Ann Rehabil Med.
2019 Oct;43(5):535-543. 10.5535/arm.2019.43.5.535.
Effect of Decreased Skeletal Muscle Index and Hand Grip Strength on Functional Recovery in Subacute Ambulatory Stroke Patients
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Dong-A University College of Medicine, Busan, Korea. dry815@hanmail.net
- 2Regional Cardiocerebrovascular Center, Dong-A Medical Center, Busan, Korea.
- KMID: 2463701
- DOI: http://doi.org/10.5535/arm.2019.43.5.535
Abstract
OBJECTIVE
To investigate the effect of decreased Skeletal Muscle Index (SMI) and hand grip strength on functional recovery in subacute ambulatory stroke patients.
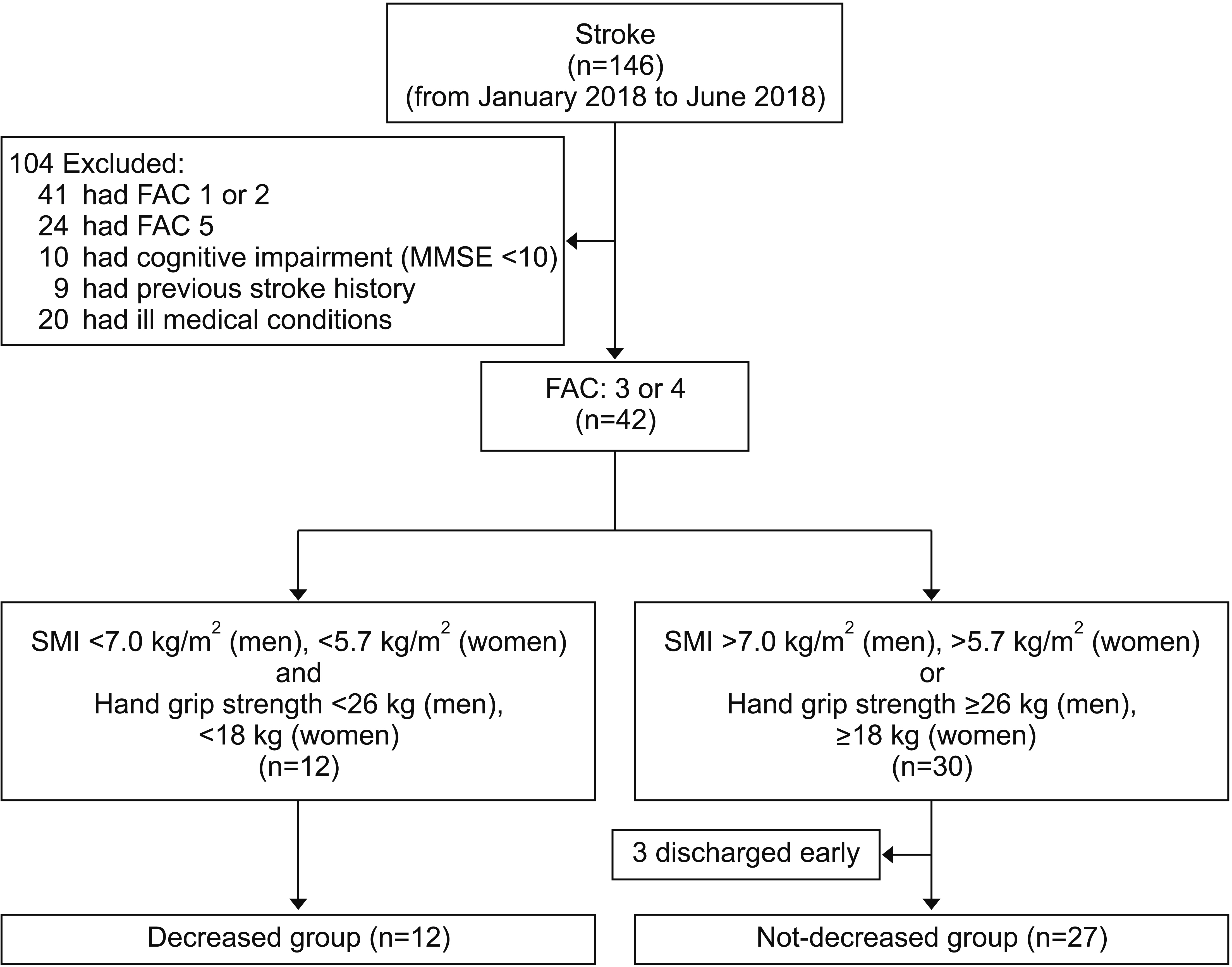
METHODS
Subacute stroke patients who were referred to the rehabilitation center were recruited. Decreased SMI and hand grip strength were diagnosed according to the Asian Working Group on Sarcopenia. Diagnostic criteria were decreased SMI and decreased unaffected hand grip strength. SMI was measured by bioelectrical impedance analysis. Unaffected hand grip strength was measured with a hand dynamometer. Patients were divided into two groups, decreased group (DG) and not-decreased group (NDG), according to the presence of decreased SMI and hand grip strength. Both groups received conventional stroke rehabilitation for 3 weeks. All patients were evaluated at the baseline and at 3 weeks after treatment. Functional status was evaluated with 4-meter walk test (4MWT), 6-minute walk test (6MWT), Timed Up and Go test (TUG), and Modified Barthel Index (MBI).
