J Korean Assoc Oral Maxillofac Surg.
2019 Oct;45(5):260-266. 10.5125/jkaoms.2019.45.5.260.
7-mm-long dental implants: retrospective clinical outcomes in medically compromised patients
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea. smin5@snu.ac.kr
- KMID: 2461478
- DOI: http://doi.org/10.5125/jkaoms.2019.45.5.260
Abstract
OBJECTIVES
Dental implants shorter than 8 mm, called short dental implants (SDIs), have been considered to have a lower success rate than standard length implants. But recent studies have shown that SDIs have a comparable success rate, and implant diameter was more important for implant survival than implant length. Also, SDIs have many advantages, such as no need for sinus lifting or vertical bone grafting, which may limit use in medically compromised patients.
MATERIALS AND METHODS
In this study, 33 patients with 47 implants 7-mm long were examined over the last four years. All patients had special medical history and were categorized into 3 groups: systemic disorders, such as diabetes mellitus (controlled or uncontrolled), mental disability, and uncontrolled hypertension; oral cancer ablation with reconstruction, with or without radiotherapy; diverse osteomyelitis, such as osteoradionecrosis and bisphosphonate-related osteonecrosis of the jaw. Most of these patients have insufficient residual bone quality due to mandible atrophy or sinus pneumatization.
RESULTS
The implant diameters were 4.0 (n=38), 4.5 (n=8), and 5.0 mm (n=1). Among the 47 implants placed, 2 implants failed before the last follow-up. The survival rate of 7-mm SDIs was 95.74% from stage I surgery to the last follow-up. Survival rates did not differ according to implant diameter. The mean marginal bone loss (MBL) at 3 months, 1 and 2 years was significantly higher than at implant installation, and the MBL at 1 year was also significantly higher than at 3 months. MBL at 1 and 2 years did not differ significantly.
CONCLUSION
Within the limitations of the present study, the results indicate that SDIs provide a reliable treatment, especially for medically compromised patients, to avoid sinus lifting or vertical bone grafting. Further, long-term follow-up is needed.
Keyword
MeSH Terms
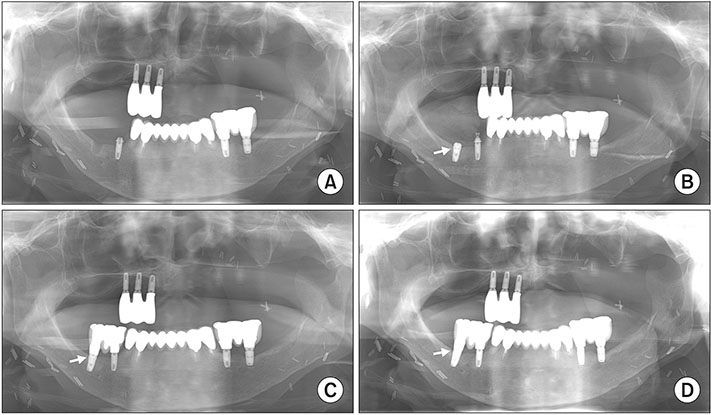
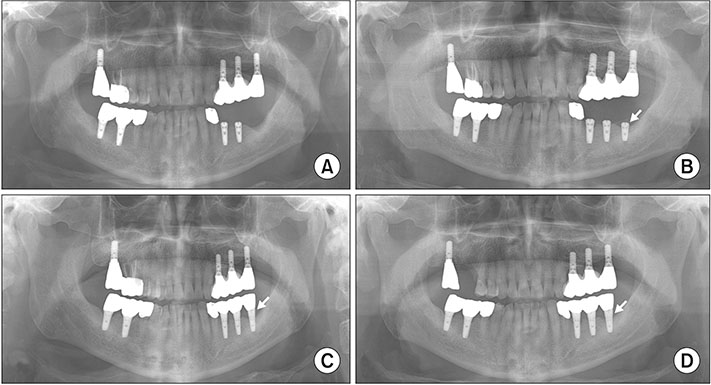
Figure
Reference
-
1. Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res. 2006; 17 Suppl 2:35–51.
Article2. Jain N, Gulati M, Garg M, Pathak C. Short implants: new horizon in implant dentistry. J Clin Diagn Res. 2016; 10:ZE14–ZE17.
Article3. Al-Hashedi AA, Taiyeb Ali TB, Yunus N. Short dental implants: an emerging concept in implant treatment. Quintessence Int. 2014; 45:499–514.4. Nisand D, Renouard F. Short implant in limited bone volume. Periodontol 2000. 2014; 66:72–96.
Article5. Sennerby L, Roos J. Surgical determinants of clinical success of osseointegrated oral implants: a review of the literature. Int J Prosthodont. 1998; 11:408–420.6. Wyatt CC, Zarb GA. Treatment outcomes of patients with implant-supported fixed partial prostheses. Int J Oral Maxillofac Implants. 1998; 13:204–211.7. Srinivasan M, Vazquez L, Rieder P, Moraguez O, Bernard JP, Belser UC. Efficacy and predictability of short dental implants (<8 mm): a critical appraisal of the recent literature. Int J Oral Maxillofac Implants. 2012; 27:1429–1437.8. Karthikeyan I, Desai SR, Singh R. Short implants: a systematic review. J Indian Soc Periodontol. 2012; 16:302–312.
