J Korean Ophthalmol Soc.
2019 Oct;60(10):935-945. 10.3341/jkos.2019.60.10.935.
Clinical Analysis of Staphylococcus Keratitis According to Coagulase Positivity
- Affiliations
-
- 1Department of Ophthalmology, Yeungnam University College of Medicine, Daegu, Korea. sbummlee@ynu.ac.kr
- KMID: 2460511
- DOI: http://doi.org/10.3341/jkos.2019.60.10.935
Abstract
- PURPOSE
To analyze clinical aspects in a cohort of patients with Staphylococcus keratitis according to coagulase positivity (coagulase negative Staphylococcus [CNS], coagulase positive Staphylococcus [CPS]).
METHODS
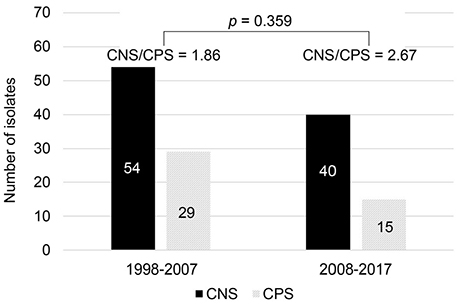
Epidemiology, predisposing factors, clinical characteristics, treatment outcomes, and antibiotic susceptibility were comparatively analyzed in 138 cases of culture-proven Staphylococcus keratitis (94 eyes with CNS and 44 eyes with CPS) over 20 years (1998-2017) at Yeungnam University Hospital. Poor clinical outcomes were defined as a final corrected visual acuity <0.1, a decreased visual acuity after treatment, complications, or surgical treatment. Risk factors for poor clinical outcomes were evaluated in the total cohort and analyzed using multivariate logistic regression.
RESULTS
The most common predisposing factors were corneal trauma in the CNS group (47.9%) and previous ocular surface disease in the CPS group (31.8%). No significant differences were observed in mean age, sex, previous ocular surface disease, epithelial defect size, and hypopyon between the two groups. Methicillin susceptibility (39.4% vs. 72.7%, p < 0.001) was significantly lower in the CNS group, and poor clinical outcomes (28.0% vs. 43.9%, p = 0.076) were more common in the CPS group. The significant risk factors for poor clinical outcomes were initial best-corrected visual acuity <0.1, epithelial defect size ≥ 5 mm², symptom duration ≥10 days, and hypopyon.
CONCLUSIONS
No significant differences were observed in epidemiological factors and initial clinical characteristics between the two study groups, but predisposing factors and methicillin susceptibility differed between the two groups. Treatment outcomes were relatively worse in the CPS group than in the CNS group, but the difference was not statistically significant. Poor clinical outcomes were more associated with long symptom duration and poor initial clinical characteristics than with coagulase positivity.
MeSH Terms
Figure
Reference
-
1. Savini V. Coagulase-positive and coagulase-negative staphylococci in human disease. In : Fontana C, Favaro M, editors. Pet-to-man travelling staphylococci: a world in progress. 1st ed. Cambridge, Massachusetts: Academic press;2018. chap. 3.2. Needham CA, Stempsey W. Incidence, adherence, and antibiotic resistance of coagulase-negative Staphylococcus species causing human disease. Diagn Microbiol Infect Dis. 1984; 2:293–299.
Article3. Huebner J, Goldmann DA. Coagulase-negative staphylococci: role as pathogens. Annu Rev Med. 1999; 50:223–236.4. Teterycz D, Ferry T, Lew D, et al. Outcome of orthopedic implant infections due to different staphylococci. Int J Infect Dis. 2010; 14:e913–e918.
Article5. Mukerji N, Vajpayee RB, Sharma N. Technique of area measurement of epithelial defects. Cornea. 2003; 22:549–551.
Article6. Thornsberry C. NCCLS standards for antimicrobial susceptibility tests. Lab Med. 1983; 14:549–553.
Article7. Green MD, Apel AJ, Naduvilath T, Stapleton FJ. Clinical outcomes of keratitis. Clin Exp Ophthalmol. 2007; 35:421–426.
