Korean J Orthod.
2019 Nov;49(6):360-371. 10.4041/kjod.2019.49.6.360.
Predictors of midpalatal suture expansion by miniscrew-assisted rapid palatal expansion in young adults: A preliminary study
- Affiliations
-
- 1Department of Orthodontics, College of Dentistry, Yonsei University, Seoul, Korea. yumichael@yuhs.ac
- 2Institute of Craniofacial Deformity, College of Dentistry, Yonsei University, Seoul, Korea.
- 3Department of Oral and Maxillofacial Radiology, College of Dentistry, Yonsei University, Seoul, Korea.
- KMID: 2464199
- DOI: http://doi.org/10.4041/kjod.2019.49.6.360
Abstract
OBJECTIVE
We sought to determine the predictors of midpalatal suture expansion by miniscrew-assisted rapid palatal expansion (MARPE) in young adults.
METHODS
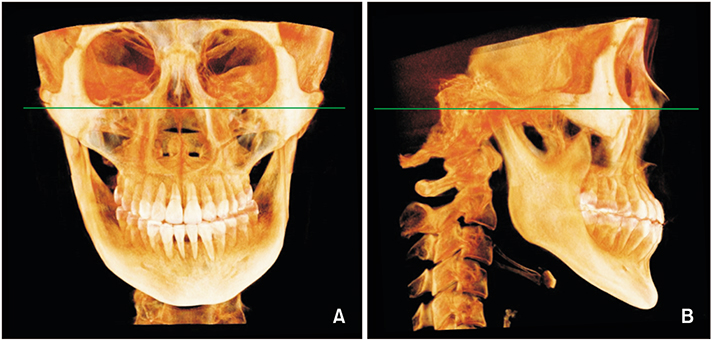
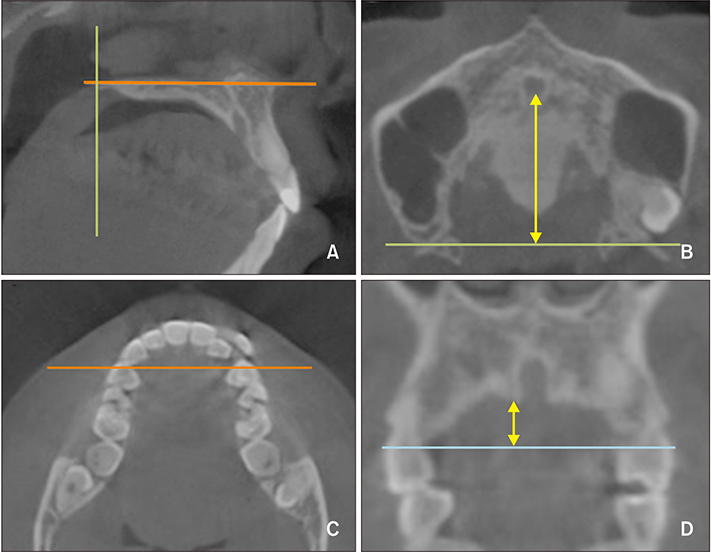
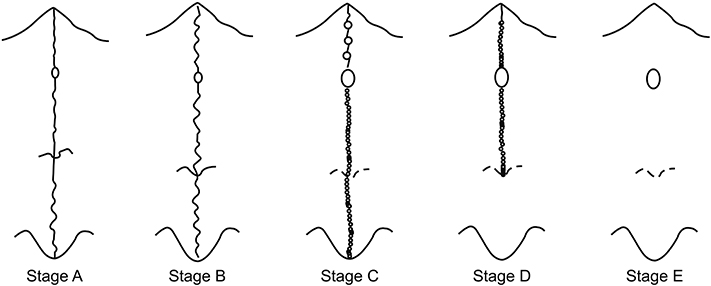
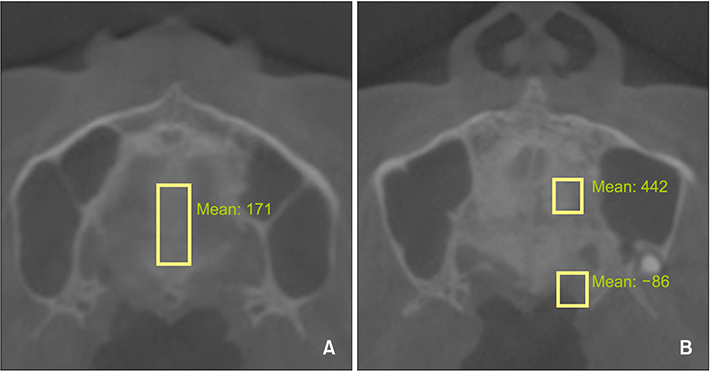
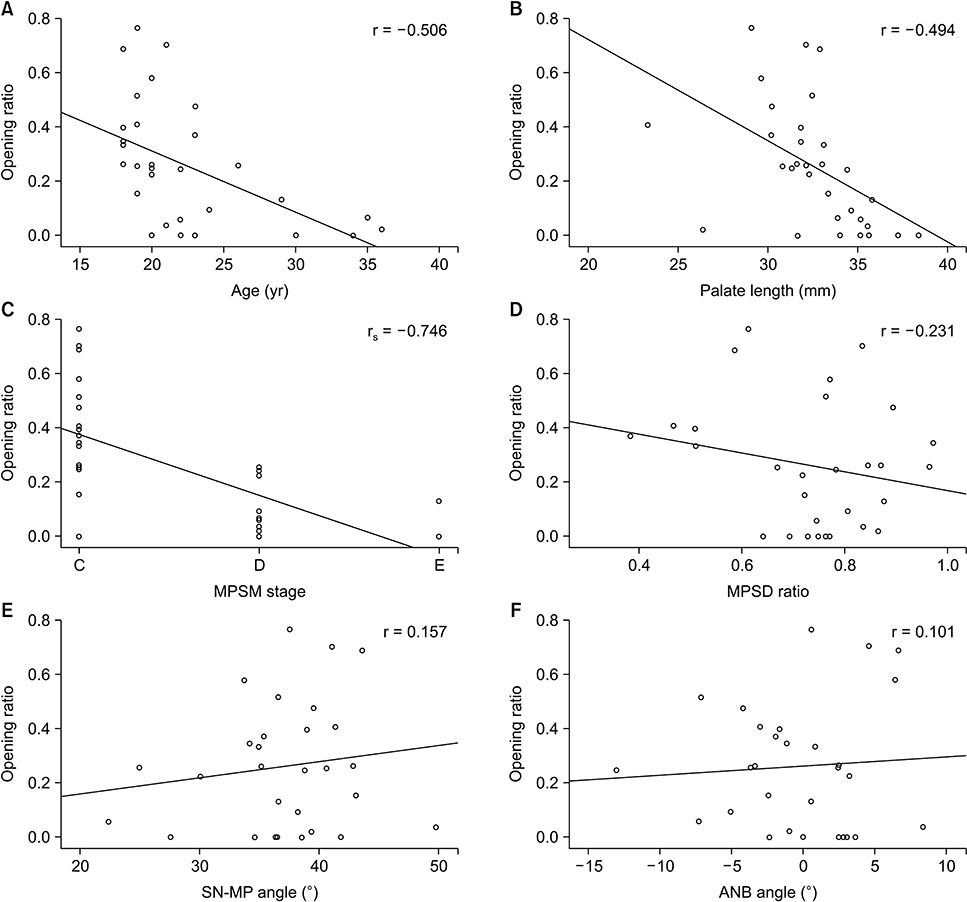
The following variables were selected as possible predictors: chronological age, palate length and depth, midpalatal suture maturation (MPSM) stage, midpalatal suture density (MPSD) ratio, the sella-nasion (SN)-mandibular plane (MP) angle as an indicator of the vertical skeletal pattern, and the point A-nasion-point B (ANB) angle for anteroposterior skeletal classification. For 31 patients (mean age, 22.52 years) who underwent MARPE treatment, palate length and depth, MPSM stage and MPSD ratio from the initial cone-beam computed tomography images, and the SN-MP angle and ANB angle from lateral cephalograms were assessed. The midpalatal suture opening ratio was calculated from the midpalatal suture opening width measured in periapical radiographs and the MARPE screw expansion. Statistical analyses of correlations were performed for the entire patient group of 31 subjects and subgroups categorized by sex, vertical skeletal pattern, and anteroposterior skeletal classification.
