Ann Rehabil Med.
2019 Oct;43(5):570-580. 10.5535/arm.2019.43.5.570.
Post-operative Physical Performance Factors Associated With Gait Speed in Patients Surgically Treated for Hip Fracture: A Cross-Sectional Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Jeju National University College of Medicine–Regional Rheumatoid and Degenerative Arthritis Center, Jeju National University Hospital, Jeju, Korea. brkim08@jejunu.ac.kr
- 2Department of Orthopaedic Surgery, Jeju National University College of Medicine–Regional Rheumatoid and Degenerative Arthritis Center, Jeju National University Hospital, Jeju, Korea.
- KMID: 2463705
- DOI: http://doi.org/10.5535/arm.2019.43.5.570
Abstract
OBJECTIVE
To determine post-operative physical performance factors associated with gait speed in patients surgically treated for hip fracture.
METHODS
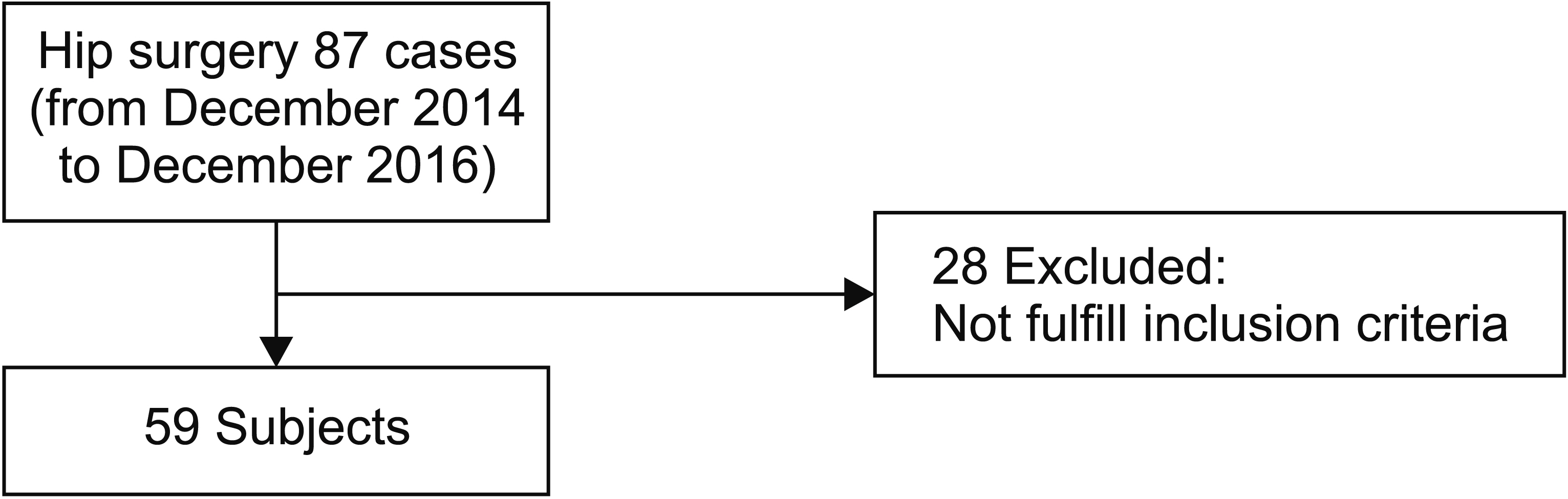
Cross-sectional data from 59 patients (16 males and 43 females; mean age, 79.2±9.1 years) who underwent hip fracture surgery were enrolled. Patients completed a 10-meter walk test (10MWT) to assess gait speed. Additional physical performance tests included the Timed Up and Go test (TUG), the Berg Balance Scale (BBS), maximum voluntary isometric contraction (MVIC) of the knee extensors and flexors on the operated and non-operated sides as well as of the hip abductors (all tested using air-resistance weight machines), and analysis of spatio-temporal gait parameters at about 6 weeks after hip surgery.
RESULTS
Bivariate analyses revealed a significant positive correlation between the post-operative 10MWT and the post-operative TUG, age, swing phase duration, and gait cycle duration along with a significant negative correlation between post-operative BBS score, MVIC of the knee extensors and flexors on the operated and non-operated sides, MVIC of the hip abductors, and cadence and stance phase duration. Linear regression analyses revealed that the post-operative TUG (β=0.85, p<0.01), gait cycle duration (β=0.17, p=0.02), and osteoporosis (β=-0.18, p=0.02) were associated with the post-operative 10MWT.