Article8. Lichtinger A, Yeung SN, Kim P, et al. Shifting trends in bacterial keratitis in Toronto: an 11-year review. Ophthalmology. 2012; 119:1785–1790.9. Orlans HO, Hornby SJ, Bowler IC. In vitro antibiotic susceptibility patterns of bacterial keratitis isolates in Oxford, UK: a 10-year review. Eye. 2011; 25:489–493.
Article10. Politis M, Wajnsztajn D, Rosin B, et al. Trends of bacterial keratitis culture isolates in Jerusalem; a 13- years analysis. PLoS One. 2016; 11:e0165223.
Article11. Tewari A, Sood N, Vegad MM, Mehta DC. Epidemiological and microbiological profile of infective keratitis in Ahmedabad. Indian J Ophthalmol. 2012; 60:267–272.
Article12. Ng AL, To KK, Choi CC, et al. Predisposing factors, microbial characteristics, and clinical outcome of microbial keratitis in a tertiary centre in Hong Kong: a 10-year experience. J Ophthalmol. 2015; 2015:769436.
Article13. Bourcier T, Thomas F, Borderie V, et al. Bacterial keratitis: predisposing factors, clinical and microbiological review of 300 cases. Br J Ophthalmol. 2003; 87:834–838.
Article14. Schaefer F, Bruttin O, Zografos L, Guex-Crosier Y. Bacterial keratitis: a prospective clinical and microbiological study. Br J Ophthalmol. 2001; 85:842–847.
Article15. Jang YS, Hahn YH. Epidemiology of Staphylococcus epidermidis keratitis. J Korean Ophthalmol Soc. 2002; 43:665–671.16. Graham JE, Moore JE, Jiru X, et al. Ocular pathogen or commensal: a PCR-based study of surface bacterial flora in normal and dry eyes. Invest Ophthalmol Vis Sci. 2007; 48:5616–5623.
Article17. Jeong JG, Kweon EY, Cho NC, You IC. Comparison of methicillin-sensitive staphylococcus epidermidis (MSSE) keratits and methicillin-resistant staphylococcus epidermidis (MRSE) keratitis. J Korean Ophthalmol Soc. 2011; 52:930–935.18. Manikandan P, Bhaskar M, Revathy R, et al. Speciation of coagulase negative Staphylococcus causing bacterial keratitis. Indian J Ophthalmol. 2005; 53:59–60.
Article19. Ong SJ, Huang YC, Tan HY, et al. Staphylococcus aureus keratitis: a review of hospital cases. PLoS One. 2013; 8:e80119.
Article20. Kim BK, Lee DW, Cho NC, You IC. Clinical aspect and prognosis of Staphylococcus epidermidis keratitis. J Korean Ophthalmol Soc. 2011; 52:14–22.21. Kim DN, Park EK. The antimicrobial activity of lysozime against the microorganisms causing conjunctivitis and/or keratitis. J Korean Ophthalmic Opt Soc. 1997; 2:85–90.22. O'Callaghan RJ. The pathogenesis of Staphylococcus aureus eye infections. Pathogens. 2018; 7:E9.23. Wallang BS, Das S, Sharma S, et al. Ring infiltrate in staphylococcal keratitis. J Clin Microbiol. 2013; 51:354–355.24. Saber H, Jasni AS, Jamaluddin TZMT, Ibrahim R. A review of Staphylococcal cassette chromosome mec (SCCmec) types in coagulase-negative staphylococci (CoNS) species. Malays J Med Sci. 2017; 24:7–18.
Article25. Vuong C, Otto M. Staphylococcus epidermidis infections. Microbes infect. 2002; 4:481–489.
Article26. Lowy FD, Hammer SM. Staphylococcus epidermidis infections. Ann Intern Med. 1983; 99:834–839.
Article27. Ekstedt RD, Yotis WW. Studies on staphylococci. II. Effect of coagulase on the virulence of coagulase negative strains. J Bacteriol. 1960; 80:496–500.28. Wu PZ, Zhu H, Thakur A, Willcox MD. Comparison of potential pathogenic traits of staphylococci that may contribute to corneal ulceration and inflammation. Aust N Z J Ophthalmol. 1999; 27:234–236.
