Korean J Orthod.
2019 Nov;49(6):413-426. 10.4041/kjod.2019.49.6.413.
Longitudinal management of recurrent temporomandibular joint ankylosis from infancy to adulthood in perspective of surgical and orthodontic treatment
- Affiliations
-
- 1Department of Orthodontics, Seoul National University Dental Hospital, Seoul, Korea.
- 2Department of Oral and Maxillofacial Surgery, School of Dentistry, Seoul National University, Seoul, Korea.
- 3Department of Orthodontics, School of Dentistry, Seoul National University, Seoul, Korea. drwhite@unitel.co.kr
- KMID: 2464204
- DOI: http://doi.org/10.4041/kjod.2019.49.6.413
Abstract
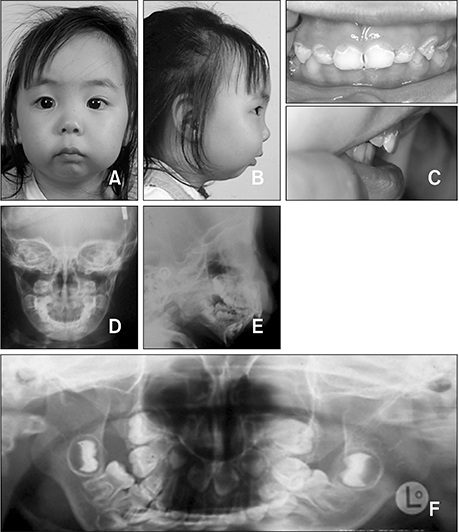
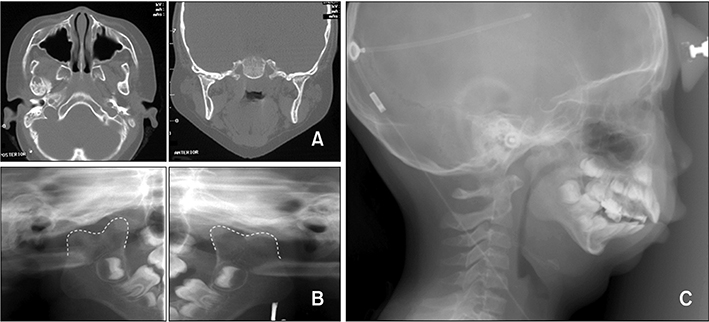
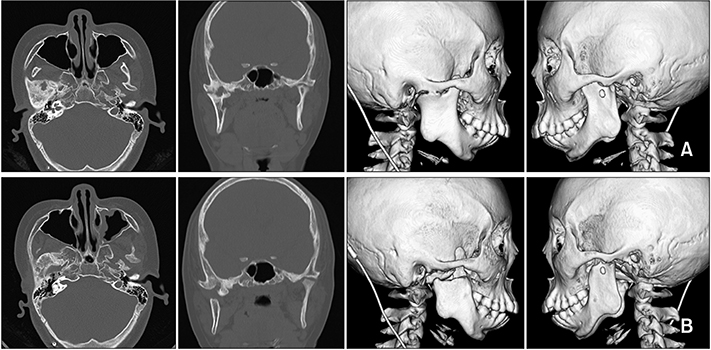
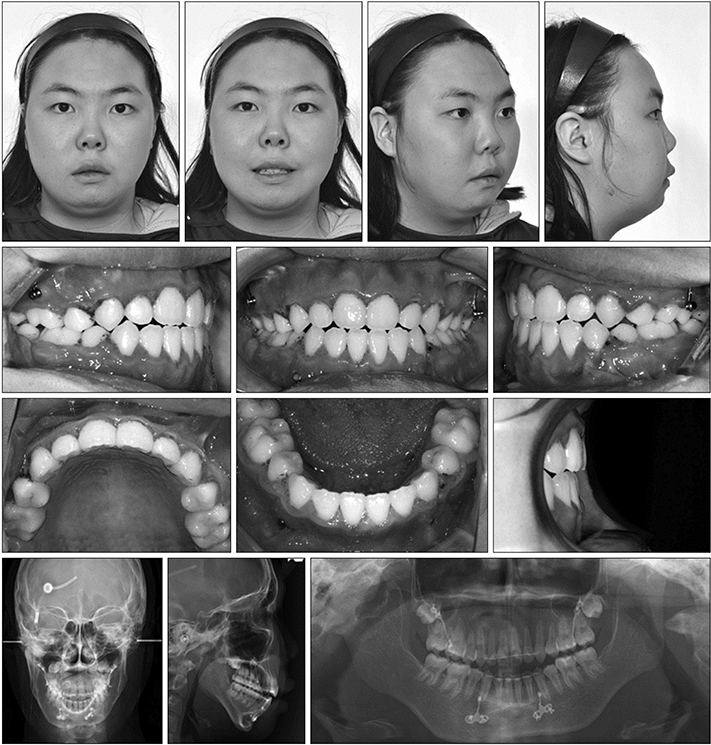
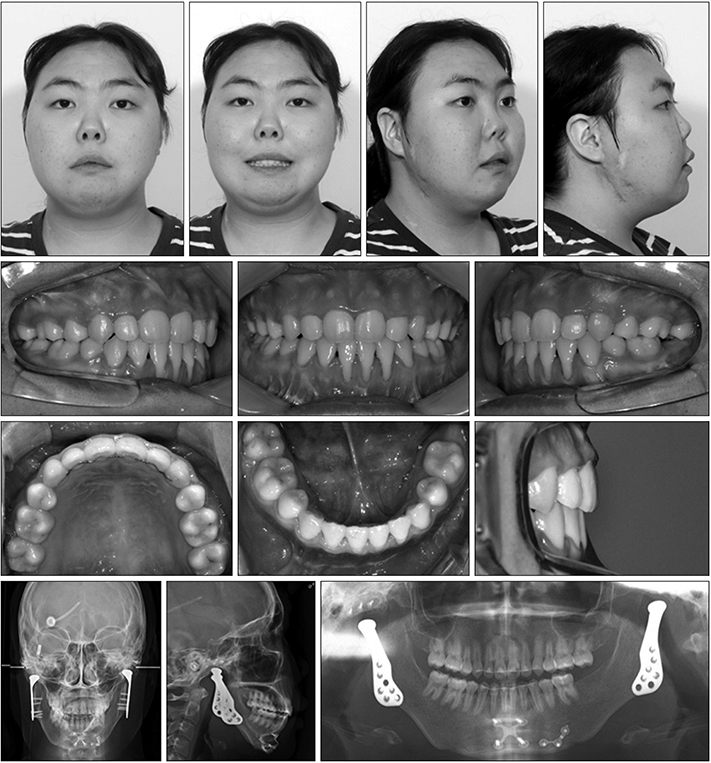
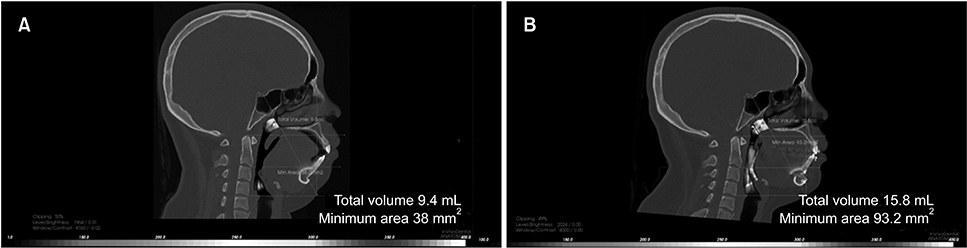
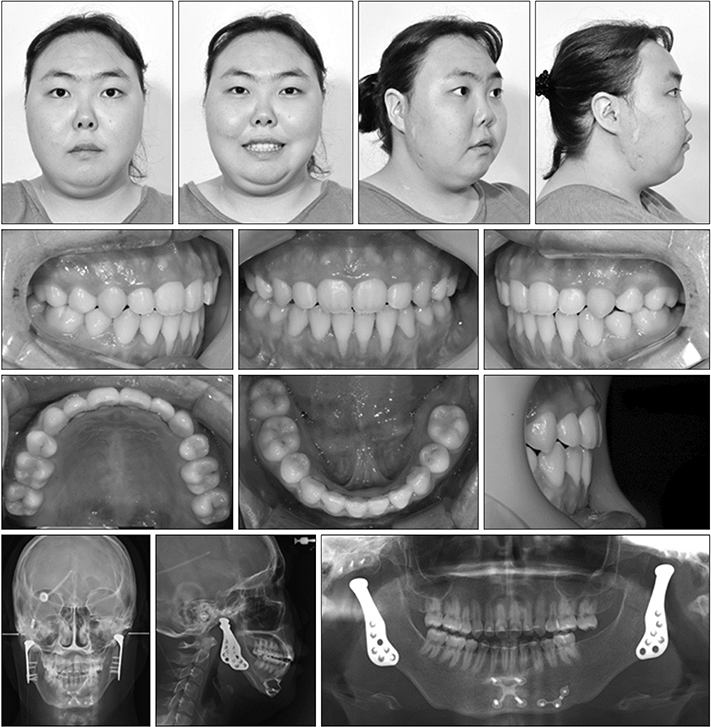
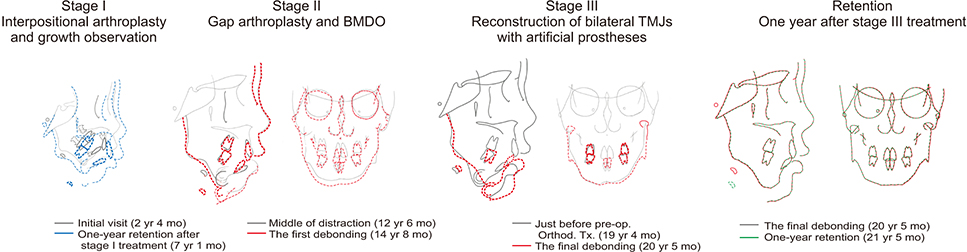
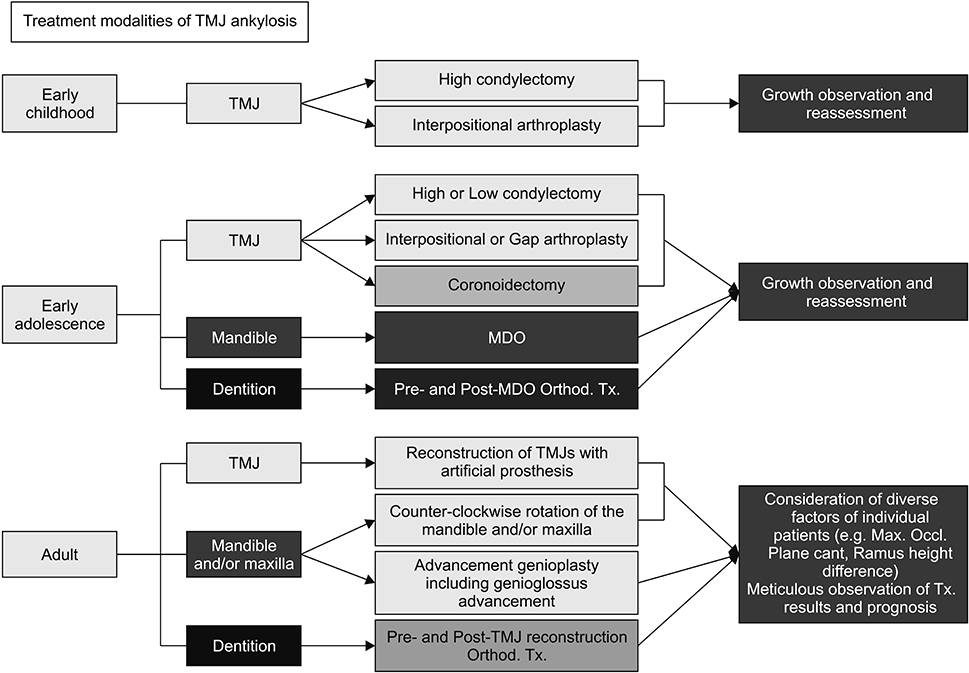