Article9. Lemos CA, Ferro-Alves ML, Okamoto R, Mendonça MR, Pellizzer EP. Short dental implants versus standard dental implants placed in the posterior jaws: a systematic review and meta-analysis. J Dent. 2016; 47:8–17.
Article10. Benlidayi ME, Ucar Y, Tatli U, Ekren O, Evlice B, Kisa HI, et al. Short implants versus standard implants: midterm outcomes of a clinical study. Implant Dent. 2018; 27:95–100.11. Esfahrood ZR, Ahmadi L, Karami E, Asghari S. Short dental implants in the posterior maxilla: a review of the literature. J Korean Assoc Oral Maxillofac Surg. 2017; 43:70–76.
Article12. Pierrisnard L, Renouard F, Renault P, Barquins M. Influence of implant length and bicortical anchorage on implant stress distribution. Clin Implant Dent Relat Res. 2003; 5:254–262.
Article13. Anitua E, Tapia R, Luzuriaga F, Orive G. Influence of implant length, diameter, and geometry on stress distribution: a finite element analysis. Int J Periodontics Restorative Dent. 2010; 30:89–95.14. Chen H, Liu N, Xu X, Qu X, Lu E. Smoking, radiotherapy, diabetes and osteoporosis as risk factors for dental implant failure: a meta-analysis. PLoS One. 2013; 8:e71955.
Article15. Moy PK, Medina D, Shetty V, Aghaloo TL. Dental implant failure rates and associated risk factors. Int J Oral Maxillofac Implants. 2005; 20:569–577.16. Guobis Z, Pacauskiene I, Astramskaite I. General diseases influence on peri-implantitis development: a systematic review. J Oral Maxillofac Res. 2016; 7:e5.
Article17. Liddelow G, Klineberg I. Patient-related risk factors for implant therapy. A critique of pertinent literature. Aust Dent J. 2011; 56:417–426. quiz 441.
Article18. Renvert S, Aghazadeh A, Hallström H, Persson GR. Factors related to peri-implantitis - a retrospective study. Clin Oral Implants Res. 2014; 25:522–529.19. Kasai T, Pogrel MA, Hossaini M. The prognosis for dental implants placed in patients taking oral bisphosphonates. J Calif Dent Assoc. 2009; 37:39–42.20. Galindo-Moreno P, León-Cano A, Ortega-Oller I, Monje A, O Valle F, Catena A. Marginal bone loss as success criterion in implant dentistry: beyond 2 mm. Clin Oral Implants Res. 2015; 26:e28–e34.21. Diz P, Scully C, Sanz M. Dental implants in the medically compromised patient. J Dent. 2013; 41:195–206.
Article22. Grant BT, Pancko FX, Kraut RA. Outcomes of placing short dental implants in the posterior mandible: a retrospective study of 124 cases. J Oral Maxillofac Surg. 2009; 67:713–717.
Article23. Barrowman RA, Wilson PR, Wiesenfeld D. Oral rehabilitation with dental implants after cancer treatment. Aust Dent J. 2011; 56:160–165.
Article24. Renouard F, Nisand D. Short implants in the severely resorbed maxilla: a 2-year retrospective clinical study. Clin Implant Dent Relat Res. 2005; 7 Suppl 1:S104–S110.
Article25. Jemt T, Lindén B, Lekholm U. Failures and complications in 127 consecutively placed fixed partial prostheses supported by Brånemark implants: from prosthetic treatment to first annual checkup. Int J Oral Maxillofac Implants. 1992; 7:40–44.
Article26. Becker W, Becker BE, Alsuwyed A, Al-Mubarak S. Long-term evaluation of 282 implants in maxillary and mandibular molar positions: a prospective study. J Periodontol. 1999; 70:896–901.
Article27. Lee JH, Frias V, Lee KW, Wright RF. Effect of implant size and shape on implant success rates: a literature review. J Prosthet Dent. 2005; 94:377–381.
Article28. Morand M, Irinakis T. The challenge of implant therapy in the posterior maxilla: providing a rationale for the use of short implants. J Oral Implantol. 2007; 33:257–266.
Article29. Mohajerani H, Roozbayani R, Taherian S, Tabrizi R. The risk factors in early failure of dental implants: a retrospective study. J Dent (Shiraz). 2017; 18:298–303.30. Bratu E, Chan HL, Mihali S, Karancsi O, Bratu DC, Fu JH, et al. Implant survival rate and marginal bone loss of 6-mm short implants: a 2-year clinical report. Int J Oral Maxillofac Implants. 2014; 29:1425–1428.
Article31. Monje A, Chan HL, Fu JH, Suarez F, Galindo-Moreno P, Wang HL. Are short dental implants (<10 mm) effective? A meta-analysis on prospective clinical trials. J Periodontol. 2013; 84:895–904.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A 10‑year survival rate of tapered self‑tapping bone‑level implants from medically compromised Korean patients at a maxillofacial surgical unit
- Revisiting root resection treatment in the age of dental implants
- Valplast(R) flexible removable partial denture for a patient with medically compromised conditions: a clinical report
- Clinical and scanning electron microscopic analysis of fractured dental implants: a retrospective clinical analysis
- Periodontal prosthesis on medically compromised patient with few remaining teeth: hybrid telescopic double crown with friction pin method