Article29. Dajcs JJ, Thibodeaux BA, Girgis DO, O'Callaghan RJ. Corneal virulence of Staphylococcus aureus in an experimental model of keratitis. DNA Cell Biol. 2002; 21:375–382.30. Murray PR, Rosenthal KS, Pfalloer MA. Medical microbiology. Staphylococcus and related gram-positive cocci. 8th ed. Philadelphia: Elsevier;2015. chap. 18.31. Kumar A, Tassopoulos AM, Li Q, Yu FS. Staphylococcus aureus protein A induced inflammatory response in human corneal epithelial cells. Biochem Biophys Res Commun. 2007; 354:955–961.
Article32. Rhem MN, Lech EM, Patti JM, et al. The collagen-binding adhesin is a virulence factor in Staphylococcus aureus keratitis. Infect Immun. 2000; 68:3776–3779.
Article33. Pinna A, Zanetti S, Sotgiu M, et al. Identification and antibiotic susceptibility of coagulase negative staphylococci isolated in corneal/ external infections. Br J Ophthalmol. 1999; 83:771–773.34. Yoon JH, Jung JW, Moon HS, et al. Antibiotics susceptibility in bacterial keratitis and proper initial treatment. J Korean Ophthalmol Soc. 2013; 54:38–45.
Article35. Goldstein MH, Kowalski RP, Gordon YJ. Emerging fluoroquinolone resistance in bacterial keratitis: a 5-year review. Ophthalmology. 1999; 106:1313–1318.36. Alexandrakis G, Alfonso EC, Miller D. Shifting trends in bacterial keratitis in South Florida and emerging resistance to fluoroquinolones. Ophthalmology. 2000; 107:1497–1502.
Article37. Kowalski RP, Dhaliwal DK, Karenchak LM, et al. Gatifloxacin and moxifloxacin: an in vitro susceptibility comparison to levofloxacin, ciprofloxacin, and ofloxacin using bacterial keratitis isolates. Am J Ophthalmol. 2003; 136:500–505.
Article38. Afshari NA, Ma JJ, Duncan SM, et al. Trends in resistance to ciprofloxacin, cefazolin, and gentamicin in the treatment of bacterial keratitis. J Ocul Pharmacol Ther. 2008; 24:217–223.
Article39. Walvick MD, Amato M. Ophthalmic methicillin-resistant Staphylococcus aureus infections: sensitivity and resistance profiles of 234 isolates. J Community Health. 2011; 36:1024–1026.
Article40. Blanco AR, Sudano Roccaro A, Spoto CG, Papa V. Susceptibility of methicillin-resistant staphylococci clinical isolates to netilmicin and other antibiotics commonly used in ophthalmic therapy. Curr Eye Res. 2013; 38:811–816.
Article41. John JF, Harvin AM. History and evolution of antibiotic resistance in coagulase-negative staphylococci: Susceptibility profiles of new anti-staphylococcal agents. Ther Clin Risk Manag. 2007; 3:1143–1152.42. Chavan SP, Jalgaonkar SV, Raut SS, Khadse RK. Clinical and antimicrobial profile of coagulase negative staphylococci in a tertiary care hospital. Int J Res Med Sci. 2017; 5:3420–3425.
Article43. Nayak N, Satpathy G. Slime production as a virulence factor in Staphylococcus epidermidis isolated from bacterial keratitis. Indian J Med Res. 2000; 111:6–10.44. Ahn M, Yoon KC, Ryu SK, et al. Clinical aspects and prognosis of mixed microbial (bacterial and fungal) keratitis. Cornea. 2011; 30:409–413.
Article45. Miedziak AI, Miller MR, Rapuano CJ, et al. Risk factors in microbial keratitis leading to penetrating keratoplasty. Ophthalmology. 1999; 106:1166–1170.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two cases of S. lugdunensis Isolated from Blood and Venous Catheter
- Antibiotic Susceptibilities of Ocular Isolates from Patients with Bacterial Ke ratitis: A Multi-center Study
- Epidemiology of Staphylococcus epidermidis Keratitis
- Epidemiology of infectious Keratitis[I] A Multi-center Study
- Correlation between Sau1 Restriction and Modification Complex Type and Coagulase Serotype or SCCmec Type of Staphylococcus aureus