Arch Hand Microsurg.
2019 Dec;24(4):311-320. 10.12790/ahm.2019.24.4.311.
Treatment of Unstable Scaphoid Nonunion Using a Volar Locking Plate
- Affiliations
-
- 1Department of Orthopaedic Surgery, Korea University Anam Hospital, Seoul, Korea. ospark@korea.ac.kr
- 2Department of Orthopaedic Surgery, Korea University Guro Hospital, Seoul, Korea.
- KMID: 2464466
- DOI: http://doi.org/10.12790/ahm.2019.24.4.311
Abstract
- PURPOSE
The purpose of this study is to assess the results of treatment of unstable scaphoid nonunion using a wedge iliac crest bone graft and a volar locking plate and screw system.
METHODS
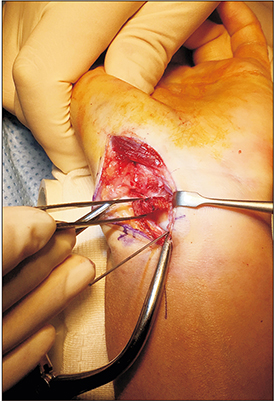
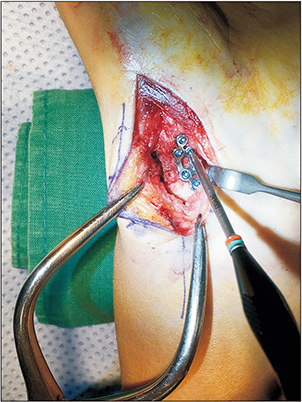
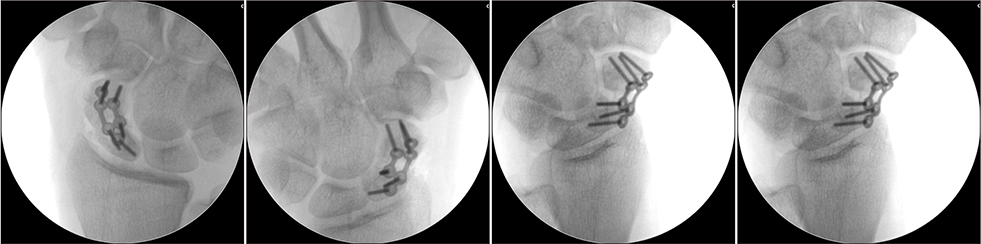
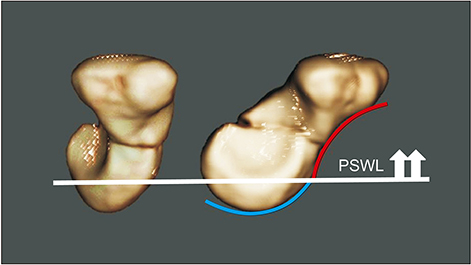
Seventeen patients are included in the study and the average age was 30.4 years. The mean duration of non-union was 44.8 months. All patients underwent open reduction, wedge-bone grafting from the iliac crest, and internal fixation using a 1.5 mm volar locking plate and screw. The nonunion sites were scaphoid waist in 12 patients and proximal pole in 5 patients. The mean follow up periods after the operation was 10.2 months. The mean union time was determined with plain radiographs and computed tomography scan. At final follow-up, range of motion (ROM) of the wrist, scapholunate and radiolunate angles, and height-to-length ratio were measured.
RESULTS
All 17 scaphoids united in a mean time of 7.9 weeks after operation. Both scapholunate angle and radiolunate angles are recovered within the normal range. The average extension-flexion arc of the injured wrists was 127.9 degrees, which was improved over 34% of preoperative ROM. Pro- and supination were normal. There was no hardware related problems and no plate removal was necessary during the follow-up period.
CONCLUSION
The use of an anatomical 1.5 mm volar locking plate with an anterior wedge iliac bone graft provides optimal stability for the unstable scaphoid nonunion. The rapid union after the plate fixation allowed earlier rehabilitation without cast immobilization which is usually performed with other fixation methods.
Keyword
MeSH Terms
Figure
Reference
-
1. Mclaughlin HL. Fracture of the carpal navicular (scaphoid) bone; some observations based on treatment by open reduction and internal fixation. J Bone Joint Surg Am. 1954; 36-A:765–774.2. Barton NJ. Experience with scaphoid grafting. J Hand Surg Br. 1997; 22:153–160.
Article3. Schuind F, Moungondo F, El Kazzi W. Prognostic factors in the treatment of carpal scaphoid non-unions. Eur J Orthop Surg Traumatol. 2017; 27:3–9.
Article4. Amadio PC, Berquist TH, Smith DK, Ilstrup DM, Cooney WP 3rd, Linscheid RL. Scaphoid malunion. J Hand Surg Am. 1989; 14:679–687.
Article5. Trumble TE, Clarke T, Kreder HJ. Non-union of the scaphoid. Treatment with cannulated screws compared with treatment with Herbert screws. J Bone Joint Surg Am. 1996; 78:1829–1837.
