J Gynecol Oncol.
2011 Mar;22(1):53-56. 10.3802/jgo.2011.22.1.53.
A case of minimal uterine serous carcinoma with distant lymph node metastasis without peritoneal dissemination
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Kurume University School of Medicine, Fukuoka, Japan. kawano_kouichirou@kurume-u.ac.jp
- KMID: 2173587
- DOI: http://doi.org/10.3802/jgo.2011.22.1.53
Abstract
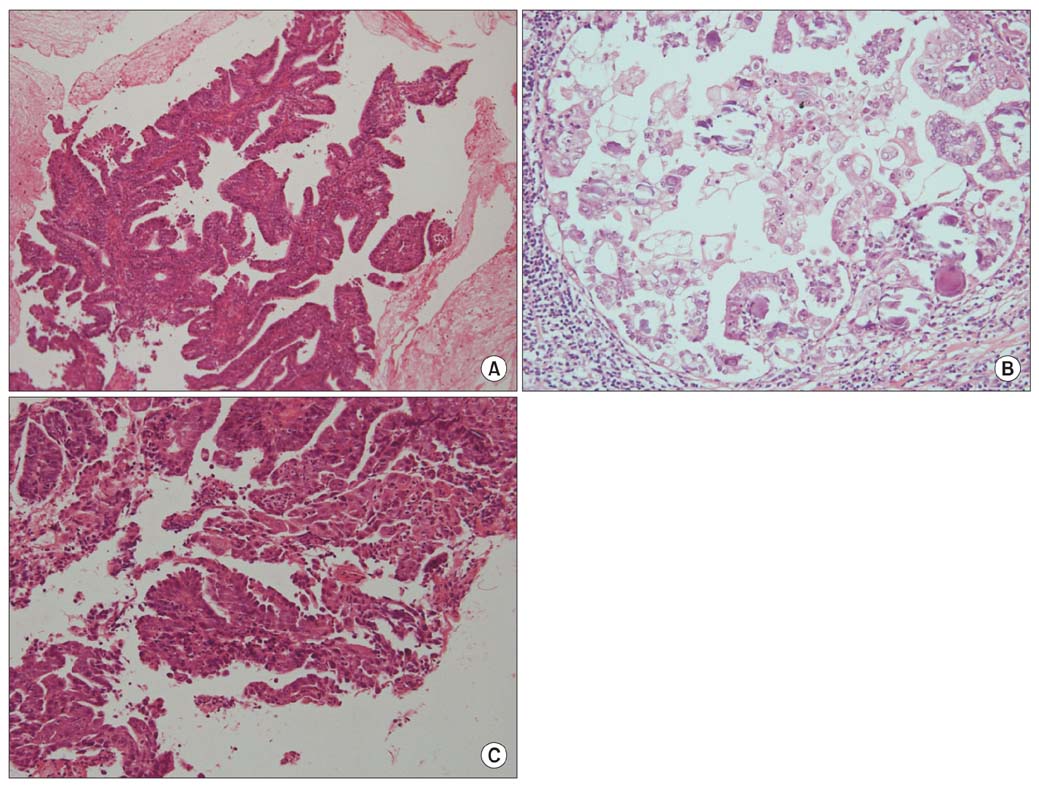
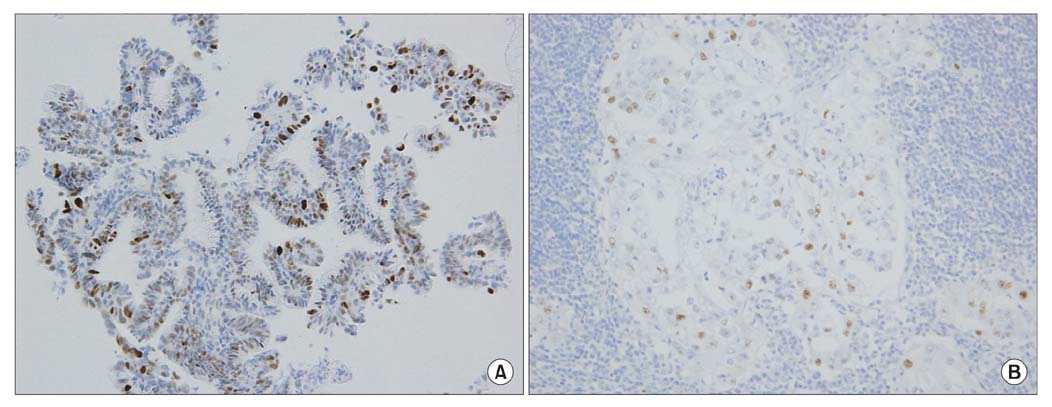
- A 61-year old woman underwent total abdominal hysterectomy and pelvic lymph node dissection under the diagnosis of endometrial cancer. Although pelvic lymph nodes were positive for adenocarcinoma with psamomma bodies, no other lesion that was a primary lesion was verified. A postoperative study revealed the existence of para-aortic lymph node and supraclavicular lymph node metastases. Therefore, the endometrial biopsy specimen was reviewed. With the findings of p53 positivity by immunohistochemistry in the papillary part, the final histopathological diagnosis was changed to endometrial serous adenocarcinoma. Postoperative chemotherapy followed by radiotherapy for supraclavicular lymph node metastasis achieved complete response. This type of tumor must be considered in a differential diagnosis when metastatic papillary serous carcinoma is detected, but the primary site remains unknown.
MeSH Terms
Figure
Reference
-
1. Abeler VM, Kjorstad KE. Serous papillary carcinoma of the endometrium: a histopathological study of 22 cases. Gynecol Oncol. 1990. 39:266–271.2. Wheeler DT, Bell KA, Kurman RJ, Sherman ME. Minimal uterine serous carcinoma: diagnosis and clinicopathologic correlation. Am J Surg Pathol. 2000. 24:797–806.3. Hui P, Kelly M, O'Malley DM, Tavassoli F, Schwartz PE. Minimal uterine serous carcinoma: a clinicopathological study of 40 cases. Mod Pathol. 2005. 