CONCLUSION
The presence of osteoporosis, post-operative balance, and isometric muscle strength in the operated and non-operated legs were statistically associated with post-operative gait speed early after hip fracture surgery.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Association of Nutritional Risk With Gait Function and Activities of Daily Living in Older Adult Patients With Hip Fractures
Yasunobu Ishikawa, Takuji Adachi, Yasushi Uchiyama
Ann Rehabil Med. 2024;48(2):115-123. doi: 10.5535/arm.230015.
Reference
-
1. World Health Organization. Osteoporosis: both health organizations and individuals must act now to avoid an impending epidemic. Geneva: World Health Organization;1999.2. Choi ES, Shon HC, Kim YM, Kim DS, Park KJ, Lim CO, et al. Is the incidence rate of hip fractures still increasing in Korea? An epidemiologic study based on National Health Insurance Database. J Korean Orthop Assoc. 2016; 51:447–54.
Article3. Gialanella B, Ferlucci C, Monguzzi V, Prometti P. Determinants of functional outcome in hip fracture patients: the role of specific neuropsychiatric symptoms. Disabil Rehabil. 2015; 37:517–22.
Article4. Jette AM, Harris BA, Cleary PD, Campion EW. Functional recovery after hip fracture. Arch Phys Med Rehabil. 1987; 68:735–40.5. Mossey JM, Mutran E, Knott K, Craik R. Determinants of recovery 12 months after hip fracture: the importance of psychosocial factors. Am J Public Health. 1989; 79:279–86.
Article6. Young Y, Brant L, German P, Kenzora J, Magaziner J. A longitudinal examination of functional recovery among older people with subcapital hip fractures. J Am Geriatr Soc. 1997; 45:288–94.
Article7. Ingemarsson AH, Frandin K, Mellstrom D, Moller M. Walking ability and activity level after hip fracture in the elderly: a follow-up. J Rehabil Med. 2003; 35:76–83.8. Whitehead C, Miller M, Crotty M. Falls in communitydwelling older persons followinig hip fracture: impact on self-efficacy, balance and handicap. Clin Rehabil. 2003; 17:899–906.9. van den Akker-Scheek I, Stevens M, Bulstra SK, Groothoff JW, van Horn JR, Zijlstra W. Recovery of gait after short-stay total hip arthroplasty. Arch Phys Med Rehabil. 2007; 88:361–7.
Article10. Hodt-Billington C, Helbostad JL, Vervaat W, Rognsvag T, Moe-Nilssen R. Changes in gait symmetry, gait velocity and self-reported function following total hip replacement. J Rehabil Med. 2011; 43:787–93.
Article11. Coulter CL, Scarvell JM, Neeman TM, Smith PN. Physiotherapist-directed rehabilitation exercises in the outpatient or home setting improve strength, gait speed and cadence after elective total hip replacement: a systematic review. J Physiother. 2013; 59:219–26.
Article12. Kolk S, Minten MJ, van Bon GE, Rijnen WH, Geurts AC, Verdonschot N, et al. Gait and gait-related activities of daily living after total hip arthroplasty: a systematic review. Clin Biomech (Bristol, Avon). 2014; 29:705–18.
Article13. Lamoureux EL, Sparrow WA, Murphy A, Newton RU. The relationship between lower body strength and obstructed gait in community-dwelling older adults. J Am Geriatr Soc. 2002; 50:468–73.
Article14. Roy MA, Doherty TJ. Reliability of hand-held dynamometry in assessment of knee extensor strength after hip fracture. Am J Phys Med Rehabil. 2004; 83:813–8.
Article15. Lamb SE, Morse RE, Evans JG. Mobility after proximal femoral fracture: the relevance of leg extensor power, postural sway and other factors. Age Ageing. 1995; 24:308–14.
Article16. Madsen OR, Lauridsen UB, Sorensen OH. Quadriceps strength in women with a previous hip fracture: relationships to physical ability and bone mass. Scand J Rehabil Med. 2000; 32:37–40.17. Kang JH, Lee G, Kim KE, Lee YK, Lim JY. Determinants of functional outcomes using clinical pathways for rehabilitation after hip fracture surgery. Ann Geriatr Med Res. 2018; 22:26–32.
Article18. Freter SH, Fruchter N. Relationship between timed ‘up and go’ and gait time in an elderly orthopaedic rehabilitation population. Clin Rehabil. 2000; 14:96–101.
Article19. Jung HY, Park JH, Shim JJ, Kim MJ, Hwang MR, Kim SH. Reliability test of Korean version of berg balance scale. J Korean Acad Rehabil Med. 2006; 30:611–8.20. Bugane F, Benedetti MG, Casadio G, Attala S, Biagi F, Manca M, et al. Estimation of spatial-temporal gait parameters in level walking based on a single accelerometer: validation on normal subjects by standard gait analysis. Comput Methods Programs Biomed. 2012; 108:129–37.21. Thingstad P, Egerton T, Ihlen EF, Taraldsen K, Moe-Nilssen R, Helbostad JL. Identification of gait domains and key gait variables following hip fracture. BMC Geriatr. 2015; 15:150.
