Ann Hepatobiliary Pancreat Surg.
2019 Nov;23(4):365-371. 10.14701/ahbps.2019.23.4.365.
Subtype of intraductal papillary mucinous neoplasm of the pancreas is important to the development of metachronous high-risk lesions after pancreatectomy
- Affiliations
-
- 1Division of Hepatobiliary-Pancreatic Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University College of Medicine, Seoul, Korea. cardioman76@gmail.com
- 2Department of Pathology and Translational Genomics, Samsung Medical Center, Sungkyunkwan University College of Medicine, Seoul, Korea.
- KMID: 2464326
- DOI: http://doi.org/10.14701/ahbps.2019.23.4.365
Abstract
- BACKGROUNDS/AIMS
Although intraductal papillary mucinous neoplasm (IPMN) has showed a favorable prognosis compared to pancreatic ductal adenocarcinoma, its recurrence patterns have somewhat questionable in detail. After partial pancreatectomy for IPMN, the evaluation for risk of metachronous occurrence of high-risk lesions (HRL) in the residual pancreas is important to establish a postoperative surveillance modality and duration of follow-up. This study aimed to evaluate the factors that may predict the metachronous occurrence of HRL in the remnant pancreas after surgery of the IPMN.
METHODS
From 2005 to 2016, clinicopathologic and surveillance data for 346 consecutive patients who underwent surgical resection for IPMN were reviewed retrospectively. Histologic subtype was classified as gastric, intestinal, pancreato-biliary, or oncocytic type.
RESULTS
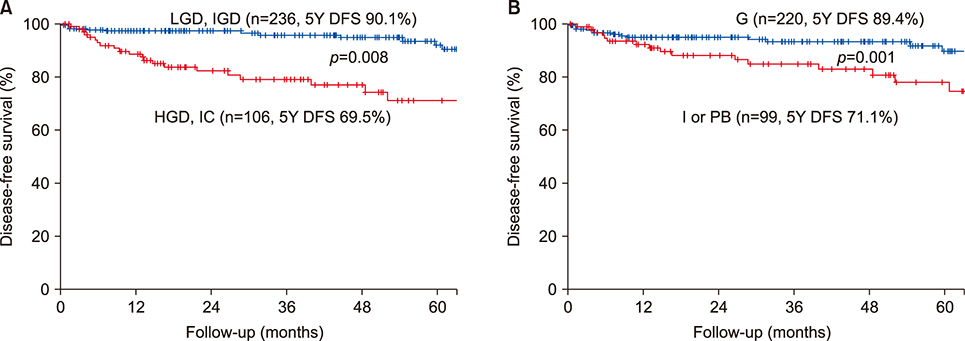
All of IPMN were classified as main duct (n=64, 18.5%), branch duct (n=171, 49.4%), and mixed type (n=111, 32.1%). Forty-eight patients (13.9%) experienced recurrence during follow-up. Among these, 9 patients (2.6%) were identified to metachronous development of HRL in the remnant pancreas. After multivariate analysis, high-grade dysplasia (HGD) or invasive carcinoma (IC) compared to low- or intermediate dysplasia was only independent risk factor for recurrence (HR 3.688, 95% CI 2.124- 12.524, p=0.009). The independent risk factors for metachronous development were HGD/IC (HR 8.414, 95% CI 4.310- 16.426, p=0.001), and intestinal/pancreato-biliary subtype compared to gastric subtype (HR 7.874, 95% CI 3.650- 27.027, p=0.010).
CONCLUSIONS
Patients with high-grade dysplasia or invasive carcinoma, and with intestinal or pancreatobiliary subtype should undergo close, long-term surveillance of the remnant pancreas after initial resection.