- This study was performed to describe the longitudinal management of recurrent temporomandibular joint (TMJ) ankylosis from infancy to adulthood in perspective of surgical and orthodontic treatment. A 2-year-old girl was referred with chief complaints of restricted mouth opening and micrognathia due to bilateral TMJ ankylosis. For stage I treatment during early childhood (6 years old), high condylectomy and interpositional arthroplasty were performed. However, TMJ ankylosis recurred and symptoms of obstructive sleep apnea (OSA) developed. For stage II treatment during early adolescence (12 years old), gap arthroplasty, coronoidectomy, bilateral mandibular distraction osteogenesis, and orthodontic treatment with extraction of the four first premolars were performed. However, TMJ ankylosis recurred. Because the OSA symptoms reappeared, she began to use a continuous positive airway pressure device. For stage III treatment after completion of growth (20 years old), low condylectomy, coronoidectomy, reconstruction of the bilateral TMJs with artificial prostheses along with counterclockwise rotational advancement of the mandible, genioglossus advancement, and orthodontic treatment were performed. After stage III treatment, the amount of mouth opening exhibited a significant increase. Mandibular advancement and ramus lengthening resulted in significant improvement in the facial profile, Class I relationships, and normal overbite/overjet. The OSA symptoms were also relieved. These outcomes were stable at the one-year follow-up visit. Since the treatment modalities for TMJ ankylosis differ according to the duration of ankylosis, patient age, and degree of deformity, the treatment flowchart suggested in this report could be used as an effective guideline for determining the appropriate timing and methods for the treatment of TMJ ankylosis.
Keyword
MeSH Terms
-
Adolescent
Ankylosis*
Arthroplasty
Bicuspid
Child, Preschool
Congenital Abnormalities
Continuous Positive Airway Pressure
Female
Follow-Up Studies
Humans
Mandible
Mandibular Advancement
Micrognathism
Mouth
Osteogenesis, Distraction
Prostheses and Implants
Sleep Apnea, Obstructive
Software Design
Temporomandibular Joint*
Figure
Reference
-
1. Kazanjian VH. Temporomandibular joint ankylosis with mandibular retrusion. Am J Surg. 1955; 90:905–910.
Article2. Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990; 48:1145–1151. discussion 1152.
