Cancer Res Treat.
2019 Apr;51(2):519-529. 10.4143/crt.2018.146.
A Comprehensive Assessment of the Racial and Ethnic Disparities in the Incidence of Gastric Cancer in the United States, 1992-2014
- Affiliations
-
- 1Department of Ultrasound Intervention, Harbin Medical University Cancer Hospital, Harbin, China. ambercountry@foxmail.com
- 2Heilongjiang Provincial Academy of Medical Sciences, Harbin, China.
- 3Nursing Department, Harbin Medical University Cancer Hospital, Harbin, China.
- 4Upper Gastrointestinal Surgery, Department of Molecular Medicine and Surgery, Karolinska Institutet, Karolinska University Hospital, Stockholm, Sweden.
- KMID: 2464399
- DOI: http://doi.org/10.4143/crt.2018.146
Abstract
- PURPOSE
This study aimed to evaluate the racial and ethnic disparities in the incidence of gastric cancer and their temporal trends in the United States.
MATERIALS AND METHODS
Using data from 13 cancer registries in the Surveillance, Epidemiology, and End Results database, we assessed such disparities during 1992-2014 in the United States using a variety of disparity metrics.
RESULTS
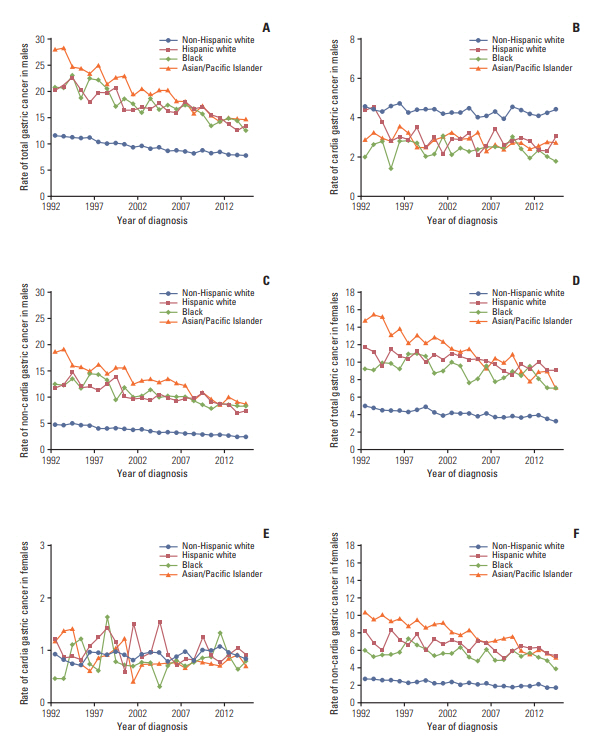
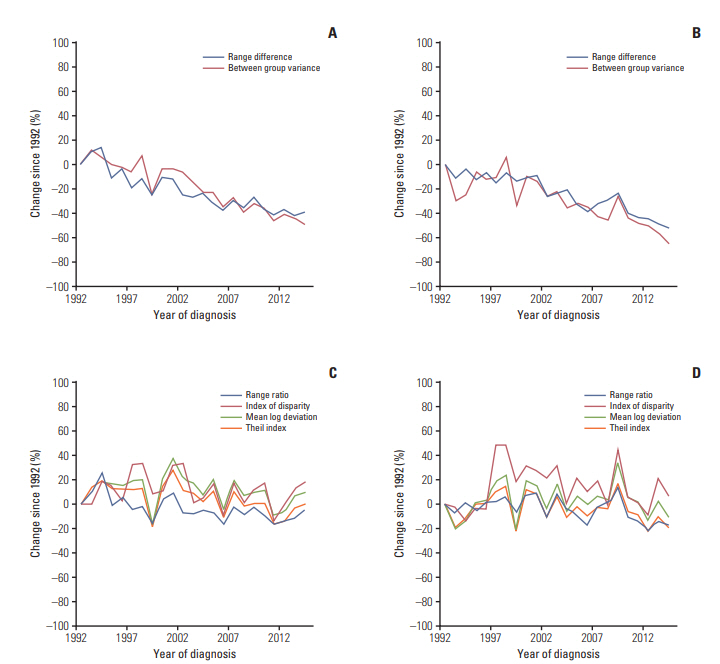
The age-standardized incidence rate of non-cardia gastric cancer was highest in Asian and Pacific Islanders, while the incidence of cardia gastric was highest in non-Hispanic whites in men and was similarly low in all groups in women. The incidence of non-cardia gastric cancer decreased in all groups over time, particularly in Asian and Pacific Islanders (on average by 3% per year). The incidence of cardia gastric remained relatively stable in virtually all racial/ethnic groups. The racial and ethnic disparities in gastric cancer incidence steadily decreased over time as measured on the absolute scale, which was mainly driven by the reduced disparities in non-cardia gastric cancer. The range difference in the incidence of gastric cancer decreased on average by 4.1% per year in men and by 2.6% per year in women from 1992 to 2014. The between group variance decreased by 5.6% per year in men and by 3.4% per year in women. The relative-scale disparity measures generally remained stable over time.
