J Korean Acad Prosthodont.
2019 Oct;57(4):356-363. 10.4047/jkap.2019.57.4.356.
Prosthetic rehabilitation by double-processing technique for edentulous patient with soft palate defect after maxillectomy: A case report
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry and Institute of Oral Bio-Science, Chonbuk National University, Jeonju, Republic of Korea. wjdwls04@gmail.com
- 2Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute, Chonbuk National University Hospital, Jeonju, Republic of Korea.
- KMID: 2461142
- DOI: http://doi.org/10.4047/jkap.2019.57.4.356
Abstract
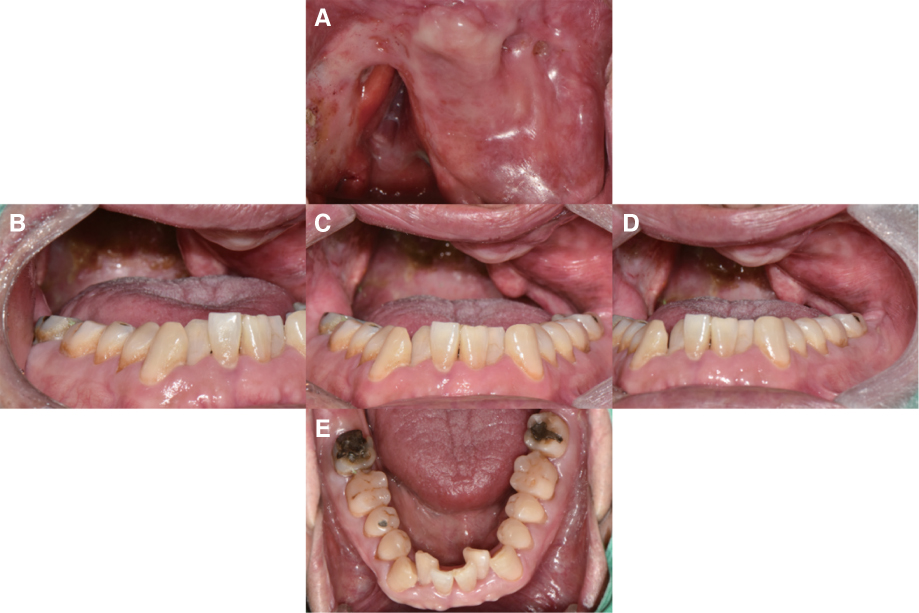
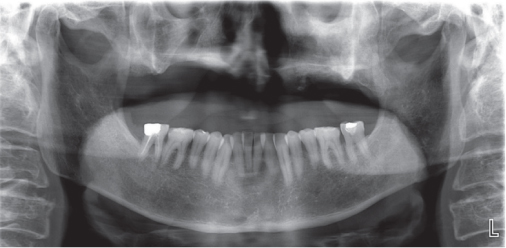
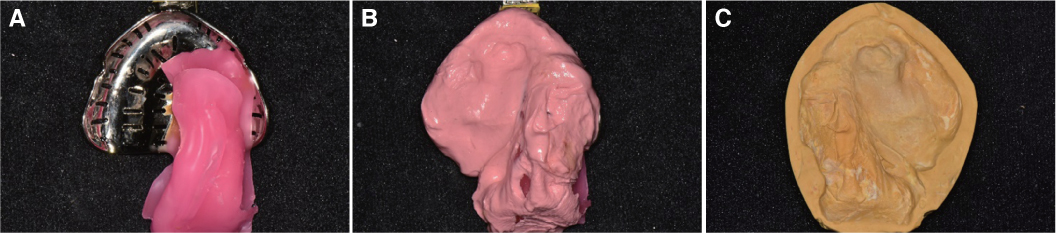
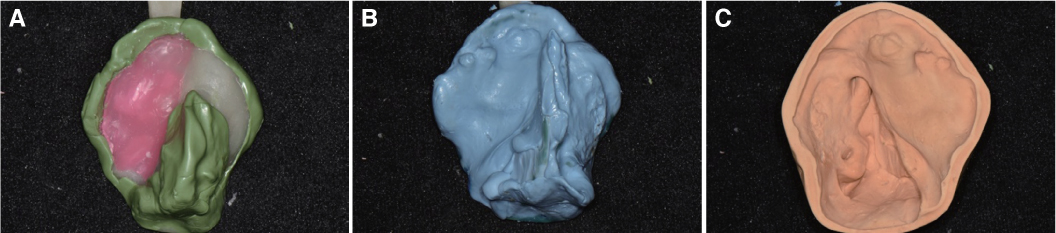
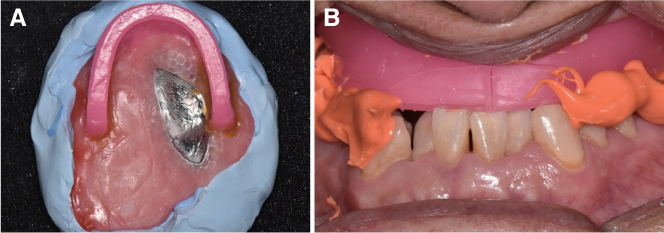
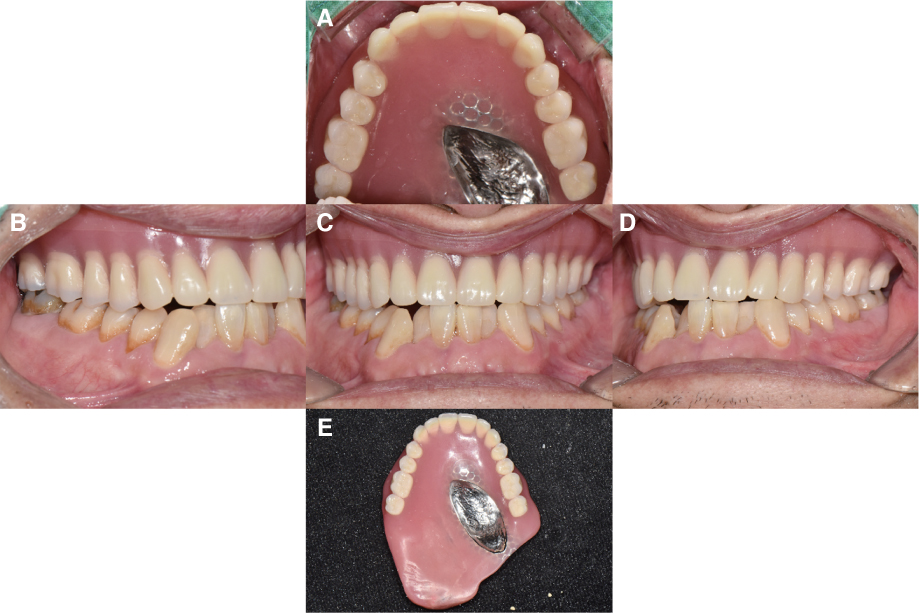
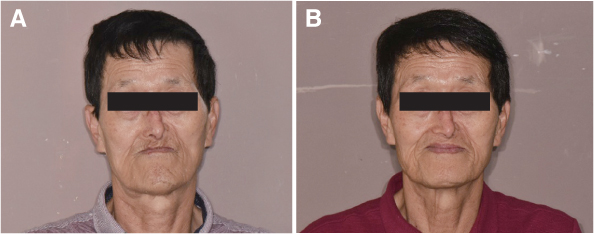
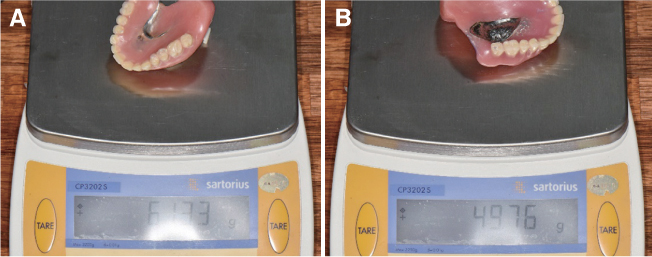
- A patient who went through maxillectomy can have soft palate defects including oronasal fistulas and suffer from dysphagia and dysarthria due to velopharyngeal insufficiency. This defect causes the food to enter nasal cavity and creates hypernasal sound which debilitates a quality of life. An obturator can rehabilitate the substantial oral tissue defects. The maxillary obturator separates the nasopharynx from the oropharynx during speech and deglutition by closing of the defect. For edentulous obturator patient, it is difficult to obtain proper retention due to reduced peripheral sealing. Therefore, the contours of the defects must be used to maximize the retention, stability, and support. Hollow type obturator can improve physiologic function by reducing weight than the traditional obturator. This case report describes a patient with hemi-maxillectomy who recovers mastication, speech, deglutition, and appearance with a maxillary obturator using physiological border molding of the velopharyngeal area and double-processing method.