Keyword
MeSH Terms
Figure
Reference
-
1. Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, Shimizu M, et al. International Association of Pancreatology. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006; 6:17–32.2. Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, et al. International Association of Pancreatology. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012; 12:183–197.3. Vege SS, Ziring B, Jain R, Moayyedi P. Clinical Guidelines Committee. American Gastroenterology Association. American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015; 148:819–822. quiz e12-e13.4. Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017; 17:738–753.5. Kang MJ, Jang JY, Lee KB, Chang YR, Kwon W, Kim SW. Long-term prospective cohort study of patients undergoing pancreatectomy for intraductal papillary mucinous neoplasm of the pancreas: implications for postoperative surveillance. Ann Surg. 2014; 260:356–363.6. Hirono S, Kawai M, Okada K, Miyazawa M, Shimizu A, Kitahata Y, et al. Long-term surveillance is necessary after operative resection for intraductal papillary mucinous neoplasm of the pancreas. Surgery. 2016; 160:306–317.7. Date K, Ohtsuka T, Nakamura S, Mochidome N, Mori Y, Miyasaka Y, et al. Surveillance of patients with intraductal papillary mucinous neoplasm with and without pancreatectomy with special reference to the incidence of concomitant pancreatic ductal adenocarcinoma. Surgery. 2018; 163:291–299.8. Furukawa T, Hatori T, Fujita I, Yamamoto M, Kobayashi M, Ohike N, et al. Prognostic relevance of morphological types of intraductal papillary mucinous neoplasms of the pancreas. Gut. 2011; 60:509–516.9. Mino-Kenudson M, Fernández-del Castillo C, Baba Y, Valsangkar NP, Liss AS, Hsu M, et al. Prognosis of invasive intraductal papillary mucinous neoplasm depends on histological and precursor epithelial subtypes. Gut. 2011; 60:1712–1720.10. Ideno N, Ohtsuka T, Kono H, Fujiwara K, Oda Y, Aishima S, et al. Intraductal papillary mucinous neoplasms of the pancreas with distinct pancreatic ductal adenocarcinomas are frequently of gastric subtype. Ann Surg. 2013; 258:141–151.11. Miyasaka Y, Ohtsuka T, Tamura K, Mori Y, Shindo K, Yamada D, et al. Predictive factors for the metachronous development of high-risk lesions in the remnant pancreas after partial pancreatectomy for intraductal papillary mucinous neoplasm. Ann Surg. 2016; 263:1180–1187.12. Marchegiani G, Mino-Kenudson M, Ferrone CR, Morales-Oyarvide V, Warshaw AL, Lillemoe KD, et al. Patterns of recurrence after resection of ipmn: who, when, and how? Ann Surg. 2015; 262:1108–1114.13. He J, Cameron JL, Ahuja N, Makary MA, Hirose K, Choti MA, et al. Is it necessary to follow patients after resection of a benign pancreatic intraductal papillary mucinous neoplasm? J Am Coll Surg. 2013; 216:657–665.14. Niedergethmann M, Grützmann R, Hildenbrand R, Dittert D, Aramin N, Franz M, et al. Outcome of invasive and noninvasive intraductal papillary-mucinous neoplasms of the pancreas (IPMN): a 10-year experience. World J Surg. 2008; 32:2253–2260.15. Schmidt CM, White PB, Waters JA, Yiannoutsos CT, Cummings OW, Baker M, et al. Intraductal papillary mucinous neoplasms: predictors of malignant and invasive pathology. Ann Surg. 2007; 246:644–651. discussion 651-644.16. Fritz S, Schirren M, Klauss M, Bergmann F, Hackert T, Hartwig W, et al. Clinicopathologic characteristics of patients with resected multifocal intraductal papillary mucinous neoplasm of the pancreas. Surgery. 2012; 152(3 Suppl 1):S74–S80.17. Date K, Ohtsuka T, Fujimoto T, Tamura K, Kimura H, Matsunaga T, et al. Molecular evidence for monoclonal skip progression in main duct intraductal papillary mucinous neoplasms of the pancreas. Ann Surg. 2017; 265:969–977.18. Passot G, Lebeau R, Hervieu V, Ponchon T, Pilleul F, Adham M. Recurrences after surgical resection of intraductal papillary mucinous neoplasm of the pancreas: a single-center study of recurrence predictive factors. Pancreas. 2012; 41:137–141.19. Tanno S, Nakano Y, Koizumi K, Sugiyama Y, Nakamura K, Sasajima J, et al. Pancreatic ductal adenocarcinomas in long-term follow-up patients with branch duct intraductal papillary mucinous neoplasms. Pancreas. 2010; 39:36–40.20. Ikeuchi N, Itoi T, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, et al. Prognosis of cancer with branch duct type IPMN of the pancreas. World J Gastroenterol. 2010; 16:1890–1895.21. Sahora K, Ferrone CR, Brugge WR, Morales-Oyarvide V, Warshaw AL, Lillemoe KD, et al. Effects of comorbidities on outcomes of patients with intraductal papillary mucinous neoplasms. Clin Gastroenterol Hepatol. 2015; 13:1816–1823.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cystic Neoplasms and Intraductal Papillary Mucinous Neoplasms of the Pancreas
- Intraductal Papillary Mucinous Tumor Simultaneously Involving the Liver and Pancreas: A Case Report
- What are the Appropriate Surgery and Postoperative Surveillance for Intraductal Papillary Mucinous Neoplasm?
- Oncocytic Type Intraductal Papillary Mucinous Neoplasm Mimicking Mucinous Cystic Neoplasm of the Pancreas: A Case Report
- Comparison of Mucinous Cystic Tumor and Intraductal Papillary Mucinous Tumor