CONCLUSION
This study demonstrates decreased racial and ethnic disparities in the incidence of gastric cancer over time in the United States, particularly as measured on the absolute scale.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, et al. Global, regional, and national cancer incidence, mortality, years of Life lost, years lived with disability, and disability-adjusted lifeyears for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol. 2017; 3:524–48.2. Karimi P, Islami F, Anandasabapathy S, Freedman ND, Kamangar F. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomarkers Prev. 2014; 23:700–13.
Article3. Rugge M, Genta RM, Di Mario F, El-Omar EM, El-Serag HB, Fassan M, et al. Gastric cancer as preventable disease. Clin Gastroenterol Hepatol. 2017; 15:1833–43.
Article4. Colquhoun A, Arnold M, Ferlay J, Goodman KJ, Forman D, Soerjomataram I. Global patterns of cardia and non-cardia gastric cancer incidence in 2012. Gut. 2015; 64:1881–8.
Article5. Wu X, Chen VW, Ruiz B, Andrews P, Su LJ, Correa P. Incidence of esophageal and gastric carcinomas among American Asians/Pacific Islanders, whites, and blacks: subsite and histology differences. Cancer. 2006; 106:683–92.6. Wu X, Chen VW, Andrews PA, Ruiz B, Correa P. Incidence of esophageal and gastric cancers among Hispanics, non-Hispanic whites and non-Hispanic blacks in the United States: subsite and histology differences. Cancer Causes Control. 2007; 18:585–93.
Article7. Kubo A, Corley DA. Marked multi-ethnic variation of esophageal and gastric cardia carcinomas within the United States. Am J Gastroenterol. 2004; 99:582–8.
Article8. Surveillance Research Program, National Cancer Institute. SEER*Stat software, version 8.3.4 [Internet]. Bethesda, MD: National Cancer Institute;2018. [cited 2018 Jun 2]. Available from: http://seer.cancer.gov/seerstat.9. Xie SH, Rabbani S, Petrick JL, Cook MB, Lagergren J. Racial and ethnic disparities in the incidence of esophageal cancer in the United States, 1992-2013. Am J Epidemiol. 2017; 186:1341–51.
Article10. Harper S, Lynch J, Meersman SC, Breen N, Davis WW, Reichman ME. An overview of methods for monitoring social disparities in cancer with an example using trends in lung cancer incidence by area-socioeconomic position and race-ethnicity, 1992-2004. Am J Epidemiol. 2008; 167:889–99.
Article11. Breen N, Scott S, Percy-Laurry A, Lewis D, Glasgow R. Health disparities calculator: a methodologically rigorous tool for analyzing inequalities in population health. Am J Public Health. 2014; 104:1589–91.
Article12. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000; 19:335–51.
