Cancer Res Treat.
2019 Oct;51(4):1370-1379. 10.4143/crt.2018.423.
Korean First Prospective Phase II Study, Feasibility of Prone Position in Postoperative Whole Breast Radiotherapy: A Dosimetric Comparison
- Affiliations
-
- 1Department of Nuclear Engineering, Hanyang University, Seoul, Korea.
- 2Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. doho.choi@samsung.com
- KMID: 2460586
- DOI: http://doi.org/10.4143/crt.2018.423
Abstract
- PURPOSE
This first Korean prospective study is to evaluate the feasibility of prone breast radiotherapy after breast conserving surgery for left breast cancer patients who have relatively small breast size and we present dosimetric comparison between prone and supine positions.
MATERIALS AND METHODS
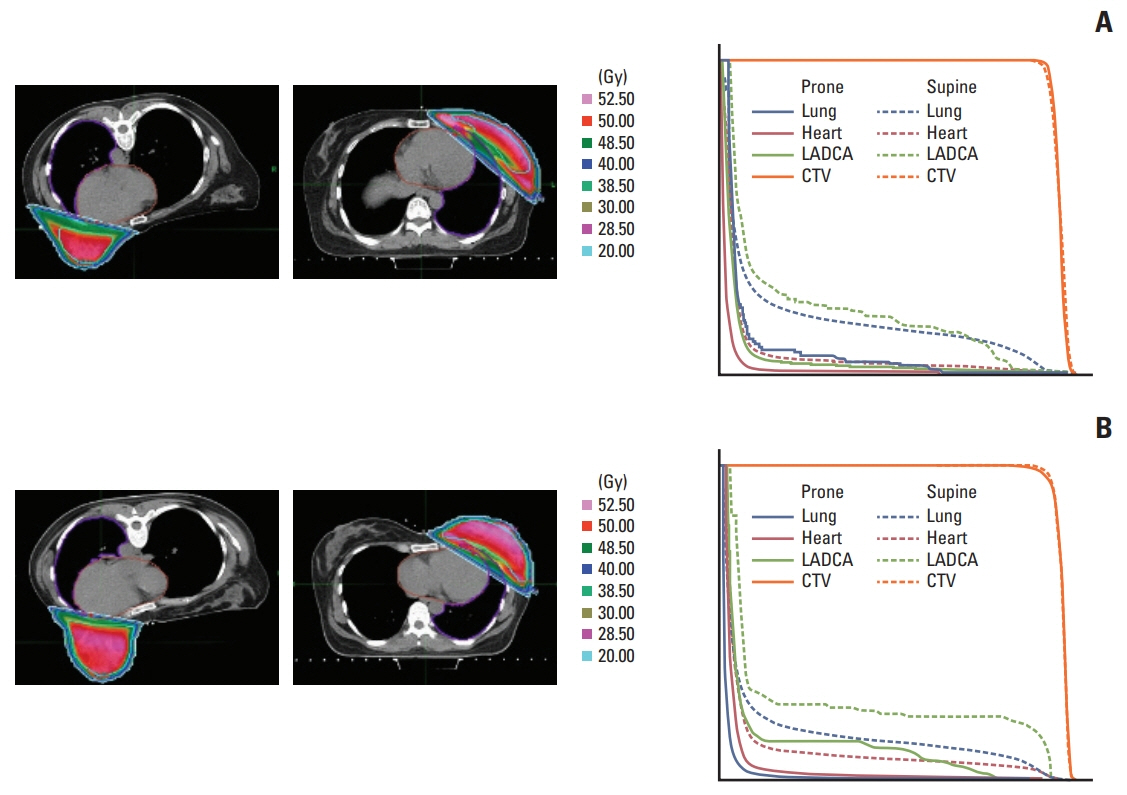
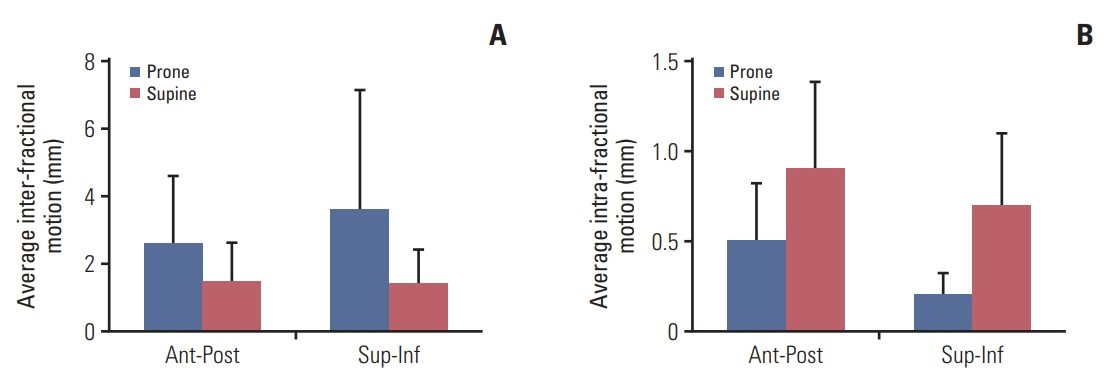
Fifty patients underwent two computed tomography (CT) simulations in supine and prone positions. Whole breast, ipsilateral lung, heart, and left-anterior-descending coronary artery were contoured on each simulation CT images. Tangential-fields treatment plan in each position was designed with total 50 Gy in 2-Gy fractions, and then one of the positions was designated for the treatment by comparing target coverage and dose to normal organs. Also, interfractional and intrafractional motion was evaluated using portal images.