RESULTS
Both groups showed improvement in 4MWT, TUG, and MBI. NDG showed improvement in 6MWT. Comparing improvements between the two groups, NDG showed more improvement in 6MWT and TUG than DG.
CONCLUSION
The presence of decreased SMI and hand grip strength had negative effects on functional recovery in subacute ambulatory stroke patients.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Path to Precision Medicine: Incorporating Blood-Based Biomarkers in Stroke Rehabilitation
Byung-Mo Oh
Ann Rehabil Med. 2021;45(5):341-344. doi: 10.5535/arm.21171.
Reference
-
1. Rosenberg IH. Summary comments: epidemiological and methodological problems in determining nutritional status of older persons. Am J Clin Nutr. 1989; 50:1231–33.2. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010; 39:412–23.
Article3. Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. J Am Med Dir Assoc. 2011; 12:249–56.4. Morley JE, Abbatecola AM, Argiles JM, Baracos V, Bauer J, Bhasin S, et al. Sarcopenia with limited mobility: an international consensus. J Am Med Dir Assoc. 2011; 12:403–9.
Article5. Cawthon PM, Peters KW, Shardell MD, McLean RR, Dam TT, Kenny AM, et al. Cutpoints for low appendicular lean mass that identify older adults with clinically significant weakness. J Gerontol A Biol Sci Med Sci. 2014; 69:567–75.
Article6. Dos Santos L, Cyrino ES, Antunes M, Santos DA, Sardinha LB. Sarcopenia and physical independence in older adults: the independent and synergic role of muscle mass and muscle function. J Cachexia Sarcopenia Muscle. 2017; 8:245–50.
Article7. Steffl M, Bohannon RW, Sontakova L, Tufano JJ, Shiells K, Holmerova I. Relationship between sarcopenia and physical activity in older people: a systematic review and meta-analysis. Clin Interv Aging. 2017; 12:835–45.
Article8. Cruz-Jentoft AJ, Landi F, Schneider SM, Zuniga C, Arai H, Boirie Y, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014; 43:748–59.
Article9. Han P, Kang L, Guo Q, Wang J, Zhang W, Shen S, et al. Prevalence and factors associated with sarcopenia in suburb-dwelling older Chinese using the Asian working group for sarcopenia definition. J Gerontol A Biol Sci Med Sci. 2016; 71:529–35.
Article10. Melton LJ 3rd, Khosla S, Crowson CS, O’Connor MK, O’Fallon WM, Riggs BL. Epidemiology of sarcopenia. J Am Geriatr Soc. 2000; 48:625–30.
Article11. Tay L, Ding YY, Leung BP, Ismail NH, Yeo A, Yew S, et al. Sex-specific differences in risk factors for sarcopenia amongst community-dwelling older adults. Age (Dordr). 2015; 37:121.
Article12. Figueiredo CP, Domiciano DS, Lopes JB, Caparbo VF, Scazufca M, Bonfa E, et al. Prevalence of sarcopenia and associated risk factors by two diagnostic criteria in community-dwelling older men: the São Paulo Ageing & Health Study (SPAH). Osteoporos Int. 2014; 25:589–96.13. Bianchi L, Abete P, Bellelli G, Bo M, Cherubini A, Corica F, et al. Prevalence and clinical correlates of sarcopenia, identified according to the EWGSOP definition and diagnostic algorithm, in hospitalized older people: the GLISTEN study. J Gerontol A Biol Sci Med Sci. 2017; 72:1575–81.
Article14. Senior HE, Henwood TR, Beller EM, Mitchell GK, Keogh JW. Prevalence and risk factors of sarcopenia among adults living in nursing homes. Maturitas. 2015; 82:418–23.
Article15. Ovbiagele B, Nguyen-Huynh MN. Stroke epidemiology: advancing our understanding of disease mechanism and therapy. Neurotherapeutics. 2011; 8:319–29.
Article16. Scherbakov N, Sandek A, Doehner W. Stroke-related sarcopenia: specific characteristics. J Am Med Dir Assoc. 2015; 16:272–6.
Article17. Hunnicutt JL, Gregory CM. Skeletal muscle changes following stroke: a systematic review and comparison to healthy individuals. Top Stroke Rehabil. 2017; 24:463–71.
Article18. Mehrholz J, Wagner K, Rutte K, Meissner D, Pohl M. Predictive validity and responsiveness of the functional ambulation category in hemiparetic patients after stroke. Arch Phys Med Rehabil. 2007; 88:1314–9.
Article19. Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc. 2014; 15:95–101.
Article20. Sugie M, Harada K, Takahashi T, Nara M, Ishikawa J, Koyama T, et al. Relationship between skeletal muscle mass and cardiac function during exercise in community-dwelling older adults. ESC Heart Fail. 2017; 4:409–16.