18:75–82.4. Hamilton CA, Cheung MK, Osann K, Chen L, Teng NN, Longacre TA, et al. Uterine papillary serous and clear cell carcinomas predict for poorer survival compared to grade 3 endometrioid corpus cancers. Br J Cancer. 2006. 94:642–646.5. Acharya S, Hensley ML, Montag AC, Fleming GF. Rare uterine cancers. Lancet Oncol. 2005. 6:961–971.6. Grice J, Ek M, Greer B, Koh WJ, Muntz HG, Cain J, et al. Uterine papillary serous carcinoma: evaluation of long-term survival in surgically staged patients. Gynecol Oncol. 1998. 69:69–73.7. Goff BA, Kato D, Schmidt RA, Ek M, Ferry JA, Muntz HG, et al. Uterine papillary serous carcinoma: patterns of metastatic spread. Gynecol Oncol. 1994. 54:264–268.8. Christman JE, Kapp DS, Hendrickson MR, Howes AE, Ballon SC. Therapeutic approaches to uterine papillary serous carcinoma: a preliminary report. Gynecol Oncol. 1987. 26:228–235.9. Darvishian F, Hummer AJ, Thaler HT, Bhargava R, Linkov I, Asher M, et al. Serous endometrial cancers that mimic endometrioid adenocarcinomas: a clinicopathologic and immunohistochemical study of a group of problematic cases. Am J Surg Pathol. 2004. 28:1568–1578.10. Zheng W, Khurana R, Farahmand S, Wang Y, Zhang ZF, Felix JC. p53 immunostaining as a significant adjunct diagnostic method for uterine surface carcinoma: precursor of uterine papillary serous carcinoma. Am J Surg Pathol. 1998. 22:1463–1473.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary peritoneal serous papillary carcinoma presenting as a large mesenteric mass mistaken for ovarian cancer: a case of primary peritoneal carcinoma
- Pattern of Distant Lymph Node Metastasis in Colorectal Carcinoma and its Correlation with Distant Organ Metastasis: CT Evaluation
- CT evaluation of colon carcinoma: Emphasis on distant lymph node invasion and liver metastases
- A Case of Primary Peritoneal Carcinoma
- A Recurrence of Ovarian Carcinoma Presenting as Only Axillary Lymphatic Metastasis: A Case Report