RESULTS
In total 50 patients, 32 cases were decided as prone-position-beneficial group and 18 cases as supine-position-beneficial group based on dosimetric advantage. Target dose homogeneity was comparable, but target conformity in prone position was closer to optimal than in supine position. For both group, prone position significantly increased lung volume. However, heart volumewas decreased by prone position for prone-position-beneficial group but was comparable between two positions for supine-position-beneficial group. Lung and heart doses were significantly decreased by prone position for prone-position-beneficial group. However, prone position for supine-position-beneficial group increased heart dose while decreasing lung dose. Prone position showed larger interfractional motion but smaller intra-fractional motion than supine position.
CONCLUSION
Prone breast radiotherapy could be beneficial to a subset of small breast patients since it substantially spared normal organs while achieving adequate target coverage.
MeSH Terms
Figure
Reference
-
References
1. Torre LA, Islami F, Siegel RL, Ward EM, Jemal A. Global cancer in women: burden and trends. Cancer Epidemiol Biomarkers Prev. 2017; 26:444–57.
Article2. Jung KW, Won YJ, Kong HJ, Lee ES; Community of Population-Based Regional Cancer Registries. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2015. Cancer Res Treat. 2018; 50:303–16.
Article3. Early Breast Cancer Trialists' Collaborative Group, Darby S, McGale P, Correa C, Taylor C, Arriagada R, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011; 378:1707–16.4. Darby SC, McGale P, Taylor CW, Peto R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol. 2005; 6:557–65.
Article5. Marks LB, Yu X, Prosnitz RG, Zhou SM, Hardenbergh PH, Blazing M, et al. The incidence and functional consequences of RT-associated cardiac perfusion defects. Int J Radiat Oncol Biol Phys. 2005; 63:214–23.
Article6. Correa CR, Litt HI, Hwang WT, Ferrari VA, Solin LJ, Harris EE. Coronary artery findings after left-sided compared with right-sided radiation treatment for early-stage breast cancer. J Clin Oncol. 2007; 25:3031–7.
Article7. Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Bronnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013; 368:987–98.
Article8. Paul Wright G, Drinane JJ, Sobel HL, Chung MH. Left-sided breast irradiation does not result in increased long-term cardiac-related mortality among women treated with breast-conserving surgery. Ann Surg Oncol. 2016; 23:1117–22.
Article9. Yu TK, Whitman GJ, Thames HD, Buzdar AU, Strom EA, Perkins GH, et al. Clinically relevant pneumonitis after sequential paclitaxel-based chemotherapy and radiotherapy in breast cancer patients. J Natl Cancer Inst. 2004; 96:1676–81.
Article10. Borst GR, De Jaeger K, Belderbos JS, Burgers SA, Lebesque JV. Pulmonary function changes after radiotherapy in non-small-cell lung cancer patients with long-term disease-free survival. Int J Radiat Oncol Biol Phys. 2005; 62:639–44.
Article11. Campana F, Kirova YM, Rosenwald JC, Dendale R, Vilcoq JR, Dreyfus H, et al. Breast radiotherapy in the lateral decubitus position: a technique to prevent lung and heart irradiation. Int J Radiat Oncol Biol Phys. 2005; 61:1348–54.
Article12. Kirova YM, Hijal T, Campana F, Fournier-Bidoz N, Stilhart A, Dendale R, et al. Whole breast radiotherapy in the lateral decubitus position: a dosimetric and clinical solution to decrease the doses to the organs at risk (OAR). Radiother Oncol. 2014; 110:477–81.
Article13. Huppert N, Jozsef G, Dewyngaert K, Formenti SC. The role of a prone setup in breast radiation therapy. Front Oncol. 2011; 1:31.