RESULTS
In the entire patient group, the midpalatal suture opening ratio showed statistically significant negative correlations with age, palate length, and MPSM stage (r = −0.506, −0.494, and −0.746, respectively, all p < 0.01). In subgroup analyses, a strong negative correlation was observed with the palate depth in the skeletal Class II subgroup (r = −0.900, p < 0.05).
CONCLUSIONS
The findings of this study indicated that age, palate length, and MPSM stage can be predictors of midpalatal suture expansion by MARPE in young adults.
Figure
Cited by 2 articles
-
Stability of bimaxillary surgery involving intraoral vertical ramus osteotomy with or without presurgical miniscrew-assisted rapid palatal expansion in adult patients with skeletal Class III malocclusion
Yoon-Soo Ahn, Sung-Hwan Choi, Kee-Joon Lee, Young-Soo Jung, Hyoung-Seon Baik, Hyung-Seog Yu
Korean J Orthod. 2020;50(5):304-313. doi: 10.4041/kjod.2020.50.5.304.Effectiveness of miniscrew assisted rapid palatal expansion using cone beam computed tomography: A systematic review and meta-analysis
Patchaya Siddhisaributr, Kornkanok Khlongwanitchakul, Niwat Anuwongnukroh, Somchai Manopatanakul, Nita Viwattanatipa
Korean J Orthod. 2022;52(3):182-200. doi: 10.4041/kjod21.256.
Reference
-
1. Lee KJ, Park YC, Park JY, Hwang WS. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop. 2010; 137:830–839.
Article2. Park JJ, Park YC, Lee KJ, Cha JY, Tahk JH, Choi YJ. Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: a cone-beam computed tomography study. Korean J Orthod. 2017; 47:77–86.
Article3. Jain V, Shyagali TR, Kambalyal P, Rajpara Y, Doshi J. Comparison and evaluation of stresses generated by rapid maxillary expansion and the implant-supported rapid maxillary expansion on the craniofacial structures using finite element method of stress analysis. Prog Orthod. 2017; 18:3.
Article4. Handelman CS, Wang L, BeGole EA, Haas AJ. Nonsurgical rapid maxillary expansion in adults: report on 47 cases using the Haas expander. Angle Orthod. 2000; 70:129–144.5. Işeri H, Ozsoy S. Semirapid maxillary expansion--a study of long-term transverse effects in older adolescents and adults. Angle Orthod. 2004; 74:71–78.6. Cunha ACD, Lee H, Nojima LI, Nojima MDCG, Lee KJ. Miniscrew-assisted rapid palatal expansion for managing arch perimeter in an adult patient. Dental Press J Orthod. 2017; 22:97–108.
Article7. Gautam P, Valiathan A, Adhikari R. Stress and displacement patterns in the craniofacial skeleton with rapid maxillary expansion: a finite element method study. Am J Orthod Dentofacial Orthop. 2007; 132:5.e1–5.e11.
Article8. Priyadarshini J, Mahesh CM, Chandrashekar BS, Sundara A, Arun AV, Reddy VP. Stress and displacement patterns in the craniofacial skeleton with rapid maxillary expansion-a finite element method study. Prog Orthod. 2017; 18:17.
Article9. Knaup B, Yildizhan F, Wehrbein H. Age-related changes in the midpalatal suture. A histomorphometric study. J Orofac Orthop. 2004; 65:467–474.10. Wehrbein H, Yildizhan F. The mid-palatal suture in young adults. A radiological-histological investigation. Eur J Orthod. 2001; 23:105–114.
Article11. Kokich VG. Age changes in the human frontozygomatic suture from 20 to 95 years. Am J Orthod. 1976; 69:411–430.