Article22. Morri M, Natali E, Tosarelli D. At discharge gait speed and independence of patients provides a challenges for rehabilitation after total joint arthroplasty: an observational study. Arch Physiother. 2016; 6:6.
Article23. Lord S, Galna B, Rochester L. Moving forward on gait measurement: toward a more refined approach. Mov Disord. 2013; 28:1534–43.
Article24. Kline Mangione K, Craik RL, Lopopolo R, Tomlinson JD, Brenneman SK. Predictors of gait speed in patients after hip fracture. Physiother Can. 2008; 60:10–8.
Article25. Gausden EB, Sin D, Levack AE, Wessel LE, Moloney G, Lane JM, et al. Gait analysis after intertrochanteric hip fracture: does shortening result in gait impairment? J Orthop Trauma. 2018; 32:554–8.
Article26. Tinetti ME, Baker DI, Gottschalk M, Williams CS, Pollack D, Garrett P, et al. Home-based multicomponent rehabilitation program for older persons after hip fracture: a randomized trial. Arch Phys Med Rehabil. 1999; 80:916–22.
Article27. Leiper CI, Craik RL. Relationships between physical activity and temporal-distance characteristics of walking in elderly women. Phys Ther. 1991; 71:791–803.
Article28. Blanke DJ, Hageman PA. Comparison of gait of young men and elderly men. Phys Ther. 1989; 69:144–8.
Article29. Brach JS, VanSwearingen JM. Physical impairment and disability: relationship to performance of activities of daily living in community-dwelling older men. Phys Ther. 2002; 82:752–61.
Article30. Bohannon RW. Reference values for extremity muscle strength obtained by hand-held dynamometry from adults aged 20 to 79 years. Arch Phys Med Rehabil. 1997; 78:26–32.
Article31. Woodward LM, Clemson L, Moseley AM, Lord SR, Cameron ID, Sherrington C. Most functional outcomes are similar for men and women after hip fracture: a secondary analysis of the enhancing mobility after hip fracture trial. BMC Geriatr. 2014; 14:140.
Article32. Nankaku M, Tsuboyama T, Kakinoki R, Akiyama H, Nakamura T. Prediction of ambulation ability following total hip arthroplasty. J Orthop Sci. 2011; 16:359–63.
Article33. Radosavljevic N, Nikolic D, Lazovic M, Petronic I, Milicevic V, Radosavljevic Z, et al. Estimation of functional recovery in patients after hip fracture by Berg Balance Scale regarding the sex, age and comorbidity of participants. Geriatr Gerontol Int. 2013; 13:365–71.
Article34. Leijendekkers RA, Marra MA, Kolk S, van Bon G, Schreurs BW, Weerdesteyn V, et al. Gait symmetry and hip strength in women with developmental dysplasia following hip arthroplasty compared to healthy subjects: a cross-sectional study. PLoS One. 2018; 13:e0193487.
Article35. Kubota M, Uchida K, Kokubo Y, Shimada S, Matsuo H, Yayama T, et al. Changes in gait pattern and hip muscle strength after open reduction and internal fixation of acetabular fracture. Arch Phys Med Rehabil. 2012; 93:2015–21.
Article36. Portegijs E, Sipila S, Rantanen T, Lamb SE. Leg extension power deficit and mobility limitation in women recovering from hip fracture. Am J Phys Med Rehabil. 2008; 87:363–70.
Article37. Lindsey C, Brownbill RA, Bohannon RA, Ilich JZ. Association of physical performance measures with bone mineral density in postmenopausal women. Arch Phys Med Rehabil. 2005; 86:1102–7.
Article38. Dostanpor A, Dobson CA, Vanicek N. Relationships between walking speed, T-score and age with gait parameters in older post-menopausal women with low bone mineral density. Gait Posture. 2018; 64:230–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors of Postoperative Delirium in Elderly Patients with Hip Fractures
- Optimal Cut-Off Points of 4-meter Gait Speed to Discriminate Functional Exercise Capacity and Health Status in Older patients with Chronic Obstructive Pulmonary Disease
- Usefulness of Psoas Muscle Cross-Sectional Area in Evaluating Physical Performance in Patients with Liver Cirrhosis
- Osteonecrosis of the Femoral Head in the Setting of a Complex Acetabulum Fracture without Hip Dislocation Treated Surgically Using Ilio-inguinal Approach: A Case Report
- Femoral Nerve Block (Motor Branch of Rectus Femoris) for Stiff-legged Gait in Spastic Patients