Article13. Brenner H, Arndt V, Stegmaier C, Ziegler H, Rothenbacher D. Is Helicobacter pylori infection a necessary condition for noncardia gastric cancer? Am J Epidemiol. 2004; 159:252–8.14. Huerta-Franco MR, Banderas JW, Allsworth JE. Ethnic/racial differences in gastrointestinal symptoms and diagnosis associated with the risk of Helicobacter pylori infection in the US. Clin Exp Gastroenterol. 2018; 11:39–49.15. Taylor VM, Ko LK, Hwang JH, Sin MK, Inadomi JM. Gastric cancer in Asian American populations: a neglected health disparity. Asian Pac J Cancer Prev. 2014; 15:10565–71.
Article16. Jamal A, Homa DM, O'Connor E, Babb SD, Caraballo RS, Singh T, et al. Current cigarette smoking among adults: United States, 2005-2014. MMWR Morb Mortal Wkly Rep. 2015; 64:1233–40.17. Clarke TC, Ward BW, Schiller JS. Early release of selected estimates based on data from the January-March 2016 National Health Interview Survey. Atlanta, GA: Centers for Disease Control and Prevention;2016.18. Nagy P, Johansson S, Molloy-Bland M. Systematic review of time trends in the prevalence of Helicobacter pylori infection in China and the USA. Gut Pathog. 2016; 8:8.
Article19. Lagergren J, Lagergren P. Recent developments in esophageal adenocarcinoma. CA Cancer J Clin. 2013; 63:232–48.
Article20. Rustgi AK, El-Serag HB. Esophageal carcinoma. N Engl J Med. 2014; 371:2499–509.
Article21. Coleman HG, Xie SH, Lagergren J. The epidemiology of esophageal adenocarcinoma. Gastroenterology. 2018; 154:390–405.
Article22. Singh S, Sharma AN, Murad MH, Buttar NS, El-Serag HB, Katzka DA, et al. Central adiposity is associated with increased risk of esophageal inflammation, metaplasia, and adenocarcinoma: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2013; 11:1399–412.
Article23. Okosun IS, Choi ST, Boltri JM, Parish DC, Chandra KM, Dever GE, et al. Trends of abdominal adiposity in white, black, and Mexican-American adults, 1988 to 2000. Obes Res. 2003; 11:1010–7.
Article24. El-Serag HB, Petersen NJ, Carter J, Graham DY, Richardson P, Genta RM, et al. Gastroesophageal reflux among different racial groups in the United States. Gastroenterology. 2004; 126:1692–9.
Article25. Wen M, Kowaleski-Jones L, Fan JX. Ethnic-immigrant disparities in total and abdominal obesity in the US. Am J Health Behav. 2013; 37:807–18.
Article26. Petrick JL, Nguyen T, Cook MB. Temporal trends of esophageal disorders by age in the Cerner Health Facts database. Ann Epidemiol. 2016; 26:151–4.
Article27. Harper S, Lynch J. Selected comparisons of measures of health disparities: a review using databases relevant to healthy people 2010 cancer-related objectives. NCI Cancer Surveillance Monograph Series, No. 7. NIH Pub. No. 07-6281. Bethesda, MD: National Cancer Institute;2007.28. Healthy People 2020 [Internet]. Washington, DC: U.S: Department of Health and Human Services, Office of Disease Prevention and Health Promotion;2018. [cited 2018 May 1]. Available from: https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities.29. Kindig D. Population health equity: rate and burden, race and class. JAMA. 2017; 317:467–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Racial Differences in Prostate Cancer Characteristics and Cancer-Specific Mortality: An Overview
- Racial Differences in the Diagnosis and Treatment of Prostate Cancer
- Racial and ethnic disparities in metabolic dysfunction-associated steatotic liver disease outcomes: A call for culturally sensitive interventions: Editorial on “Differences in liver and mortality outcomes of non-alcoholic fatty liver disease by race and ethnicity: A longitudinal real-world study”
- Associations of racial and ethnic discrimination with adverse changes in exercise and screen time during the COVID-19 pandemic in the United States
- Preventable causes of cancer in Texas by race/ethnicity: tobacco smoking