, Hamada Y. Successful treatment of SAPHO syndrome with an oral bisphosphonate. Rheumatol Int. 2009; 29:713–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of SAPHO Syndrome in a Palmoplantar Pustulosis Patient
- Two Cases of SAPHO Syndrome
- A Case of SAPHO Syndrome Associated with Lytic Bone Lesions Resembling Metastases
- Two cases of SAPHO syndrome
- Usefulness of the Automated Bone Scan Index in Arthritis: A Quantitative Approach for Evaluating Synovitis, Acne, Pustulosis, Hyperostosis, and Osteitis (SAPHO) Syndrome