Article21. Landi F, Liperoti R, Russo A, Giovannini S, Tosato M, Capoluongo E, et al. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr. 2012; 31:652–8.
Article22. Harimoto N, Yoshizumi T, Izumi T, Motomura T, Harada N, Itoh S, et al. Clinical outcomes of living liver transplantation according to the presence of sarcopenia as defined by skeletal muscle mass, hand grip, and gait speed. Transplant Proc. 2017; 49:2144–52.
Article23. Chen WZ, Chen XD, Ma LL, Zhang FM, Lin J, Zhuang CL, et al. Impact of visceral obesity and sarcopenia on short-term outcomes after colorectal cancer surgery. Dig Dis Sci. 2018; 63:1620–30.
Article24. Bokshan SL, DePasse JM, Daniels AH. Sarcopenia in orthopedic surgery. Orthopedics. 2016; 39:e295. –300.
Article25. Kim SC, Lee YG, Park SB, Kim TH, Lee KH. Muscle Mass, Strength, mobility, quality of life, and disease severity in ankylosing spondylitis patients: a preliminary study. Ann Rehabil Med. 2017; 41:990–7.
Article26. Addison O, Prior SJ, Kundi R, Serra MC, Katzel LI, Gardner AW, et al. Sarcopenia in peripheral arterial disease: prevalence and effect on functional status. Arch Phys Med Rehabil. 2018; 99:623–8.
Article27. Sporns PB, Muhle P, Hanning U, Suntrup-Krueger S, Schwindt W, Eversmann J, et al. Atrophy of swallowing muscles is associated with severity of dysphagia and age in patients with acute stroke. J Am Med Dir Assoc. 2017; 18:635.
Article28. Yi Y, Shim JS, Oh BM, Seo HG. Grip strength on the unaffected side as an independent predictor of functional improvement after stroke. Am J Phys Med Rehabil. 2017; 96:616–20.
Article29. Muscaritoli M, Anker SD, Argiles J, Aversa Z, Bauer JM, Biolo G, et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr. 2010; 29:154–9.
Article30. Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014; 69:547–58.
Article31. Ogaya S, Iwata A, Higuchi Y, Fuchioka S. The association between intersegmental coordination in the lower limb and gait speed in elderly females. Gait Posture. 2016; 48:1–5.
Article32. Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000; 55:M221–31.
Article33. Cesari M, Kritchevsky SB, Newman AB, Simonsick EM, Harris TB, Penninx BW, et al. Added value of physical performance measures in predicting adverse health-related events: results from the Health, Aging And Body Composition Study. J Am Geriatr Soc. 2009; 57:251–9.
Article34. Liu LK, Chen LY, Peng LN, Liu CL, Lin MH, Chen LK. Timed up-and-go test: a potential indicator for successful aging of older men in Taiwan. J Aging Res Clin Practice. 2013; 2:152–6.35. Peel NM, Kuys SS, Klein K. Gait speed as a measure in geriatric assessment in clinical settings: a systematic review. J Gerontol A Biol Sci Med Sci. 2013; 68:39–46.
Article36. An S, Lee Y, Shin H, Lee G. Gait velocity and walking distance to predict community walking after stroke. Nurs Health Sci. 2015; 17:533–8.
Article37. Marty E, Liu Y, Samuel A, Or O, Lane J. A review of sarcopenia: Enhancing awareness of an increasingly prevalent disease. Bone. 2017; 105:276–86.
Article38. Tsekoura M, Billis E, Tsepis E, Dimitriadis Z, Matzaroglou C, Tyllianakis M, et al. The effects of group and home-based exercise programs in elderly with sarcopenia: a randomized controlled trial. J Clin Med. 2018; 7:E480.
Article39. Yamada S, Kamiya K, Kono Y. Frailty may be a risk marker for adverse outcome in patients with congestive heart failure. ESC Heart Fail. 2015; 2:168–70.
Article40. Schoenfeld BJ, Grgic J, Ogborn D, Krieger JW. Strength and hypertrophy adaptations between low- vs. high-load resistance training: a systematic review and meta-analysis. J Strength Cond Res. 2017; 31:3508–23.
Article41. Yoshimura Y, Uchida K, Jeong S, Yamaga M. Effects of nutritional supplements on muscle mass and activities of daily living in elderly rehabilitation patients with decreased muscle mass: a randomized controlled trial. J Nutr Health Aging. 2016; 20:185–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Mirror Therapy on Recovery of Upper Limb Function and Strength in Subacute Hemiplegia after Stroke
- Relationship Between Grip and Pinch Strength and Activities of Daily Living in Stroke Patients
- Feasibility and Usability of a Robot-Assisted Complex Upper and Lower Limb Rehabilitation System in Patients with Stroke: A Pilot Study
- Cervicobrachial Disorders of Female International Telephone Operators III. Grip Strenghth
- The Effects of Hand Acupoint Massages on ADL Ability and Grip Strength of Stroke Patients