Obstet Gynecol Sci.
2019 Nov;62(6):483-486. 10.5468/ogs.2019.62.6.483.
A case of extremely early cervical adenocarcinoma diagnosed only by endocervical curettage with macroscopic pelvic lymph node metastases
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Wonkwang University Hospital, Wonkwang University School of Medicine, Iksan, Korea. brkim74@wku.ac.kr
- KMID: 2462129
- DOI: http://doi.org/10.5468/ogs.2019.62.6.483
Abstract
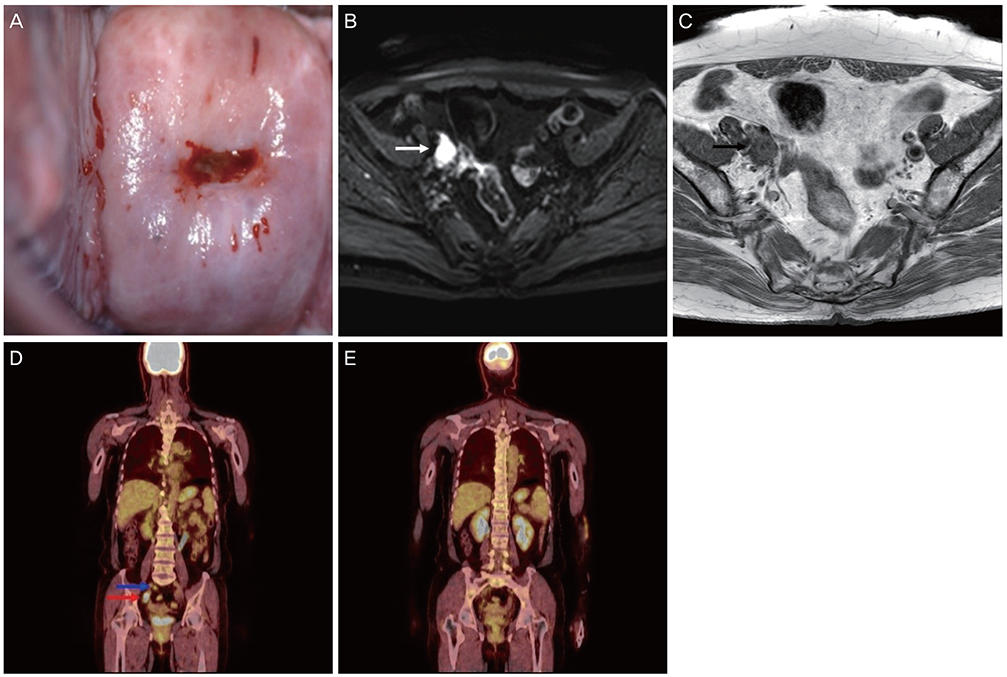
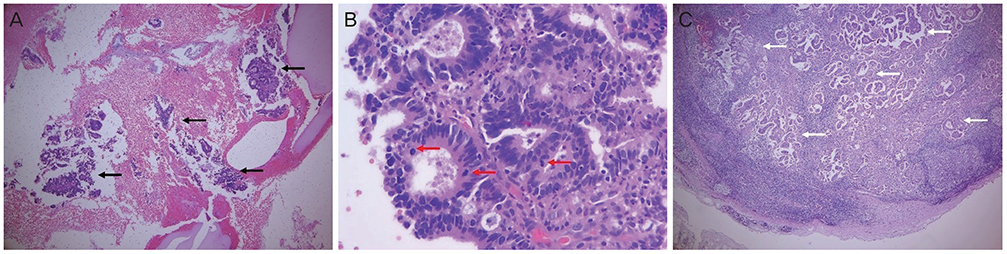
- Microinvasive adenocarcinoma is not as well studied as microinvasive squamous cell carcinoma because diagnosis of adenocarcinoma cannot be ascertained for early invasive lesions. However, most clinicians consider a depth of invasion of 3 mm without lympho-vascular space invasion as the maximum limit for conservative management. Microinvasive cervical adenocarcinoma is characterized by a rare incidence of lymph node metastasis and very good prognosis. We describe a 62-year-old patient with an extremely early cervical adenocarcinoma which was detected only by endocervical curettage. However, she had multiple macroscopic pelvic node metastases. Clinicians should consider the probability of lymph node metastasis, although management of stage IA1 cervical adenocarcinoma may still be conservative.
MeSH Terms
Figure
Reference
-
1. Sherman ME, Wang SS, Carreon J, Devesa SS. Mortality trends for cervical squamous and adenocarcinoma in the United States. Relation to incidence and survival. Cancer. 2005; 103:1258–1264.2. Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009; 105:103–104.
Article3. Baalbergen A, Smedts F, Helmerhorst TJ. Conservative therapy in microinvasive adenocarcinoma of the uterine cervix is justified: an analysis of 59 cases and a review of the literature. Int J Gynecol Cancer. 2011; 21:1640–1645.
Article4. Bean LM, Ward KK, Plaxe SC, McHale MT. Survival of women with microinvasive adenocarcinoma of the cervix is not improved by radical surgery. Am J Obstet Gynecol. 2017; 217:332.e1–332.e6.
Article5. Reynolds EA, Tierney K, Keeney GL, Felix JC, Weaver AL, Roman LD, et al. Analysis of outcomes of microinvasive adenocarcinoma of the uterine cervix by treatment type. Obstet Gynecol. 2010; 116:1150–1157.
Article6. Nagarsheth NP, Maxwell GL, Bentley RC, Rodriguez G. Bilateral pelvic lymph node metastases in a case of FIGO stage IA(1) adenocarcinoma of the cervix. Gynecol Oncol. 2000; 77:467–470.
Article7. Galic V, Herzog TJ, Lewin SN, Neugut AI, Burke WM, Lu YS, et al. Prognostic significance of adenocarcinoma histology in women with cervical cancer. Gynecol Oncol. 2012; 125:287–291.
Article8. Lee YY, Choi CH, Kim TJ, Lee JW, Kim BG, Lee JH, et al. A comparison of pure adenocarcinoma and squamous cell carcinoma of the cervix after radical hysterectomy in stage IB–IIA. Gynecol Oncol. 2011; 120:439–443.
Article9. Im SS, Wilczynski SP, Burger RA, Monk BJ. Early stage cervical cancers containing human papillomavirus type 18 DNA have more nodal metastasis and deeper stromal invasion. Clin Cancer Res. 2003; 9:4145–4150.10. Akladios C, Lecointre L, Baulon E, Thoma V, Averous G, Fender M, et al. Reliability of endocervical curettage in the diagnosis of high-grade cervical neoplasia and cervical cancer in selected patients. Anticancer Res. 2015; 35:4183–4189.11. Holschneider CH, Berek JS. Valvar cancer. In : Berek JS, Novak E, editors. Berek & Novak's gynecology. 15th ed. Philadelphia (PA): Lippincott Williams & Wilkins;2014. p. 135–137.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pelvic Lymph Node Metastases in Cervical Carcinoma with Early Stromal Invasion
- A case of minimal uterine serous carcinoma with distant lymph node metastasis without peritoneal dissemination
- Pelvic Lymph Node Evaluation in Uterine Cervical Carcinoma Using Contrast Enhanced MR Imaging
- Chylous ascites, following radical hysterectomy with pelvic lymph node dissection in a patient with cervical cancer
- Clinicopathological Significance of FHIT Protein Expression in Cervical Adenocarcinoma