Article3. Ko EW, Huang CS, Chen YR. Temporomandibular joint reconstruction in children using costochondral grafts. J Oral Maxillofac Surg. 1999; 57:789–798. discussion 799–800.
Article4. Kaban LB, Bouchard C, Troulis MJ. A protocol for management of temporomandibular joint ankylosis in children. J Oral Maxillofac Surg. 2009; 67:1966–1978.
Article5. Vasconcelos BC, Bessa-Nogueira RV, Cypriano RV. Treatment of temporomandibular joint ankylosis by gap arthroplasty. Med Oral Patol Oral Cir Bucal. 2006; 11:E66–E69.6. Topazian RG. Comparison of gap and interposition arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Surg. 1966; 24:405–409.7. Cheung LK, Lo J. The long-term effect of transport distraction in the management of temporomandibular joint ankylosis. Plast Reconstr Surg. 2007; 119:1003–1009.
Article8. Stucki-McCormick SU. Reconstruction of the mandibular condyle using transport distraction osteogenesis. J Craniofac Surg. 1997; 8:48–52. discussion 53.
Article9. López EN, Dogliotti PL. Treatment of temporomandibular joint ankylosis in children: is it necessary to perform mandibular distraction simultaneously? J Craniofac Surg. 2004; 15:879–884. discussion 884–5.
Article10. Peltomäki T. Growth of a costochondral graft in the rat temporomandibular joint. J Oral Maxillofac Surg. 1992; 50:851–857. discussion 857–8.
Article11. Henry CH, Wolford LM. Reconstruction of the temporomandibular joint using a temporalis graft with or without simultaneous orthognathic surgery. J Oral Maxillofac Surg. 1995; 53:1250–1256. discussion 1256–7.
Article12. van Loon JP, de Bont GM, Boering G. Evaluation of temporomandibular joint prostheses: review of the literature from 1946 to 1994 and implications for future prosthesis designs. J Oral Maxillofac Surg. 1995; 53:984–996. discussion 996–7.13. Wolford LM, Karras S, Mehra P. Concomitant temporomandibular joint and orthognathic surgery: a preliminary report. J Oral Maxillofac Surg. 2002; 60:356–362. discussion 362–3.
Article14. Coleta KE, Wolford LM, Gonçalves JR, Pinto Ados S, Cassano DS, Gonçalves DA. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint prostheses: part II--airway changes and stability. Int J Oral Maxillofac Surg. 2009; 38:228–235.
Article15. Yadav R, Bhutia O, Shukla G, Roychoudhury A. Distraction osteogenesis for management of obstructive sleep apnoea in temporomandibular joint ankylosis patients before the release of joint. J Craniomaxillofac Surg. 2014; 42:588–594.
Article16. Hägg U, Taranger J. Maturation indicators and the pubertal growth spurt. Am J Orthod. 1982; 82:299–309.
Article17. Dela Coleta KE, Wolford LM, Gonçalves JR, Pinto Ados S, Pinto LP, Cassano DS. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint prostheses: part I--skeletal and dental stability. Int J Oral Maxillofac Surg. 2009; 38:126–138.
Article18. Wolford LM, Cottrell DA, Henry CH. Temporomandibular joint reconstruction of the complex patient with the Techmedica custom-made total joint prosthesis. J Oral Maxillofac Surg. 1994; 52:2–10. discussion 11.
Article19. Wojczyńska A, Leiggener CS, Bredell M, Ettlin DA, Erni S, Gallo LM, et al. Alloplastic total temporomandibular joint replacements: do they perform like natural joints? Prospective cohort study with a historical control. Int J Oral Maxillofac Surg. 2016; 45:1213–1221.
Article20. Wolford LM, Mercuri LG, Schneiderman ED, Movahed R, Allen W. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ Concepts device. J Oral Maxillofac Surg. 2015; 73:952–960.
Article21. Mercuri LG, Giobbie-Hurder A. Long-term outcomes after total alloplastic temporomandibular joint reconstruction following exposure to failed materials. J Oral Maxillofac Surg. 2004; 62:1088–1096.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Difficult airway management in a case with lingual tonsil hypertrophy and temporo-mandibular joint partial ankylosis
- The sequential management of recurrent temporomandibular joint ankylosis in a growing child: a case report
- Temporomandibular joint re-ankylosis: a case report and literature review
- Airway Management for General Anesthesia in a Patient with Severe Trismus due to Temporomandibular Joint Ankylosis : A case report
- Treatment of Temporomandibular Joint Reankylosis by Submandibular Anchorage Technique with Temporalis Myofascial Flap