Article14. Remouchamps VM, Letts N, Vicini FA, Sharpe MB, Kestin LL, Chen PY, et al. Initial clinical experience with moderate deepinspiration breath hold using an active breathing control device in the treatment of patients with left-sided breast cancer using external beam radiation therapy. Int J Radiat Oncol Biol Phys. 2003; 56:704–15.
Article15. Shah C, Badiyan S, Berry S, Khan AJ, Goyal S, Schulte K, et al. Cardiac dose sparing and avoidance techniques in breast cancer radiotherapy. Radiother Oncol. 2014; 112:9–16.
Article16. Mulliez T, Veldeman L, van Greveling A, Speleers B, Sadeghi S, Berwouts D, et al. Hypofractionated whole breast irradiation for patients with large breasts: a randomized trial comparing prone and supine positions. Radiother Oncol. 2013; 108:203–8.
Article17. Formenti SC, DeWyngaert JK, Jozsef G, Goldberg JD. Prone vs supine positioning for breast cancer radiotherapy. JAMA. 2012; 308:861–3.
Article18. Lymberis SC, deWyngaert JK, Parhar P, Chhabra AM, FentonKerimian M, Chang J, et al. Prospective assessment of optimal individual position (prone versus supine) for breast radiotherapy: volumetric and dosimetric correlations in 100 patients. Int J Radiat Oncol Biol Phys. 2012; 84:902–9.
Article19. Kirby AM, Evans PM, Donovan EM, Convery HM, Haviland JS, Yarnold JR. Prone versus supine positioning for whole and partial-breast radiotherapy: a comparison of non-target tissue dosimetry. Radiother Oncol. 2010; 96:178–84.
Article20. Fernandez-Lizarbe E, Montero A, Polo A, Hernanz R, Moris R, Formenti S, et al. Pilot study of feasibility and dosimetric comparison of prone versus supine breast radiotherapy. Clin Transl Oncol. 2013; 15:450–9.
Article21. Bartlett FR, Colgan RM, Donovan EM, McNair HA, Carr K, Evans PM, et al. The UK HeartSpare Study (Stage IB): randomised comparison of a voluntary breath-hold technique and prone radiotherapy after breast conserving surgery. Radiother Oncol. 2015; 114:66–72.
Article22. Hannan R, Thompson RF, Chen Y, Bernstein K, Kabarriti R, Skinner W, et al. Hypofractionated whole-breast radiation therapy: does breast size matter? Int J Radiat Oncol Biol Phys. 2012; 84:894–901.
Article23. Chen JL, Cheng JC, Kuo SH, Chan HM, Huang YS, Chen YH. Prone breast forward intensity-modulated radiotherapy for Asian women with early left breast cancer: factors for cardiac sparing and clinical outcomes. J Radiat Res. 2013; 54:899–908.
Article24. Lee HY, Chang JS, Lee IJ, Park K, Kim YB, Suh CO, et al. The deep inspiration breath hold technique using Abches reduces cardiac dose in patients undergoing left-sided breast irradiation. Radiat Oncol J. 2013; 31:239–46.
Article25. Yoon M, Park SY, Shin D, Lee SB, Pyo HR, Kim DY, et al. A new homogeneity index based on statistical analysis of the dose-volume histogram. J Appl Clin Med Phys. 2007; 8:9–17.
Article26. Feuvret L, Noel G, Mazeron JJ, Bey P. Conformity index: a review. Int J Radiat Oncol Biol Phys. 2006; 64:333–42.
Article27. Takahashi K, Morota M, Kagami Y, Okamoto H, Sekii S, Inaba K, et al. Prospective study of postoperative whole breast radiotherapy for Japanese large-breasted women: a clinical and dosimetric comparisons between supine and prone positions and a dose measurement using a breast phantom. BMC Cancer. 2016; 16:757.
Article28. Morrow NV, Stepaniak C, White J, Wilson JF, Li XA. Intra- and interfractional variations for prone breast irradiation: an indication for image-guided radiotherapy. Int J Radiat Oncol Biol Phys. 2007; 69:910–7.
Article29. Mitchell J, Formenti SC, DeWyngaert JK. Interfraction and intrafraction setup variability for prone breast radiation therapy. Int J Radiat Oncol Biol Phys. 2010; 76:1571–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Dosimetric Parameters of Patient with Large and Pendulous Breast Receiving Breast Radiotherapy in the Prone versus Supine Position
- Dosimetric Advantages of the Field-in-field Plan Compared with the Tangential Wedged Beams Plan for Whole-breast Irradiation
- The Effect of Laryngeal Mask Airway on Postoperative Sore Throat in Prone Position
- The Supine and Prone Position for Computed Tomographic Myelography(CTM) of the Lumbar Spine: Change of Gantry Angle
- Analysis on the Dosimetric Characteristics of Tangential Breast Intensity Modulated Radiotherapy