Article12. Bishara SE, Staley RN. Maxillary expansion: clinical implications. Am J Orthod Dentofacial Orthop. 1987; 91:3–14.
Article13. Mossaz CF, Byloff FK, Richter M. Unilateral and bilateral corticotomies for correction of maxillary transverse discrepancies. Eur J Orthod. 1992; 14:110–116.
Article14. Timms DJ, Vero D. The relationship of rapid maxillary expansion to surgery with special reference to midpalatal synostosis. Br J Oral Surg. 1981; 19:180–196.
Article15. Korbmacher H, Schilling A, Püschel K, Amling M, Kahl-Nieke B. Age-dependent three-dimensional microcomputed tomography analysis of the human midpalatal suture. J Orofac Orthop. 2007; 68:364–376.
Article16. Matsuyama Y, Motoyoshi M, Tsurumachi N, Shimizu N. Effects of palate depth, modified arm shape, and anchor screw on rapid maxillary expansion: a finite element analysis. Eur J Orthod. 2015; 37:188–193.
Article17. Parcha E, Bitsanis E, Halazonetis DJ. Morphometric covariation between palatal shape and skeletal pattern in children and adolescents: a cross-sectional study. Eur J Orthod. 2017; 39:377–385.
Article18. Forster CM, Sunga E, Chung CH. Relationship between dental arch width and vertical facial morphology in untreated adults. Eur J Orthod. 2008; 30:288–294.
Article19. Franchi L, Baccetti T. Transverse maxillary deficiency in Class II and Class III malocclusions: a cephalometric and morphometric study on postero-anterior films. Orthod Craniofac Res. 2005; 8:21–28.
Article20. Angelieri F, Cevidanes LH, Franchi L, Gonçalves JR, Benavides E, McNamara JA Jr. Midpalatal suture maturation: classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2013; 144:759–769.
Article21. Grünheid T, Larson CE, Larson BE. Midpalatal suture density ratio: a novel predictor of skeletal response to rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2017; 151:267–276.
Article22. Riedel RA. The relation of maxillary structures to cranium in malocclusion and in normal occlusion. Angle Orthod. 1952; 22:142–145.23. Schudy FF. The rotation of the mandible resulting from growth: its implications in orthodontic treatment. Angle Orthod. 1965; 35:36–50.24. Persson M, Thilander B. Palatal suture closure in man from 15 to 35 years of age. Am J Orthod. 1977; 72:42–52.
Article25. Melsen B, Melsen F. The postnatal development of the palatomaxillary region studied on human autopsy material. Am J Orthod. 1982; 82:329–342.
Article26. Ladewig VM, Capelozza-Filho L, Almeida-Pedrin RR, Guedes FP, de Almeida Cardoso M, de Castro Ferreira Conti AC. Tomographic evaluation of the maturation stage of the midpalatal suture in postadolescents. Am J Orthod Dentofacial Orthop. 2018; 153:818–824.
Article27. Barbosa NMV, Castro AC, Conti F, Capelozza-Filho L, Almeida-Pedrin RR, Cardoso MA. Reliability and reproducibility of the method of assessment of midpalatal suture maturation: a tomographic study. Angle Orthod. 2019; 89:71–77.
Article28. Isaacson RJ, Wood JL, Ingram AH. Forces produced by rapid maxillary expansion. Angle Orthod. 1964; 34:256–260.29. Isaacson RJ, Ingram AH. Forces produced by rapid maxillary expansion. Angle Orthod. 1964; 34:261–270.30. Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Müller R. Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res. 2010; 25:1468–1486.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: A cone-beam computed tomography study
- Nonsurgical maxillary expansion in a 60-year-old patient with gingival recession and crowding
- Effectiveness of miniscrew assisted rapid palatal expansion using cone beam computed tomography: A systematic review and meta-analysis
- A posteroanterior cephalometric study on the change of maxilla by rapid palatal expansion
- A comparative experimental study on gross reactions of surounding maxillary sutures to the widening of midpalatal suture in young and adult dog