Article6. Dodds SD, Patterson JT, Halim A. Volar plate fixation of recalcitrant scaphoid nonunions with volar carpal artery vascularized bone graft. Tech Hand Up Extrem Surg. 2014; 18:2–7.
Article7. Slade JF 3rd, Dodds SD. Minimally invasive management of scaphoid nonunions. Clin Orthop Relat Res. 2006; 445:108–119.
Article8. Park HY, Yoon JO, Jeon IH, Chung HW, Kim JS. A comparison of the rates of union after cancellous iliac crest bone graft and Kirschner-wire fixation in the treatment of stable and unstable scaphoid nonunion. Bone Joint J. 2013; 95-B:809–814.
Article9. Tomaino MM, King J, Pizillo M. Correction of lunate malalignment when bone grafting scaphoid nonunion with humpback deformity: rationale and results of a technique revisited. J Hand Surg Am. 2000; 25:322–329.
Article10. Nakamura R, Horii E, Watanabe K, Tsunoda K, Miura T. Scaphoid non-union: factors affecting the functional outcome of open reduction and wedge grafting with Herbert screw fixation. J Hand Surg Br. 1993; 18:219–224.
Article11. Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984; 66:114–123.
Article12. Fernandez DL. Anterior bone grafting and conventional lag screw fixation to treat scaphoid nonunions. J Hand Surg Am. 1990; 15:140–147.
Article13. Radford PJ, Matthewson MH, Meggitt BF. The Herbert screw for delayed and non-union of scaphoid fractures: a review of fifty cases. J Hand Surg Br. 1990; 15:455–459.
Article14. Ford DJ, Khoury G, el-Hadidi S, Lunn PG, Burke FD. The Herbert screw for fractures of the scaphoid. A review of results and technical difficulties. J Bone Joint Surg Br. 1987; 69:124–127.
Article15. Inoue G, Shionoya K, Kuwahata Y. Ununited proximal pole scaphoid fractures. Treatment with a Herbert screw in 16 cases followed for 0.5–8 years. Acta Orthop Scand. 1997; 68:124–127.
Article16. del Piñal F. Treatment of nonunion of the scaphoid by a limited combined approach. J Bone Joint Surg Br. 2001; 83:78–82.
Article17. Cooney WP, Linscheid RL, Dobyns JH, Wood MB. Scaphoid nonunion: role of anterior interpositional bone grafts. J Hand Surg Am. 1988; 13:635–650.
Article18. Ghoneim A. The unstable nonunited scaphoid waist fracture: results of treatment by open reduction, anterior wedge grafting, and internal fixation by volar buttress plate. J Hand Surg Am. 2011; 36:17–24.
Article19. Leixnering M, Pezzei C, Weninger P, et al. First experiences with a new adjustable plate for osteosynthesis of scaphoid nonunions. J Trauma. 2011; 71:933–938.
Article20. Putnam JG, Mitchell SM, DiGiovanni RM, Stockwell EL, Edwards SG. Outcomes of unstable scaphoid nonunion with segmental defect treated with plate fixation and autogenous cancellous graft. J Hand Surg Am. 2019; 44:160.e1–160.e7.
Article21. Jurkowitsch J, Dall'Ara E, Quadlbauer S, et al. Rotational stability in screw-fixed scaphoid fractures compared to plate-fixed scaphoid fractures. Arch Orthop Trauma Surg. 2016; 136:1623–1628.
Article22. Mandaleson A, Tham SK, Lewis C, Ackland DC, Ek ET. Scaphoid fracture fixation in a nonunion model: a biomechanical study comparing 3 types of fixation. J Hand Surg Am. 2018; 43:221–228.
Article23. Goodwin JA, Castañeda P, Shelhamer RP, Bosch LC, Edwards SG. A comparison of plate versus screw fixation for segmental scaphoid fractures: a biomechanical study. Hand (N Y). 2019; 14:203–208.
Article24. Hove LM. Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg. 1999; 33:423–426.
Article25. Bond CD, Shin AY, McBride MT, Dao KD. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am. 2001; 83:483–488.
Article26. Brydie A, Raby N. Early MRI in the management of clinical scaphoid fracture. Br J Radiol. 2003; 76:296–300.
Article27. Gellman H, Caputo RJ, Carter V, Aboulafia A, McKay M. Comparison of short and long thumb-spica casts for nondisplaced fractures of the carpal scaphoid. J Bone Joint Surg Am. 1989; 71:354–357.
Article28. Esteban-Feliu I, Barrera-Ochoa S, Vidal-Tarrason N, Mir-Simon B, Lluch A, Mir-Bullo X. Volar plate fixation to treat scaphoid nonunion: a case series with minimum 3 years of follow-up. J Hand Surg Am. 2018; 43:569.e1–569.e8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- External Fixation for Distal Radius Fractures
- 2.4 mm Volar Locking Compression Plate for Treatment of Unstable Distal Radius Fractures
- Volar T-Locking Compression Plate for Treatment of Unstable Distal Radius Fractures
- Short Term Results of Operative Management with 2.4 mm Volar Locking Compression Plates in Distal Radius Fractures
- Comparative Analysis of the Results of Fixed-angle versus Variable-angle Volar Locking Plate for Distal Radius Fracture Fixation