Keyword
MeSH Terms
Figure
Reference
-
1. Beumer J, Marunick MT, Esposito SJ. Maxillofacial rehabilitation: prosthodontic and surgical management of cancerrelated, acquired, and congenital defects of the head and neck. Quintessence Pub;2011. p. 175–181.2. Zarb GA, Hobkirk J, Eckert S, Jacob R. Prosthodontic treatment for edentulous patients: complete dentures and implantsupported prosthesis. Elsevier;2013. p. 351–366.3. Brown KE. Peripheral consideration in improving obturator retention. J Prosthet Dent. 1968; 20:176–181.
Article4. Desjardins RP. Obturator prosthesis design for acquired maxillary defect. J Prosthet Dent. 1978; 39:424–435.5. Schwartzman B, Caputo AA, Beumer J. Gravity-induced stresses by an obturator prosthesis. J Prosthet Dent. 1990; 64:466–468.
Article6. Minsley GE, Nelson DR, Rothenberger SL. An alternative method for fabrication of a closed hollow obturator. J Prosthet Dent. 1986; 55:485–490.
Article7. Matalon V, LaFuente H. A simplified method for making a hollow obturator. J Prosthet Dent. 1976; 36:580–582.
Article8. Oh WS, Roumanas ED. Optimization of maxillary obturator thickness using a double-processing technique. J Prosthodont. 2008; 17:60–63.
Article9. Seaver EJ, Dalston RM, Leeper HA, Adams LE. A study of nasometric values for normal nasal resonance. J Speech Hear Res. 1991; 34:715–721.
Article10. Aramany MA. Basic principles of obturator design for partially edentulous patients. Part I: classification. J Prosthet Dent. 1978; 40:554–557.
Article11. Eckert SE, Desjardins RP, Taylor TD. Clinical maxillofacial prosthetics. 1st ed. Quintessence Pub;2000. p. 125–131.12. Wu YL, Schaaf NG. Comparison of weight reduction in different designs of solid and hollow obturator prostheses. J Prosthet Dent. 1989; 62:214–217.
Article13. Murata H, Hamada T, Nagasiri R. Stabilizing record bases for edentulous obturator prostheses with silicone resilient relining material. J Prosthet Dent. 1999; 82:366–368.
Article14. Kim SI, Baik JA, Shin HK, Kim OH. Study of nasalance for normal Korean adults using nasometer II. Speech Science. 2000; 7:219–228.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prosthetic rehabilitation of soft palate resection edentulous patient with maxillary obturator
- Prosthetic rehabilitation using an obturator in a fully edentulous patient who had partial maxillectomy
- Prosthetic rehabilitation of partially edentulous patient after maxillectomy: A case report
- Prosthetic rehabilitation of a fully edentulous patient after maxillectomy: A case report
- Removable prosthetic rehabilitation in patient with maxillofacial defects caused by gunshot: A case report